Affective Disorders and Suicide Risk: A Reexamination
Abstract
OBJECTIVE: In 1970, Guze and Robins published a meta-analysis of suicide in patients with affective illness that inferred a lifetime risk of 15%. Since then, this figure has been generalized to all depressive disorders and cited uncritically in many papers and textbooks. The authors argue for an alternative estimate of suicide risk and question the generalizability of the Guze and Robins estimate. METHOD: The authors sorted studies obtained through a literature search that included data pertaining to suicide occurrence in affective illness into one of three groups: outpatients, inpatients, or suicidal inpatients. Suicide risks were calculated meta-analytically for these three groups, as well as for two previously published collections. RESULTS: There was a hierarchy in suicide risk among patients with affective disorders. The estimate of the lifetime prevalence of suicide in those ever hospitalized for suicidality was 8.6%. For affective disorder patients hospitalized without specification of suicidality, the lifetime risk of suicide was 4.0%. The lifetime suicide prevalence for mixed inpatient/outpatient populations was 2.2%, and for the nonaffectively ill population, it was less than 0.5%. CONCLUSIONS: The percentage of subjects dead due to suicide (case fatality prevalence) is a more appropriate estimate of suicide risk than the percentage of the dead who died by suicide (proportionate mortality prevalence). More important, it is well established that patients with affective disorders suffer a higher risk of suicide relative to the general population. However, no risk factor, including classification of diagnostic subtype, has been reliably shown to predict suicide. This article demonstrates a hierarchy of risk based on the intensity of the treatment setting. Given that patients with a hospitalization history, particularly when suicidal, have a much elevated suicide prevalence over both psychiatric outpatients and nonpatients, the clinical decision to hospitalize in and of itself appears to be a useful indicator of increased suicide risk.
In 1970, Guze and Robins reviewed 17 studies of suicide in patients with primary affective disorder and concluded that 15% of depressed patients would die by suicide (1). In 1990, Goodwin and Jamison reviewed 13 additional studies to replicate the results of Guze and Robins and concluded that 18.9% of depressed patients would die by suicide (2). The methodologies of these two reviews were similar, containing the same assumptions as well as the same biases. We note three points of particular interest. First, both reviews considered studies that consisted almost exclusively of hospitalized patients. Second, both reviews calculated proportionate mortality (the percentage of the dead who died by suicide) rather than case fatality (the percentage of the original sample who died by suicide). Third, most of the studies included in both estimates of lifetime suicide risk had follow-up periods of only a few years. We shall show how these three issues distort the interpretation of the actual risk of suicide in patients with affective disorders.
Even though both reviews considered studies that almost exclusively consisted of hospitalized populations, subsequent authors, all citing Guze and Robins, have generalized their 15% figure to populations neither Guze and Robins (1) nor Goodwin and Jamison (2) considered. Following this convention, major American textbooks continue to report the 15% figure as correct for all depressed patients (3–7). Moreover, “depression” is no longer defined as it was in 1970. Subsequent editions of DSM have made the diagnosis of a major depressive episode more inclusive. Today up to 20% of the population meet criteria for a watered-down, broad, and, ultimately, a less lethal depressive diagnosis. Klein and Thase (8) made this point powerfully when they observed that in 1972, the lifetime prevalence of depression in the American population in DSM-II terms was 2%–3%, when the definition of depression included only involutional melancholia, the unipolar form of manic depression, psychotic depression, and “severe depressive neuroses.” By 1994, under the rubric of DSM-IV, the lifetime prevalence of depression had increased to 10%–20%. The major difference between 1972 and 1999 is not that we are caught in an affective epidemic. “Much broader and more inclusive definitions of mood disturbance, with major differences in thresholds for ‘clinical depression’ and when we recommend treatment” are the explanation (9). Today, many more people carry a depressive label, but the incidence of the severe forms remains relatively low.
The psychiatric literature and textbooks do not alert readers to this diagnostic shift. Extrapolations of studies of the most severely ill are now wrongly applied to all patients with a depressive diagnosis of any sort. Examples that such generalizations are inappropriate are easily found. For instance, Helgason (10) followed a cohort of Icelanders for 61 years and found that 7.2% of the patients with affective disorder died as a result of suicide. When the cohort was split into two groups, one psychotic and one neurotic, the suicide rates bifurcated (patients with primarily psychotic depression: 14.5%; patients with primarily neurotic depression: 1.8%).
Both of the previous reviews (1, 2) employed proportionate mortality to estimate suicide rates in affective disorder patients. Proportionate mortality is a conditional quantity that represents the probability that a subject will have died as a result of suicide, given that the subject has died during the follow-up period. If all of the subjects in every study were followed throughout their lifespan, proportionate mortality would correctly estimate the probability of suicide. However, if subjects are not followed for their entire lives, proportionate mortality will overestimate the risk of suicide, particularly since suicide is overrepresented as a cause of death among younger persons (11).
This leads to the third limitation of the results obtained by the two previous reviews (1, 2). Their suicide rates were estimated from studies of hospitalized patients that had varying, and frequently brief, lengths of follow-up after discharge. Because suicide is known to occur at the highest rates soon after hospitalization and early in the course of diagnosed illness, subjects who die in studies with short follow-up periods are more likely to die from suicide than any other cause. Therefore, in short studies proportionate mortality will greatly overestimate the lifetime risk of suicide. We therefore challenge the use of the proportionate mortality estimate as a measure of suicide risk and propose the use of case fatality rates as a more realistic alternative.
The two previous reviews both tell us something about the sickest psychiatric patients, i.e., those mentally ill enough to require hospitalization. But these “highly selected” populations yield results “unlikely to be generally applicable to all patients suffering from the particular disease” (12). We dispute the generalizability of the findings of the earlier meta-analyses (1, 2) to affectively ill populations other than depressed inpatients and outline a hierarchical model of assigning suicide risk to patients with affective disorders.
Method
Our reexamination began with a reanalysis of the data in the 17 studies included in the meta-analysis of Guze and Robins (1). For each study, we compared both proportionate mortality and case fatality. The additional 13 studies that Goodwin and Jamison (2) used to confirm the findings of Guze and Robins (1) were also reanalyzed. We also conducted a computer search of the MEDLINE (1966–present) and PsycINFO (1984–present) databases and reviewed the bibliographies of relevant psychiatry textbook chapters, studies, and review articles to identify additional studies. The search was limited to English-language studies.
The purpose of our study was to reassess the lifetime prevalence of suicide in patients with affective disorders. All studies analyzed in this article are, by definition, survivorship studies, and most are observational rather than randomized and controlled. O’Brien and Shampo (13) stated that “in every study of survivorship, the first requirement is to describe the group studied.” Thus, we have only included those reports containing a minimum data set that summarized the number of suicides and deaths among a cohort of affectively ill patients. Each included study plainly indicated whether the subjects at the inception of the investigation were inpatients, outpatients, or a mixture of both.
We chose the general and inclusive term “affective disorders” because it encompasses the incongruence among investigators (12) as well as the definitional heterogeneity bred over the past several decades by the evolution of classification systems such as DSM and ICD. Many studies predated or ignored these systems. The jumble of terms for affective disorders included manic depression, bipolar depression, neurotic depression, nonpsychotic depression, reactive depression, endogenous depression, neurosis, involutional melancholia, unipolar depression, primary depression, secondary depression, and affective psychosis. Adding to the confusion was the fact that some authors are of the opinion that the presence of endogenous features, rather than depressive subtype, determines suicide rates (14, 15).
Over 30 years ago, Silverman (16) determined that suicide in depressed patients was not clearly associated with the presence or absence of physical symptoms, diagnostic subtype, psychosis, or treatment modality. The search for definitive suicide risk factors, detailed in hundreds, if not thousands, of papers, remains inconclusive. Among psychotropic medications, only lithium has been found to reduce the incidence of suicide (17) and then only after patients have reliably taken it for at least 2 years (18).
This study scrutinized each population’s treatment status, since we hypothesized that different patient statuses have different suicide rates. First, we confirmed that the studies included in the two previous reviews (1, 2) almost exclusively contained inpatient subjects. As new studies were identified, we took special pains to distinguish how patients were classified for comparison purposes. The new studies of affective disorder patients were sorted into two inpatient categories and one outpatient category on the basis of how the authors classified patient status at study commencement (19). The first inpatient category was undifferentiated according to suicidality; the second comprised patients hospitalized after suicidal ideation or attempt.
After noting treatment status, we restricted the studies accepted by excluding studies that did not have a mean follow-up time of at least 2 years, since the incidence of suicide is elevated in the first 2 years after hospitalization (20–23). In addition, all studies included had to have at least a 90% rate of follow-up. This restriction was based on the common sense presumption that the larger the number of original subjects unaccounted for, the greater the number who may have been lost to a condition like suicide (11, 24). As more subjects are lost to follow-up, more questions must be raised about what happened to them and what conclusions can be drawn with confidence from the remaining data (25).
While we took great pains to obtain the cleanest collection of studies possible, several problems presented themselves. First, the suicidal inpatient category contained mixed diagnoses, since only two of the studies specifically excluded all but affective disorder patients. Second, few outpatient studies could meet our initial rigid inclusion criteria. Most studies began with a mix of patients from a variety of psychiatric services, including inpatient, outpatient, emergency room, and day hospital. In one study, 54% had a history of prior hospitalization, and 86% had been hospitalized at least once during the 5-year follow-up period (26). The largest American study of mortality in psychiatric “outpatients,” Morrison’s San Diego study of 12,000 patients, was, in fact, a report of a mixed group (27). More than 40% of these so-called “outpatients” had at least one hospitalization during the 8.5 years of the study (J.R. Morrison, personal communication, 1999). As a result, we relaxed the outpatient category criteria to include studies in which at least two-thirds of the subjects were nominal outpatients at the starting point.
Another potential limitation of this study, and of the two previous reviews (1, 2) as well, arises from the failure to consider additional factors that may influence suicide risk. For instance, while the discrepancy between male and female suicide rates in the general population is significantly narrowed in the psychiatric population, it is not completely erased (28). While some studies distinguished between the sexes, others simply provided the number of patients followed. Other potential risk factors surely exist for which data are not generally available. These may include rehospitalization, treatment modalities, employment, age, race, country, or any of the myriad other factors that can be used to characterize populations.
Like the two previous reviews (1, 2), our study used a small set of variables from each study to examine the risk of suicide in affective disorder patients. Our data analysis considered only the number of patients, the number of deaths, and the number of suicides in each of the studies we analyzed. It would have been preferable to collect the survival status and length of follow-up for each subject, but those data were not universally available. Our analysis included as suicides only those deaths classified specifically as such and excluded accidental deaths, “quasi-suicides,” and other categories of ambiguous deaths. This narrow suicide definition only slightly diminishes suicide counts. Coroners over the last century have been shown to apply consistent standards to suicide classification (29) and to underestimate suicide by exclusion of accidental deaths and the like at a consistent rate of 15%–20% (30).
Like the two previous reviews (1, 2), ours is a meta-analysis, an approach “developed as a way to summarize the results of different research studies of related problems” (31). Admittedly, many difficulties arise when dealing with data from such studies. The studies themselves do not fully reflect the situation in the population at large (32–36). Further, the various studies differ in their aims and in their execution (37). While it was impossible to completely overcome these limitations, we were able to minimize their impact by carefully delineating the terms and conditions for inclusion.
Statistical methods can compensate for the remaining heterogeneity. These methods are often referred to as “random effects models” (38) as opposed to “fixed effects models,” which do not account for study-to-study variability. The idea behind random effects techniques is that some universal set of studies exists, from which the observed studies are randomly drawn. This construct has the effect of ascribing study-to-study variability to this unobserved sampling mechanism. The global estimates of probabilities or averages obtained by using random effects models are usually approximately equal to the quantities that are calculated by using traditional techniques. However, the variance estimates are larger, which reflects the additional study-to-study variability.
In this article, we calculated four distinct probability estimates for each of five different populations of psychiatric patients (affective disorder outpatients, affective disorder inpatients, suicidal inpatients, and the hospitalized affective disorder patients from the two previous meta-analyses [1, 2]). The first probability estimate is the “case fatality prevalence,” or the probability that a subject will die by suicide during the course of the study. Within a single study, this can be estimated by dividing the number of suicides by the number of subjects. The second probability is the “proportionate mortality prevalence,” or the probability that a subject will die as a result of suicide given that the subject will die during the course of the study. This corresponds to the rates used in the two previous meta-analyses (1, 2). For a single study, this can be estimated by dividing the number of suicides by the number of deaths. The third probability represents the “general mortality prevalence,” or the probability that a subject will die of any cause during follow-up. For a single study, this probability can be estimated by the ratio of total deaths to total subjects. The fourth probability is a projection of what the suicide mortality would be if all subjects were followed until death. It is obtained by an application of Bayes’s Rule, which states that the probability of suicide is equal to the probability of suicide, given death, times the probability of death (39).
Each of the first three probabilities, and its 95% confidence interval, was calculated by using the generalized estimating equations (40) capabilities found in PROC GENMOD, a part of the SAS statistical package (41). The suicide mortality estimate was calculated as the product of the proportionate mortality prevalence and the general mortality prevalence. In addition to obtaining probability estimates, pair-wise comparisons among the various mortality prevalence estimates were performed, again by using PROC GENMOD.
Results
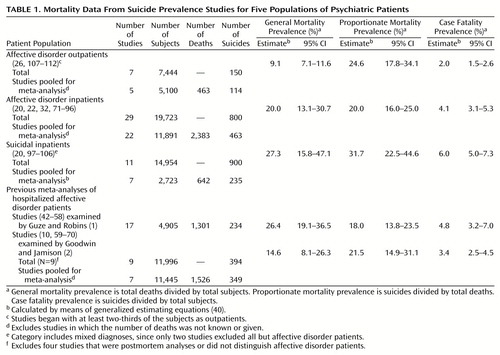
Table 1 summarizes the data obtained from the studies belonging to each of our five populations of psychiatric patients. One group reflects the 17 studies (42–58) originally examined by Guze and Robins (1). Another represents the 13 studies (10, 59–70) in Goodwin and Jamison’s review (2). The other three groups were those we identified for this study. Twenty-nine studies (20, 22, 32, 71–96) met inclusion criteria for the “affective disorder inpatients” category. Eleven studies (20, 97–106) focused specifically on inpatients hospitalized after a suicide attempt or ideation. Seven studies of affective disorder patients (26, 107–112) began with at least two-thirds of the subjects as outpatients. The information recorded for each group of studies includes the number of studies that could be pooled in our meta-analysis as well as the total number of subjects, deaths, and suicides in each collection of pooled studies. It also contains the random effects estimates of the general mortality prevalence, proportionate mortality prevalence, and case fatality prevalence rates, along with corresponding 95% confidence intervals (CIs).
The group-wide general mortality estimates varied from 9.1% to 27.3% among the different populations of psychiatric patients. The estimates of proportionate mortality ranged from 18.0% to 24.6% for four of the groups, with that for suicidal inpatients equal to 31.7%. The case fatality estimates were considerably smaller, ranging from 2.0% for affective disorder outpatients to 6.0% for suicidal inpatients. The case fatality estimates nearly matched the final estimates of suicide risk we obtained by applying Bayes’s Rule to the probability estimates obtained from the random effects models (Figure 1).
The case fatality rates of all of the three populations of psychiatric patients for which we identified new studies were significantly different from one another. The case fatality prevalence of affective disorder inpatients significantly differed from that of both suicidal inpatients (χ2=5.40, df=1, p=0.02) and affective disorder outpatients (χ2=12.87, df=1, p=0.0003). Also, the case fatality prevalence of the affective disorder outpatients and the suicidal inpatients significantly differed (χ2=43.84, df=1, p<0.0001). As we expected, the earlier studies collected by Guze and Robins (1) and Goodwin and Jamison (2) were most similar to our new collection of studies of affective disorder inpatients. The case fatality prevalence from Guze and Robins was significantly different from that of our affective disorder outpatients (χ2=12.73, df=1, p=0.0004) but was not statistically different from that of Goodwin and Jamison (χ2=1.91, df=1, p<0.17) or from our affective disorder (χ2=0.42, df=1, p<0.52) or suicidal (χ2=1.15, df=1, p<0.29) inpatients. While not different from that of Guze and Robins (1), the case fatality prevalence from Goodwin and Jamison (2) significantly differed from those of both affective disorder outpatients (χ2=6.36, df=1, p<0.02) and suicidal inpatients (χ2=10.58, df=1, p<0.002). These results support our hypothesis that suicide risk is hierarchical among the affectively ill.
Discussion
This study was a meta-analysis that drew upon data pooled from diverse sources. Even with the crudeness of the data, however, two points emerge robustly. First, case fatality rates are a better measure of suicide risk than proportionate mortality rates. Second, lifetime suicide prevalence sorts out in a stair-step hierarchy of increasing risk according to treatment history (Figure 1).
We are not the first to argue that case fatality rates describe suicide risk better than proportionate mortality rates. In a 1968 American Journal of Psychiatry review on the epidemiology of depression (16), Silverman roundly criticized the use of proportionate mortality to describe suicide risk in an earlier meta-analysis of Robins and associates (113).
The proportionate mortality measure reflects only the percentage of suicides among those who died during the study, and that is its weakness. It estimates a conditional probability: the risk of a suicide should death occur during the study. It cannot approximate the actual risk of suicide unless at least one of two conditions is met: either all of the subjects under observation are followed until they die or suicides occur at the same rate relative to the total number of deaths.
The first of these conditions is difficult to meet. Many subjects in a given study are likely to outlive the career of a single researcher. For instance, Helgason’s 1979 paper followed a cohort for 61 years (10), and almost one-half of the cohort was still alive at the end of this extensive follow-up period.
The second requirement does not fit what we know about suicide epidemiology. Suicide is overrepresented in youthful populations (11). Further, numerous researchers have demonstrated that suicide occurs variably at different points in the natural course of affective illness (20, 23, 114–117). It is evident that suicide risk decreases as the time from the most recent hospitalization, or treatment, increases (20, 114–116, 118). Also, suicide risk is highest during the years immediately following the onset of affective disorders (23, 117, 119).
Because the risk of suicide is not constant across the history of affective disease, proportionate mortality must provide a biased estimate of suicide risk. This is particularly true for studies with a short length of follow-up in which very few patients have yet died from any cause. With suicide concentrated in the first months after discharge, and in the early stages of disease, it will be disproportionately represented in a suicide-to-death ratio. This is reflected in the results of the studies we examined. Studies with a short length of follow-up produced estimates of proportionate mortality that were very high. In fact, the proportionate mortality prevalence estimates from two studies, one with a mean follow-up of 3.2 years (76) and one with a mean follow-up of 0.5 years (44), were equal to 100% (44, 76). Case fatality estimates do not suffer from this bias, since they allow individuals who have not yet died to provide information concerning the probability of suicide during follow-up. Of course, we must acknowledge that case fatality prevalence will underestimate the lifetime rate of suicide by missing future suicides. However, proportionate mortality prevalence misses not only future suicides but also future deaths. As suicides tend to occur at a higher rate soon after diagnosis or treatment, the bias in case fatality estimates is sure to be smaller than the bias incurred by using proportionate mortality prevalence to estimate lifetime suicide risk.
As a final evaluation of the appropriateness of case fatality and proportionate mortality methods, consider the results presented in Table 1 and Figure 1. The case fatality prevalence estimates are quite close to our final estimates of suicide risk, while the proportionate mortality prevalence estimates are much higher. While neither proportionate mortality prevalence nor case fatality prevalence is a perfect estimate of suicide risk, from this combined evidence, it would appear that case fatality is better.
If case fatality rates are used to approximate suicide risk, a hierarchical layering of suicide risk becomes apparent. The results in Table 1 suggest, and pair-wise comparisons verify, that suicide prevalence differs according to treatment history. Those who are not psychiatric patients have the lowest risk. Psychiatric outpatients have a higher risk, but it is not so great as that of psychiatric inpatients. In turn, psychiatric inpatients who are suicidal have the highest risk. While we must recognize that only two of the 11 studies of suicidal inpatients specifically concerned affective disorder patients, these had two of the four highest case fatality prevalences, at 9.2% (99) and 15.2% (104). This points to greater lethality in the affective subgroup. Clinical judgment about the level of treatment intensity required appears to predict suicide prevalence.
Others before us have recognized this hierarchy. Black and Winokur (120) asserted that hospitalized psychiatric patients form “a special subgroup” whose elevated death risk early after discharge “may not be generalizable.” Moreover, Kiloh and colleagues (88) found that in the long-term outcome of depressive illness, “few factors apart from prior hospital admission seem to be of prognostic importance.” A number of studies that included one or more types of psychiatric patients, as well as nonpsychiatric subjects, provided further evidence that our proposed hierarchy is correct (10, 34, 67, 121, 122). These studies consistently demonstrate that those who are deemed to be the most severely ill at baseline are at the greatest risk for suicide. They complement the finding of VanGastel and colleagues (123), who reported that both suicidal ideation and attempt are directly related to the severity of depression.
Given that a suicide risk hierarchy is present, we now recall that the studies included in the meta-analyses of both Guze and Robins (1) and Goodwin and Jamison (2) almost exclusively consisted of inpatients. Subsequent authors, including those in most major English-language textbooks, who have referenced the seminal Guze and Robins meta-analysis, have extrapolated the results to all patients with affective disorders. In most cases they have failed to acknowledge the preponderance of inpatients in the original studies. This consequent bias cannot be ignored. The case fatality prevalence estimates from the two previous meta-analyses compared favorably to that from our newly gathered inpatient collection but differed from those of outpatients. Additionally, Goodwin and Jamison’s case fatality prevalence was significantly different from the case fatality prevalence obtained from studies that examined suicidal inpatients. We emphasize that the results of the two previous meta-analyses are applicable only to patients with affective disorders who have been hospitalized without specification of suicidality.
If hospitalized depressed patients are at greater risk of suicide, what then determines which ones are hospitalized? Rather than depression itself, it is the threat of suicide that usually decides which patients are offered—or forced to accept—admission (9, 23). The severity of depression and, hence, the degree of suicidality, may be driven by specific factors occurring along with the core depressive syndrome. These include substance abuse or dependence in the patient or first-degree relatives, anxiety (particularly the malignant anguish or “psychache” described by Shneidman [124]), impulsivity, aggressivity, and family history of affective illness, suicide, or suicide attempts (125). Hopelessness is pervasive in suicidal states (126). Goldney and colleagues (127) found that the patients in a series who died as a result of suicide after psychiatric hospitalization had more and longer hospitalizations, more previous suicide attempts, more overt depression, and more neuroleptic use. All these factors, rather than specific indicia of affective disease, will likely enter into the clinical judgment and result in some patients being admitted to the hospital while others are treated in less restrictive settings.
In summary, the case fatality method gives a more accurate accounting of suicide prevalence than the proportionate mortality method. This is because suicide risk in affective disorders concentrates early in the course of illness and soon after hospital discharge. Case fatality rates are different among groups of affective disorder patients, defined by history of treatment and suicidality. Those recently hospitalized with a suicide attempt or suicidal ideation are at highest risk. Those recently hospitalized for any psychiatric reason have the next highest risk. Psychiatric outpatients are at lower risk than inpatients but are at higher risk than those in the general population who do not carry an affective diagnosis. From a public health perspective, suicide prevention efforts should thus be focused on recently or repeatedly hospitalized patients, especially the suicidal ones. In the absence of other compelling data, it may be reasonable to relax concern somewhat as the length of time from the last hospitalization or suicidal state increases for any given patient.
 |
Received Nov. 10, 1999; revision received May 24, 2000; accepted June 9, 2000. From the Department of Psychiatry and Psychology and the Department of Health Sciences Research, Mayo Clinic. Address reprint requests to Dr. Bostwick, Department of Psychiatry and Psychology, Mayo Clinic, 200 First St., S.W., Rochester, MN 55905; [email protected] (e-mail).The authors thank Sara Van Scoy, M.D., as well as the library staff at Wilford Hall Medical Center, Lackland Air Force Base, Lackland, Tex., for their assistance in identifying and locating studies included in the literature review.
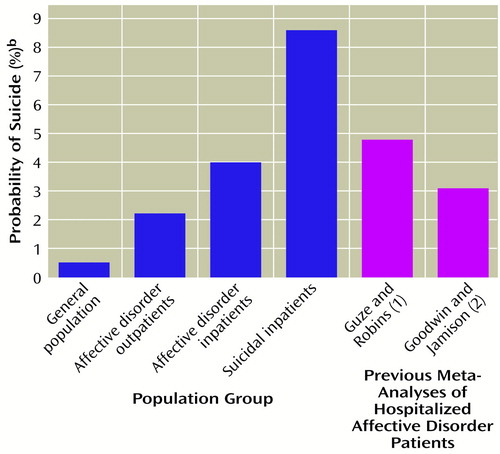
Figure 1. Lifetime Risk of Suicide Among Five Populations of Psychiatric Patientsa
aSee Table 1 for studies that comprised the patient populations.
bDetermined by application of Bayes’s Rule (39), which states that the probability of suicide is equal to the probability of suicide given death (proportionate mortality prevalence) times the probability of death (general mortality prevalence).
1. Guze SB, Robins E: Suicide and primary affective disorders. Br J Psychiatry 1970; 117:437–438Crossref, Medline, Google Scholar
2. Goodwin FK, Jamison KR: Suicide, in Manic-Depressive Illness. New York, Oxford University Press, 1990, pp 227–244Google Scholar
3. Klerman GL: Depression and related disorders of mood, in The New Harvard Guide to Psychiatry. Edited by Nicholi AM. Cambridge, Mass, Belknap Press, 1988, p 319Google Scholar
4. Davidson L: Suicide and aggression in the medical setting, in The Psychiatric Care of the Medical Patient. Edited by Stoudemire A, Fogel BS. New York, Oxford University Press, 1993, pp 71–72Google Scholar
5. Andreasen NC, Black DW: Suicide and violent behavior, in Introductory Textbook of Psychiatry. Washington, DC, American Psychiatric Press, 1995, p 514Google Scholar
6. Roy A: Psychiatric emergencies, in Comprehensive Textbook of Psychiatry, 6th ed. Edited by Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1995, p 1744Google Scholar
7. Dubovsky SI, Buzan R: Mood disorders, in The American Psychiatric Press Textbook of Psychiatry, 3rd ed. Edited by Hales RE, Yudofsky SC, Talbott JA. Washington, DC, American Psychiatric Press, 1999, p 480Google Scholar
8. Klein DF, Thase M: Medication versus psychotherapy for depression. Progress Notes (American Society of Clinical Psychopharmacology) 1997; 8:41–47Google Scholar
9. Blair-West GW, Mellsop GW, Eyeson-Annan ML: Down-rating lifetime suicide risk in major depression. Acta Psychiatr Scand 1997; 95:259–263Crossref, Medline, Google Scholar
10. Helgason T: Epidemiological investigations concerning affective disorders, in Origin, Prevention, and Treatment of Affective Disorders. Edited by Schou M, Strõmgren E. London, Academic Press, 1979, pp 241–255Google Scholar
11. Inskip HM, Harris EC, Barraclough B: Lifetime risk of suicide for affective disorder, alcoholism, and schizophrenia. Br J Psychiatry 1998; 172:35–37Crossref, Medline, Google Scholar
12. Stenager EN, Stenager E: Suicide and patients with neurologic diseases: methodologic problems. Arch Neurol 1992; 49:1296–1303Google Scholar
13. O’Brien PC, Shampo MA: Survivorship studies. Mayo Clin Proc 1981; 56:709–711Medline, Google Scholar
14. Black DW, Winokur G, Nasrallah A: Suicide in major subtypes of affective disorder. Arch Gen Psychiatry 1987; 44:878–880Crossref, Medline, Google Scholar
15. Duggan CF, Lee AS, Murray RM: Do different subtypes of hospitalized depressives have different long-term outcomes? Arch Gen Psychiatry 1991; 48:308–312Google Scholar
16. Silverman C: The epidemiology of depression—a review. Am J Psychiatry 1968; 124:883–891Link, Google Scholar
17. Tondo L, Jamison KR, Baldessarini RJ: Effect of lithium maintenance on suicidal behavior in major mood disorders. Ann NY Acad Sci 1997; 836:339–351Crossref, Medline, Google Scholar
18. Ahrens B, Mûller-Oerlinghausen B, Grof P: Length of lithium treatment needed to eliminate the high mortality of affective disorders. Br J Psychiatry Suppl 1993; 21:27–29Medline, Google Scholar
19. Lagakos S: Statistical analysis of survival data, in Medical Uses of Statistics, 2nd ed. Edited by Bailar JC, Mosteller F. Boston, NEJM Books, 1992, pp 281–291Google Scholar
20. Pokorny AD: Prediction of suicide in psychiatric patients. Arch Gen Psychiatry 1983; 40:249–257Crossref, Medline, Google Scholar
21. Black DW, Warrack G, Winokur G: Excess mortality among psychiatric patients. JAMA 1985; 253:58–61Crossref, Medline, Google Scholar
22. Buchholtz-Hansen PE, Wang AG, Kragh-Sorenson P: Mortality in major affective disorder: relationship to subtype of depression. Acta Psychiatr Scand 1993; 87:329–335Crossref, Medline, Google Scholar
23. Malone KM, Haas GL, Sweeney JA, Mann JJ: Major depression and the risk of attempted suicide. J Affect Disord 1995; 34:173–185Crossref, Medline, Google Scholar
24. Sims AC: Importance of a high tracing rate in long-term medical follow-up studies. Lancet 1973; 2:433–435Crossref, Medline, Google Scholar
25. Everitt BS: Analysis of longitudinal data. Br J Psychiatry 1998; 172:7–10Crossref, Medline, Google Scholar
26. Pederson AM, Barry DJ, Babigian HM: Epidemiological considerations of psychotic depression. Arch Gen Psychiatry 1972; 193–197Google Scholar
27. Morrison JR: Suicide in a psychiatric practice population. J Clin Psychiatry 1982; 43:348–352Medline, Google Scholar
28. Jamison KR: Suicide and bipolar disorders. Ann NY Acad Sci 1986; 487:301–315Crossref, Medline, Google Scholar
29. Sainsbury P, Jenkins JS: The accuracy of officially reported statistics for purposes of epidemiological research. J Epidemiol Community Health 1982; 36:43–48Crossref, Medline, Google Scholar
30. Speechley M, Stavraky KM: The adequacy of suicide statistics for use in epidemiology and public health. Can J Public Health 1991; 82:38–42Medline, Google Scholar
31. Bailar JC: The promise and problems of meta-analysis. N Engl J Med 1997; 337:559–561Crossref, Medline, Google Scholar
32. Angst J: Course of affective disorder, in Brain Mechanisms and Abnormal Behavior. Edited by van Praag HM, Lader MH, Rafaelson OJ. New York, Marcel Dekker, 1981, pp 225–242Google Scholar
33. Koranyi EK: Fatalities in 2,070 psychiatric outpatients. Arch Gen Psychiatry 1977; 34:1137–1142Google Scholar
34. Babigian HM, Odoroff CL: The mortality experience of a population with psychiatric illness. Am J Psychiatry 1969; 126:470–480Link, Google Scholar
35. Rich CL, Young D, Fowler RC: San Diego Suicide Study, I: young versus old subjects. Arch Gen Psychiatry 1986; 43:577–582Crossref, Medline, Google Scholar
36. Eaton WW: Studying the natural history of psychopathology, in Textbook in Psychiatric Epidemiology. Edited by Tsuang MT, Tohen M, Zahner GEP. New York, Wiley-Liss, 1995, pp 157–177Google Scholar
37. Martin RL: Methodological and conceptual problems in the study of mortality in psychiatry. Psychiatr Dev 1985; 4:317–333Google Scholar
38. Fleiss JL: The statistical basis of meta-analysis. Stat Methods Med Res 1993; 2:121–145Crossref, Medline, Google Scholar
39. Rosner B: Fundamentals of Biostatistics, 4th ed. Pacific Grove, Calif, Duxbury, 1995Google Scholar
40. Diggle PJ, Liang KY, Zeger SL: Analysis of Longitudinal Data. Oxford, UK, Oxford University Press, 1994Google Scholar
41. SAS/STAT User’s Guide, version 6.12. Cary, NC, SAS Institute, 1990Google Scholar
42. Ziskind E, Somerfeld-Ziskind E, Ziskind L: Metrazol and electric convulsive therapy of the affective psychoses. Arch Neurol Psychiatry 1945; 53:212–217Crossref, Google Scholar
43. Huston PE, Locher LM: Involutional psychosis: course when untreated and treated with electric shock. Arch Neurol Psychiatry 1948; 59:385–394Crossref, Medline, Google Scholar
44. Seager CP: Controlled trial of straight and modified electroplexy. J Ment Sci 1959; 105:1022–1028Google Scholar
45. Helgason T: Epidemiology of mental disorders in Iceland: a psychiatric and demographic investigation of 5,395 Icelanders. Acta Psychiatr Scand Suppl 1964; 173:1–258Google Scholar
46. Fremming KH: The Expectation of Mental Infirmity in a Sample of the Danish Population: Occasional Papers in Eugenics 7. London, Cassell, 1951Google Scholar
47. Bond ED, Braceland FJ: Prognosis in mental disease: the use of one-page abstracts. Am J Psychiatry 1937; 94:263–274Link, Google Scholar
48. Huston PE, Locher LM: Manic-depressive psychosis: course when untreated and treated with electric shock. Arch Neurol Psychiatry 1948; 60:37–48Crossref, Medline, Google Scholar
49. Hastings DW: Follow-up results in psychiatric illness. Am J Psychiatry 1958; 114:1057–1066Google Scholar
50. Watts CAH: The incidence and prognosis of endogenous depression. Br Med J 1956; 1:1392–1397Google Scholar
51. Astrup C, Fossum A, Holmboe R: A follow-up study of 270 patients with acute affective psychoses. Acta Psychiatr Scand Suppl 1959; 135:1–65Google Scholar
52. Pitts FN, Winokur G: Affective disorder, III: diagnostic correlates and incidence of suicide. J Nerv Ment Dis 1964; 139:176–181Crossref, Medline, Google Scholar
53. Langelûddecke A: Ûber Lebenserwartung und Rûckfallhaufigkeit bei Manisch-Depressiven. Z Psych Hyg 1941; 14:1–15Google Scholar
54. Slater E: Zur Erbpathologie des Manische-Depressive Irreseins: die Eltern und Kinder von Manische-Depressiven. Z Neurol Psychiatr 1938; 163:1–47Crossref, Google Scholar
55. Stenstedt A: Study in manic-depressive psychosis: clinical, social, and genetic investigations. Acta Psychiatr Neurol Scand Suppl 1952; 79:1–111Google Scholar
56. Lundquist G: Prognosis and course in manic-depressive psychoses: a follow-up study of 319 first admissions. Acta Psychiatr Neurol Scand Suppl 1945; 35:1–96Google Scholar
57. Schulz B: Sterblichkeit endogen Geisteskranker und ihrer Eltern. Z Menschl Vererb Konstitutions Lehre 1949; 29:338–367Google Scholar
58. Bratfos O, Haug JO: The course of manic-depressive psychosis: a follow-up investigation of 215 patients. Acta Psychiatr Scand 1968; 44:89–112Crossref, Medline, Google Scholar
59. Perris C, d’Elia G: A study of bipolar (manic-depressive) and unipolar recurrent depressive psychoses. Acta Psychiatr Scand 1966; 194:172–189Crossref, Google Scholar
60. Barraclough B: Suicide prevention, recurrent affective disorder and lithium (abstract). Br J Psychiatry 1972; 121:391–392Crossref, Medline, Google Scholar
61. Taschev T: The course and prognosis of depression on the basis of 652 patients deceased, in Classification and Prediction of the Outcome of Depression: Symposium Schloss Reinhartshausen/Rhein, Symposia Medica Hoechst 8. Edited by Angst J. Stuttgart, Germany, FK Schattauer, 1974, pp 157–172Google Scholar
62. James NM, Chapman CJ: A genetic study of bipolar affective disorder. Br J Psychiatry 1975; 126:449–456Crossref, Medline, Google Scholar
63. Winokur G, Tsuang M: The Iowa 500: suicide in mania, depression, and schizophrenia. Am J Psychiatry 1975; 132:650–651Link, Google Scholar
64. Tsuang MT: Suicide in schizophrenics, manics, depressives, and surgical controls. Arch Gen Psychiatry 1978; 35:153–155Crossref, Medline, Google Scholar
65. Dunner DL, Gershon ES, Goodwin FK: Heritable factors in the severity of affective illness. Biol Psychiatry 1976; 11:31–42Medline, Google Scholar
66. Weeke A: Causes of death in manic-depressives, in Origin, Prevention and Treatment of Affective disorders. Edited by Schou M, Strõmgren E. London, Academic Press, 1979, pp 289–299Google Scholar
67. Hagnell O, Lanke J, Rorsman B: Suicide rates in the Lundby study: mental illness as a risk factor for suicide. Neuropsychobiology 1981; 7:248–253Crossref, Medline, Google Scholar
68. Egeland JA, Sussex JN: Suicide and family loading in affective disorders. JAMA 1985; 254:915–918Crossref, Medline, Google Scholar
69. Black DW, Winokur G, Nasrallah A: Is death from natural causes still excessive in psychiatric patients? a follow-up of 1,593 patients with major affective disorder. J Nerv Ment Dis 1987; 175:674–680Crossref, Medline, Google Scholar
70. Angst J: Suicides among depressive and bipolar patients, in 1998 Annual Meeting Syllabus and Proceedings Summary. Washington, DC, American Psychiatric Association, 1998Google Scholar
71. Lewis AJ: Prognosis in the manic-depressive psychoses. Lancet 1936; 2:997–999Crossref, Google Scholar
72. Rennie TAC: Prognosis in manic-depressive psychoses. Am J Psychiatry 1942; 98:801–814Link, Google Scholar
73. Ciompi L: Follow-up studies on the evolution of former neurotic and depressive states in old age: clinical and psychodynamic aspects. J Geriatr Psychiatry 1969; 3:90–106Google Scholar
74. Post F: The management and nature of depressive illnesses in late life: a follow-through study. Br J Psychiatry 1972; 121:393–404Crossref, Medline, Google Scholar
75. Prien RF, Klett CJ, Caffey EM: Lithium carbonate and imipramine in prevention of affective episodes. Arch Gen Psychiatry 1973; 29:420–425Crossref, Medline, Google Scholar
76. Carlson GA, Kotin J, Davenport YB, Adland M: Follow-up of 53 bipolar manic-depressive patients. Br J Psychiatry 1974; 124:134–139Crossref, Medline, Google Scholar
77. Avery D, Winokur G: Mortality in depressed patients treated with electroconvulsive therapy and antidepressants. Arch Gen Psychiatry 1976; 33:1029–1037Google Scholar
78. Sims A, Prior P: The pattern of mortality in severe neuroses. Br J Psychiatry 1978; 133:299–305Crossref, Medline, Google Scholar
79. Tsuang MT, Woolson RF: Excess mortality in schizophrenia and affective disorders. Arch Gen Psychiatry 1978; 35:1181–1185Google Scholar
80. Whitlock FA, Siskind M: Depression and cancer: a follow-up study. Psychol Med 1979; 9:747–752Crossref, Medline, Google Scholar
81. Copeland JRM: Psychotic and neurotic depression: discriminant function analysis and five-year outcome. Psychol Med 1983; 13:373–383Crossref, Medline, Google Scholar
82. Weeke A, Vaeth M: Excess mortality of bipolar and unipolar manic-depressive patients. J Affect Disord 1986; 11:227–234Crossref, Medline, Google Scholar
83. Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W: Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry 1987; 144:35–40Link, Google Scholar
84. Berglund M, Smith GJW: Post-diction of suicide in a group of depressive patients. Acta Psychiatr Scand 1988; 77:504–510Crossref, Medline, Google Scholar
85. Berglund M, Nilsson K: Mortality in severe depression. Acta Psychiatr Scand 1987; 76:372–380Crossref, Medline, Google Scholar
86. Black DW, Winokur G, Nasrallah A: Effect of psychosis on suicide risk in 1,593 patients with unipolar and bipolar affective disorders. Am J Psychiatry 1988; 145:849–852Link, Google Scholar
87. Lee AS, Murray RM: The long-term outcome of Maudsley depressives. Br J Psychiatry 1988; 153:741–751Crossref, Medline, Google Scholar
88. Kiloh LG, Andrews M, Neilson M: The long-term outcome of depressive illness. Br J Psychiatry 1988; 153:752–757Crossref, Medline, Google Scholar
89. Andrews G, Neilson M, Hunt C, Stewart G, Kiloh LG: Diagnosis, personality and the long-term outcome of depression. Br J Psychiatry 1990; 157:13–18Crossref, Medline, Google Scholar
90. Vestergaard P, Aagaard J: Five-year mortality in lithium-treated manic-depressive patients. J Affect Disord 1991; 21:33–38Crossref, Medline, Google Scholar
91. Goldstein RB, Black DW, Nasrallah A, Winokur G: The prediction of suicide. Arch Gen Psychiatry 1991; 48:418–422Crossref, Medline, Google Scholar
92. Allgulander C, Allebeck P, Przybeck TR, Rice JP: Risk of suicide by psychiatric diagnosis in Stockholm County. Eur Arch Psychiatry Clin Neurosci 1992; 241:323–326Crossref, Medline, Google Scholar
93. Surtees PG, Barkley C: Future imperfect: the long-term outcome of depression. Br J Psychiatry 1994; 164:327–341Crossref, Medline, Google Scholar
94. Nilsson A: Mortality in recurrent mood disorders during periods on and off lithium: a complete population study in 362 patients. Pharmacopsychiatry 1995; 28:8–13Crossref, Medline, Google Scholar
95. Thies-Flechtner K, Mûller-Oerlinghausen B, Seibert W, Walther A, Greil A: Effect of prophylactic treatment on suicide risk in patients with major affective disorders. Pharmacopsychiatry 1996; 29:103–107Crossref, Medline, Google Scholar
96. Ringbäck-Weitoft G, Gullberg A, Rosen M: Avoidable mortality among psychiatric patients. Soc Psychiatry Psychiatr Epidemiol 1998; 33:430–437Crossref, Medline, Google Scholar
97. Pokorny AD: A follow-up study of 618 suicidal patients. Am J Psychiatry 1966; 122:1109–1116Google Scholar
98. Dahlgren KG: Attempted suicides—35 years afterward. Suicide Life Threat Behav 1977; 7:75–79Medline, Google Scholar
99. Fowler RC, Tsuang MT, Kronfol Z: Communication of suicidal intent and suicide in unipolar depression. J Affect Disord 1979; 1:219–225Crossref, Medline, Google Scholar
100. Beck AT, Steer RA, Kovas M, Garrison B: Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry 1985; 142:559–563Link, Google Scholar
101. Motto JA, Heilbron DC, Juster RP: Development of a clinical instrument to estimate suicide risk. Am J Psychiatry 1985; 142:680–686Link, Google Scholar
102. Beck AT, Steer RA: Clinical predictors of eventual suicide: a 5- to 10-year prospective study of suicide attempters. J Affect Disord 1989; 17:203–209Crossref, Medline, Google Scholar
103. Allgulander C, Fisher LD: Clinical predictors of completed suicide and repeated self-poisoning in 8,895 self-poisoning patients. Eur Arch Psychiatr Neurol Sci 1990; 239:270–276Crossref, Medline, Google Scholar
104. Nordstrom P, Asberg M, Aberg-Wistedt A, Nordin C: Attempted suicide predicts suicide risk in mood disorders. Acta Psychiatr Scand 1995; 92:345–350Crossref, Medline, Google Scholar
105. Mûtzell S: Survival after attempted suicide in Sweden: a follow-up after 20 years. Int J Adolescence and Youth 1997; 6:315–328Crossref, Google Scholar
106. Holley HL, Fick G, Love EJ: Suicide following an inpatient hospitalization for a suicide attempt: a Canadian follow-up study. Soc Psychiatry Psychiatr Epidemiol 1998; 33:543–551Crossref, Medline, Google Scholar
107. Sims A: Mortality in neurosis. Lancet 1973; 2:1072–1075Google Scholar
108. Nystrõm S: Factors related to 10-year prognosis. Acta Psychiatr Scand 1979; 60:225–238Crossref, Medline, Google Scholar
109. Martin RL, Cloninger RC, Guze SB, Clayton PL: Mortality in a follow-up of 500 psychiatric outpatients. Arch Gen Psychiatry 1985; 42:58–66Crossref, Medline, Google Scholar
110. Newman SC, Bland RC: Suicide risk varies by subtype of affective disorder. Acta Psychiatr Scand 1991; 83:420–426Crossref, Medline, Google Scholar
111. Tondo L, Baldessarini RJ, Hennen J, Floris G, Silvetti F, Tohen M: Lithium treatment and risk of suicidal behavior in bipolar disorder patients. J Clin Psychiatry 1998; 59:405–414Crossref, Medline, Google Scholar
112. Beck AT, Brown GK, Steer RA, Dahlsgaard KK, Grisham JR: Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide Life Threat Behav 1999; 29:1–9Medline, Google Scholar
113. Robins E, Murphy GE, Wilkinson RH, Glassner S, Kayes J: Some clinical considerations in the prevention of suicide based on a study of 134 successful suicides. Am J Public Health 1959; 49:888–898Crossref, Google Scholar
114. Geddes JR, Juszczak E: Period trends in rate of suicide in first 28 days after discharge from psychiatric hospital in Scotland, 1968–92. Br Med J 1995; 311:357–360Crossref, Medline, Google Scholar
115. Goldacre M, Seagroat V, Hawton K: Suicide after discharge from psychiatric inpatient care. Lancet 1993; 342:283–286Crossref, Medline, Google Scholar
116. Davies S, Naik PC, Lee AS: Lifetime risk of suicide in affective disorders (letter). Br J Psychiatry 1998; 173:185Crossref, Medline, Google Scholar
117. Amaddeo F, Bisoffi G, Bonizzato P, Micciolo R, Tansella M: Mortality among patients with psychiatric illness. Br J Psychiatry 1995; 166:783–788Crossref, Medline, Google Scholar
118. Simon GE, VonKorff M: Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol 1998; 147:155–160Crossref, Medline, Google Scholar
119. Sharma R, Markar HR: Mortality in affective disorder. J Affect Disord 1994; 31:91–96Crossref, Medline, Google Scholar
120. Black DW, Winokur G: Prospective studies of suicide and mortality in psychiatric patients. Ann NY Acad Sci 1986; 487:106–113Crossref, Medline, Google Scholar
121. James IP, Levin S: Suicide following discharge from psychiatric hospital. Arch Gen Psychiatry 1964; 10:43–46Crossref, Medline, Google Scholar
122. Allebeck P, Allgulander C: Psychiatric diagnoses as predictors of suicide: a comparison of diagnoses at conscription and in psychiatric care in a cohort of 50,465 young men. Br J Psychiatry 1990; 157:339–344Crossref, Medline, Google Scholar
123. VanGastel A, Schotte C, Maes M: The prediction of suicidal intent in depressed patients. Acta Psychiatr Scand 1997; 96:254–259Crossref, Medline, Google Scholar
124. Shneidman ES: Suicide as psychache. J Nerv Ment Dis 1993; 181:147–149Crossref, Google Scholar
125. Bronisch T: The relationship between suicidality and depression. Arch Suicide Res 1996; 2:235–254Crossref, Google Scholar
126. Keller F, Wolfersdorf M: Hopelessness and the tendency to commit suicide in the course of depressive disorders. Crisis 1993; 14:173–177Medline, Google Scholar
127. Goldney RD, Positano S, Spence ND, Rosenman SJ: Suicide in association with psychiatric hospitalization. Aust NZ J Psychiatry 1985; 19:177–183Crossref, Medline, Google Scholar



