Suicide Attempts Among Patients Starting Depression Treatment With Medications or Psychotherapy
Abstract
Objective: This study compared the time patterns of suicide attempts among outpatients starting depression treatment with medication or psychotherapy. Method: Outpatient claims from a prepaid health plan were used to identify new episodes of depression treatment beginning with an antidepressant prescription in primary care (N=70,368), an antidepressant prescription from a psychiatrist (N=7,297), or an initial psychotherapy visit (N=54,123). Outpatient and inpatient claims were used to identify suicide attempts or possible suicide attempts during the 90 days before and 180 days after the start of treatment. Results: Overall incidence of suicide attempt was highest among patients receiving antidepressant prescriptions from psychiatrists (1,124 per 100,000), lower among those starting psychotherapy (778 per 100,000), and lowest among those receiving antidepressant prescriptions in primary care (301 per 100,000). The pattern of attempts over time was the same in all three groups: highest in the month before starting treatment, next highest in the month after starting treatment, and declining thereafter. Results were unchanged after eliminating patients receiving overlapping treatment with medication and psychotherapy. Overall incidence of suicide attempt was higher in adolescents and young adults, but the time pattern was the same across all three treatments. Conclusions: The pattern of suicide attempts before and after starting antidepressant treatment is not specific to medication. Differences between treatments and changes over time probably reflect referral patterns and the expected improvement in suicidal ideation after the start of treatment.
In 2003, the U.K. Committee on Safety of Medicines raised concerns about newer antidepressant drugs precipitating suicidal ideation or suicide attempt, especially in adolescents (1) . After reviewing data from pediatric clinical trials, the U.S. Food and Drug Administration issued a “black box” warning recommending close monitoring for suicidal ideation after the start of antidepressants (2) .
These warnings prompted epidemiological studies examining suicide risk early in antidepressant treatment. Jick and colleagues (3) found that incidence of suicide attempt or suicide death was highest in the first few weeks after the start of antidepressants. This was interpreted by some as supporting traditional claims that medication transiently increases the risk of suicide attempt (4) . We subsequently reported that the incidence of suicide attempt was actually higher before the start of antidepressants (5) . This was interpreted by some as evidence for a protective effect, suggesting that antidepressants reduce the overall risk of suicide attempt (6) .
An alternative explanation is that these time trends simply reflect the expected improvement in depressive symptoms, including suicidal ideation, after the start of treatment. Patients often enter treatment at a time of crisis, characterized by high levels of suicidal ideation and other symptoms of depression. On average, suicidal ideation and other depressive symptoms decrease significantly after treatment begins, even when that treatment has no specific antidepressant effect. Here we compare time trends in suicide attempts among patients starting treatment with either antidepressant medications or psychotherapy in order to distinguish specific effects of either treatment from nonspecific effects.
Method
Depression treatment episodes and suicide attempts were identified with computerized claims records from Group Health Cooperative, a mixed-model prepaid health plan serving approximately 500,000 members in Washington state and northern Idaho. Group Health Cooperative enrollees are demographically similar to the area population and include members covered through capitation contracts with Medicare and Medicaid. Approximately 85% of new antidepressant prescriptions are written by primary care physicians. Individual psychotherapy is provided by both salaried group model providers (approximately 70%) and contracted network providers (approximately 30%).
Pharmacy and outpatient visit claims were used to identify all new episodes of antidepressant treatment for depression, defined as follows: filled prescription for any antidepressant drug between Jan. 1, 1996, and Dec. 1, 2005; no filled prescription for any antidepressant in the prior 180 days; at least one outpatient visit with a diagnosis of depressive disorder (ICD-9 codes 296.2, 296.3, 311, or 300.4) within 30 days of the initial prescription; age 7 or older at the time of the initial prescription; and continuously enrolled in Group Health Cooperative for 180 days before the initial prescription. Treatment episodes were further classified by the specialty of the prescribing physician (psychiatry versus primary care and other general medical providers).
Computerized outpatient claims data were used to identify all new episodes of psychotherapy for depression, defined as follows: outpatient visit to a specialty mental health provider for individual psychotherapy (CPT codes 90801 to 90844) with a diagnosis of depressive disorder (ICD-9 codes 296.2, 296.3, 311, or 300.4) between Jan. 1, 1996, and Dec. 31, 2005; no individual psychotherapy visit in the prior 180 days; age 7 or older at the initial psychotherapy visit, and continuously enrolled in Group Health Cooperative for 180 days before the initial psychotherapy visit.
Computerized inpatient and outpatient claims data were used to identify all hospitalizations or emergency room encounters with diagnoses of definite suicide attempt (ICD codes E950 through E958) or possible suicide attempt (ICD codes E980 through E987) in the 90 days before or 180 days after the initial antidepressant prescription or psychotherapy visit.
In order to validate diagnoses of suicide attempt from claims data, G.E.S. reviewed a sample of 30 medical records (outpatient notes, emergency room notes, and inpatient discharge summaries) from the possible suicide attempt group (codes E980 through E987) and 30 from the definite suicide attempt group (codes E950 through E958). In the possible suicide attempt group, chart notes clearly documented intentional injury in 24 (80%) and clearly documented suicidal intent in 21 (70%). In the definite suicide attempt group, chart notes clearly documented intentional injury in 30 (100%) and suicidal intent in 30 (100%).
Within each treatment group (medication from primary care physician, medication from psychiatrist, psychotherapy), the relative odds of suicide attempt over time were examined in repeated-measures logistic regression models (one observation per person per month). A set of three indicator variables compared the relative odds of suicide attempt in the month after the beginning of treatment to those in three other periods: <1 month before the start of treatment, the month before the start of treatment, and >1 month after the start of treatment. These comparisons are reported as odds ratios with 95% confidence intervals.
Results
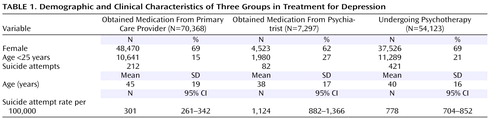
The criteria described above identified a total of 131,788 treatment episodes among 109,256 individuals. Approximately 55% of the treatment episodes began with an antidepressant prescription in primary care, approximately 40% with a psychotherapy visit, and approximately 5% with an antidepressant prescription from a psychiatrist. Table 1 compares the characteristics of the three treatment groups. The patients receiving antidepressant prescriptions from psychiatrists were younger and more often male. In the total group, there were 715 suicide attempts (including 618 coded as definite suicide attempts and 97 as possible suicide attempts) in the period beginning 90 days before treatment was started and ending 180 days after treatment was started. As shown in Table 1 , the overall incidence of suicide attempt during this period was highest among patients receiving antidepressant treatment from a psychiatrist, slightly lower among patients starting psychotherapy, and much lower among patients starting antidepressant treatment in primary care.
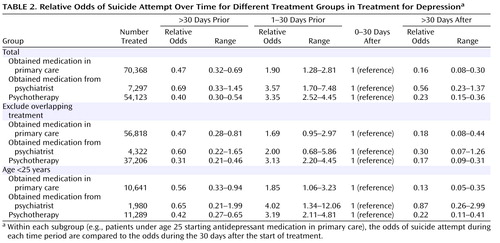
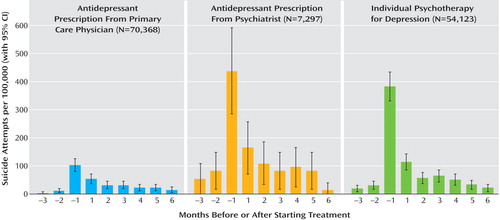
Figure 1 displays the prevalence of suicide attempts by month in the three treatment groups. Although the overall incidence varied across the three groups, the time pattern was identical. Incidence was highest in the month before the start of treatment, was next highest in the month after the start of treatment, and declined steadily thereafter. The top portion of Table 2 shows the results of logistic regression models comparing different time periods in each of the three groups. In all three groups, the odds of suicide attempt during the month before the start of treatment were significantly higher than in the month after. This effect was smaller in patients starting antidepressants in primary care than in those treated by specialists. In all three groups, the odds of suicide attempt were lower in the period more than 1 month before the start of treatment and the period more than 1 month after the start of treatment. These latter differences were not statistically significant in the group receiving medication from a psychiatrist, with wider confidence limits in that group reflecting the much smaller group size.
Secondary analyses excluded the subgroup of patients with any overlapping treatment. For the two medication groups, these analyses excluded those making any psychotherapy visit in the 3 months before or 6 months after starting medication. For the psychotherapy group, these analyses excluded those filling any antidepressant prescription in the 3 months before or 6 months after the first psychotherapy visit. The results of logistic regression models for this subgroup are shown in the middle portion of Table 2 . Changes in the odds of suicide attempt over time do not differ from those in the full group, but confidence limits are wider, reflecting the smaller group size.
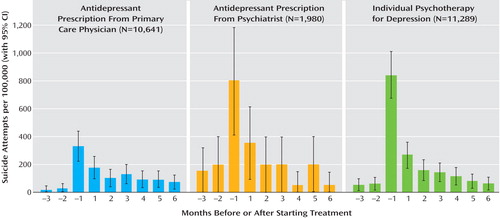
Figure 2 displays parallel analysis restricted to patients ages less than 25. Across all three groups, the overall incidence of suicide attempt was approximately twice as high in this subgroup as in the full group. Nevertheless, adolescents and younger adults showed the same time pattern seen in the full group: the highest incidence in the month before the start of treatment, next highest in the month after the start of treatment, and declining steadily thereafter. The bottom portion of Table 2 displays the results of logistic regression models in the adolescent and young adult subgroup. The pattern of results (both between treatment groups and between time periods) did not differ meaningfully from that in the full group. Confidence limits for odds ratios were wider, reflecting the smaller group size.
Discussion
We found the same pattern in the timing of suicide attempts among patients starting depression treatment with psychotherapy as among those starting antidepressant medication, either from a primary care physician or a psychiatrist. In all three groups, the incidence of suicide attempt was highest in the month before the start of treatment and declined steadily over the next 6 months. The striking similarity across the three groups suggests that this time pattern reflects the expected improvement in depression and suicidal ideation when starting treatment rather than any specific effect of either medication or psychotherapy. Although the incidence was higher in the first month of treatment than in subsequent months, this should not be attributed to a specific adverse effect of medication. And while the incidence appeared to decline immediately after the start of treatment, this should not be attributed to a specific protective effect.
Any observational study comparing suicide attempts among patients receiving different treatments (or comparing treated and untreated patients) will be subject to confounding by indication. That is, patients receive different depression treatments because of differences in the severity of depression and/or differences in the perceived risk of suicide attempt. Consequently, any observed differences in suicide attempts after treatment may reflect preexisting differences in risk rather than any specific effect of treatment. Researchers can attempt to reduce this bias by studying more homogeneous patient groups or by using clinical data to adjust for preexisting differences in depression severity. But residual confounding or bias is likely to persist. Our findings regarding differences between patients receiving antidepressant prescriptions from psychiatrists and primary care physicians illustrate this problem of residual confounding. In previous research conducted in this same health care system (7) , we demonstrated that patients starting antidepressant treatment in psychiatric clinics and primary care clinics differ only slightly in the severity of depression as measured by conventional diagnostic interviews or symptom scales. Nevertheless, this and earlier studies (8) found that rates of suicide attempt or suicide death are at least three times as high among patients treated by psychiatrists. We do not interpret this difference as evidence that psychiatric care increases the risk of suicide. Instead, we would conclude that referrals to specialty care are appropriately informed by assessment of the risk. Patients at higher risk for suicide attempts are more often referred for psychiatric care. Similarly, we take care not to draw any conclusions from the comparison of overall suicide attempt rates in patients starting psychotherapy to rates in either of the pharmacotherapy groups. Overall incidence was higher in the psychotherapy group than in the primary care pharmacotherapy group, but this almost certainly reflects referral patterns rather than some harmful or negative effect of psychotherapy. Overall incidence was similar in the psychotherapy and the pharmacotherapy-from-psychiatrists group, reflecting the fact that high-risk patients are more often referred to specialty care.
These data offer some reassurance that overall risk of suicide attempt declines after depression treatment is started, with either medication or psychotherapy. They also suggest that patterns of suicide risk early in depression treatment are more influenced by referral patterns and the expected improvement in depression after treatment is started than by specific effects of any particular treatment. If either antidepressant medication or psychotherapy has a specific effect on the risk of suicide attempt, those specific effects were not apparent in this group of patients treated in community practice. Our findings suggest that any specific effects are not large enough to emerge from the nonspecific pattern common to all treatments. These data do not, however, exclude the possibility that depression treatment may precipitate suicidal ideation or suicide attempt in vulnerable individuals (9) .
We rely on administrative data to identify suicide attempts diagnosed during outpatient encounters or hospitalizations. Our chart reviews suggest that this method has good specificity (i.e., events identified are almost certainly true suicide attempts). But this method would overlook any attempts that either do not come to the attention of health care providers or are not formally diagnosed. We would not expect this to bias comparisons across treatments because diagnoses were made almost exclusively by emergency room and inpatient providers (rather than by treating psychiatrists, psychotherapists, or primary care physicians). We might expect, however, that self-injury might be more often classified as suicide attempt after depression treatment was started than before. Consequently, the decline in risk of suicide attempt after the start of treatment may be larger than our findings indicate.
Interpretation of these findings should consider some other important limitations. First, we cannot directly assess the severity of depression either before or after starting treatment. Although we assume that overall differences in risk among the three treatment groups reflect preexisting differences in severity, we cannot test that assumption using these data. Second, one-third or more of patients starting depression treatment (with either medication or psychotherapy) drop out within a few weeks (10 , 11) . These high rates of nonadherence would make it more difficult to distinguish any specific treatment effects from nonspecific effects of help-seeking and spontaneous improvement.
For the time being, physicians and other health care providers are faced with an apparent conflict between findings of placebo-controlled trials and findings of epidemiological or observational studies. Data from placebo-controlled trials clearly indicate that newer antidepressants can increase suicidal thoughts and suicidal behavior in adolescents and young adults during the first several weeks of treatment (12 , 13) . The number of actual suicide attempts in those studies, however, was too small to compare rates in the antidepressant and placebo groups. Consequently, we cannot determine whether the effect of antidepressants on suicidal ideation or behavior translates to an increased risk of actual suicide attempt or suicide death. In contrast, placebo-controlled trials in older adults found a possible reduction in risk of suicidal ideation (13) and no significant effect on the risk of actual suicide attempt (14) or suicide death (15) . Observational studies in adults and adolescents found that the risk of suicide attempt actually declines after treatment is started (5) and that areas with higher rates of antidepressant use tend to have lower rates of suicide death (16 , 17) . Autopsy studies found low rates of antidepressant exposure among adolescents dying by suicide (18 , 19) . We should emphasize that any of these methods (randomized trials or large observational studies) can only examine average effects. Even a finding that antidepressants reduce suicidal ideation or behavior in older adults would not exclude the possibility that medication may increase the risk in a vulnerable subgroup of patients (9) . Given this uncertainty, prescribers should certainly heed recommendations by the U.S. Food and Drug Administration to advise patients about this risk and to maintain close contact after patients start medication (2) .
1. UK Committee on Safety of Medicines: Seroxat Must Not Be Used for Treatment of Children, June 10, 2003. http://www.mhra.gov.uk/home/idcplg?IdcService=SS_GET_PAGE&us eSecondary=true&ssDocName=CON2015704&ssTargetNo deId=221Google Scholar
2. Center for Drug Evaluation and Research, US Food and Drug Administration: FDA Public Health Advisory: Worsening Depression and Suicidality in Patients Being Treated With Antidepressant Medications, March 22, 2004. http://www.fda.gov/cder/drug/antidepressants/AntidepressanstPHA.htmGoogle Scholar
3. Jick H, Kaye J, Jick S: Antidepressants and the risk of suicidal behaviors. JAMA 2004; 292:338–343Google Scholar
4. Mayer-Gross W, Slater E, Roth M: Clinical Psychiatry. London, Cassell, 1960Google Scholar
5. Simon GE, Savarino J, Operskalski B, Wang PS: Suicide risk during antidepressant treatment. Am J Psychiatry 2006; 163:41–47Google Scholar
6. Berenson A: Antidepressants seem to cut suicide risk in teenagers and adults, study says. New York Times, Jan 1, 2006, p 1Google Scholar
7. Simon G, Von Korff M, Rutter C, Peterson D: Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry 2001; 58:395–401Google Scholar
8. Simon G, Von Korff M: Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol 1998; 147:155–160Google Scholar
9. Teicher M, Glod CA, Cole JO: Antidepressant drugs and the emergence of suicidal tendencies. Drug Saf 1993; 8:186–212Google Scholar
10. Simon G, Von Korff M, Wagner EH, Barlow W: Patterns of antidepressant use in community practice. Gen Hosp Psychiatry 1993; 15:399–408Google Scholar
11. Horvitz-Lennon M, Normand SL, Frank RG, Goldman HH: “Usual care” for major depression in the 1990s: characteristics and expert-estimated outcomes. Am J Psychiatry 2003; 160:720–726Google Scholar
12. Hammad T, Laughren T, Racoosin J: Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry 2006; 63:332–339Google Scholar
13. Stone M, Jones M: Clinical Review: Relationship Between Antidepressant Drugs and Suicidality in Adults, Nov 16, 2006. http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdfGoogle Scholar
14. Hammad T, Laughren T, Racoosin J: Suicide rates in short-term randomized controlled trials of newer antidepressants. J Clin Psychopharmacol 2006; 26:203–207Google Scholar
15. Khan A, Khan S, Kolts R, Brown WA: Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003; 160:790–792Google Scholar
16. Gibbons R, Hur K, Bhaumik D, Mann J: The relationship between antidepressant medication use and rate of suicide. Arch Gen Psychiatry 2005; 62:165–172Google Scholar
17. Gibbons RD, Hur K, Bhaumik DK, Mann JJ: The relationship between antidepressant prescription rates and rate of early adolescent suicide. Am J Psychiatry 2006; 163:1898–1904Google Scholar
18. Leon A, Marzuk P, Tardiff K, Bucciarelli A, Markham Piper T, Galea S: Antidepressants and youth suicide in New York City, 1999–2002. J Am Acad Child Adolesc Psychiatry 2006; 45:1054–1058Google Scholar
19. Leon A, Marzuk P, Tardiff K, Teres J: Paroxetine, other antidepressants, and youth suicide in New York City: 1993 through 1998. J Clin Psychiatry 2004; 65:915–918Google Scholar