Substance Abuse in First-Episode Bipolar I Disorder: Indications for Early Intervention
Abstract
OBJECTIVE: This study clarified the early characteristics of substance use disorders in patients with first-episode bipolar I disorder. METHOD: The authors evaluated substance use disorders, associated factors, and clinical course, prospectively, in the first 2 years of DSM-IV bipolar I disorder with standardized methods. RESULTS: Baseline substance use disorder was found in 33% (37 of 112) of the patients at baseline and in 39% at 24 months. Anxiety disorders were more frequent in the patients with than without substance use disorder (30% and 13%, respectively). Associations of alcohol dependence with depressive symptoms and cannabis dependence with manic symptoms were suggested. Patients using two or more substances had worse outcomes. CONCLUSIONS: Since substance use disorders were frequent from the beginning of bipolar I disorder and were associated with anxiety disorders and poor outcome, early interventions for substance use disorder and anxiety might improve later outcome.
Patients with bipolar I disorder have high risks of comorbid substance use disorders, with lifetime prevalence as high as 50%–60% (1). Substance use disorder comorbidity is eventually associated with worse bipolar I disorder outcome and higher suicidal risk, but very little is known about substance use disorder in early bipolar I disorder (2–5). Therefore, we analyzed data from the McLean-Harvard First Episode Mania Study to evaluate the timing of specific substance use disorders, associated risk factors, and relationships to clinical outcomes in the first 24 months of follow-up.
Method
Case finding, diagnostic, and assessment methods were detailed previously (6). The subjects were consecutive patients (ages 18–75) who were admitted to McLean Hospital (1989–1996) for a first lifetime manic/mixed bipolar I episode (updated to DSM-IV criteria) after providing written informed consent with institutional review board approval (6). Raters with ≥5 years of clinical research experience carried out interviews with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID), Patient Edition, and maintained high interrater reliability (intraclass correlation coefficient [ICC]=0.92 for primary, 0.90 for secondary diagnoses) (6). Demographic and clinical data were collected from patients and families by trained research assistants to supplement semistructured interviews with relatives and treating clinicians, and data were extracted from clinical records. Substance use disorder diagnoses (alcohol, cannabis, cocaine, hallucinogens, opiates, sedatives, and stimulants) were ascertained by the SCID. Diagnoses of anxiety disorders and other secondary conditions were based on best-estimate methods using the baseline SCID and follow-up data (6).
Inpatients were assessed weekly until discharge; all 112 subjects were then followed up at 6, 12, and 24 months postdischarge to document current and intervening clinical status, substance use patterns, occupational and residential functional status, and clinically determined treatment according to community standards; 80 also underwent a second SCID assessment at 24 months. Trained follow-up interviewers who were blind to baseline information used semistructured telephone interviews of demonstrated reliability and comparability to in-person assessments (mean ICC=0.90) (6). Syndromal recovery from mania was the primary clinical outcome measure (definition: Clinical Global Impression improvement rating ≤2 and severity rating ≤3 for DSM-IV criterion A for mania, with no B criterion rated >3 and not more than one B criterion rated 3, all sustained for ≥8 weeks). Patients with mixed episodes fulfilled these criteria and comparable criteria for major depressive episodes (6). Number of weeks to recovery was timed from hospital entry.
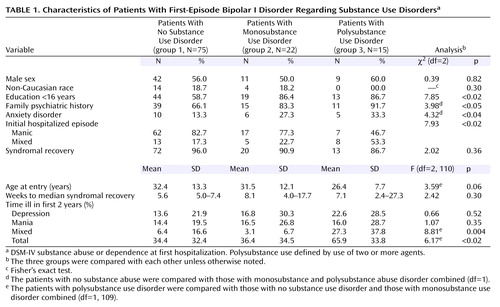
The subjects were divided into three groups: group 1, no substance use disorder diagnosis; group 2, abuse of a single agent; and group 3, abuse of two or more substances. The distributions of selected factors among these subgroups were tested with contingency tables (chi-square or Fisher’s exact p if cell size <10) for categorical measures or linear regression modeling methods (F) for continuous measures (all at dfs stated in Table 1). Median times to recovery and their 95% confidence intervals were estimated with survival analysis based on Cox proportional hazards modeling (chi-square analysis [df=1]). For regression modeling, age at entry and percentages of time ill were transformed logarithmically to afford near-Gaussian data distributions. Data are reported as means or computed values with 95% confidence intervals. Statistical significance required two-tailed p<0.05. We used STATA statistical software (Stata Corp., College Station, Tex.).
Results
Of 112 patients with DSM-IV bipolar I disorder, 75 (67.0%) had no substance use disorder at study entry (group 1), whereas 37 (33.0%) did (groups 2 and 3); 29 were dependent on a substance (78.4% of substance use disorder cases and 25.9% of all patients), and eight met criteria for abuse. Of 22 subjects using one substance only (group 2), 17 used alcohol, four cannabis, and one heroin; the 15 in group 3 abused two or more substances (Table 1). Dependence was ranked as follows: 23 with alcohol, 11 cannabis, five cocaine, and one hallucinogens; abuse was ranked as follows: seven with alcohol, four cannabis, one cocaine, and two hallucinogens. For both dependence and abuse, there was considerable overlap in use of different drugs (average=1.8 per substance use disorder case). The prevalence of substance use disorder rose to 38.8% at 24 months (31 of 80 with a second SCID assessment).
Polydrug use subjects (group 3) versus nonabusers (group 1) were younger, less well educated, more likely to have a family history of psychiatric illness, and to be seen initially in mixed states. Subgroups with no abuse and monodrug use were similar in all of these baseline measures, and the subgroups did not differ by sex or race. Comorbidity with any anxiety disorder was more common with substance use disorders. Patients with polydrug use spent more time ill during follow-up (especially in mixed episodes). Syndromal recovery was similar across subgroups. Other morbidity at 2 years (including initial depression severity and time spent in major depression/dysthymia or mania) did not differ significantly among subgroups (Table 1).
We also compared 2-year outcomes of patients with no substance use disorder versus alcohol-dependent (N=23) versus cannabis-dependent patients (N=11). Patients with no substance use disorder spent similar proportions of time in manic and depressive illness (mean=14.4%, SD=19.5%, versus mean=13.5%, SD=21.9%; ratio=1.1:1). Cannabis-dependent subjects spent more time in mania (mean=26.8%, SD=34.0%, versus mean=11.5%, SD=19.1%; ratio=2.3:1), whereas alcohol-dependent patients spent much more time depressed (mean=11.9%, SD=22.9%, in mania versus mean=21.9%, SD=29.5%, in depression; ratio=1:1.8). However, these findings did not reach statistical significance, and there was a considerable overlap in the use of both drugs.
Discussion
This preliminary assessment indicated that the prevalence of substance use disorder was already substantial among first-episode, DSM-IV bipolar I subjects (33%), reaching 39% by 24 months. Syndromal recovery from index mania occurred at similar rates across substance use disorder subgroups. However, overall morbidity during follow-up was particularly severe among patients with polysubstance use disorder, whereas patients with monosubstance use disorder had surprisingly good early outcomes. A previously suggested (3) association of alcohol with depression and cannabis with mania was found and warrants further study.
Of note, patients with comorbid substance use disorder were more likely than nonusers to be diagnosed with a DSM-IV anxiety disorder. A link between anxiety and substance use disorders in major affective disorders has been proposed (4), but the cause-effect relationships remain unclear. Substance use might sometimes ameliorate anxiety symptoms or anxiety worsened by substance use disorder. The evident association suggests the testable hypothesis that very early clinical interventions in new bipolar I disorder aimed at limiting both anxiety symptoms and substance use disorder might contribute to improved outcomes.
 |
Presented in part at the 157th annual meeting of the American Psychiatric Association, New York, May 1–6, 2004. Received Jan. 27, 2004; revisions received April 30 and May 28, 2004; accepted June 14, 2004. From the Department of Psychiatry and the Neuroscience Program, Harvard Medical School, Boston; the Bipolar & Psychotic Disorders Program and International Consortium for Bipolar Disorder Research, Mailman Research Center, McLean Hospital; the Department of Clinical Neuroscience, University of Parma, Italy; and Lilly Research Laboratories, Indianapolis. Address correspondence and reprint requests to Dr. Baethge, Department of Psychiatry, Harvard Medical School, McLean Hospital, 115 Mill St., Belmont, MA 02478-9106; [email protected] (e-mail). Supported by the Max Kade Foundation, a National Alliance for Research on Schizophrenia and Depression Young Investigator Award (to Dr. Baethge), the Bruce J. Anderson Foundation, and the McLean Private Donors Research Fund (to Dr. Baldessarini).
1. Cassidy F, Ahearn EP, Carroll BJ: Substance abuse in bipolar disorder. Bipolar Disord 2001; 3:181–188Crossref, Medline, Google Scholar
2. Tohen M, Greenfield SF, Weiss RD, Zarate CA Jr, Vagge LM: The effect of comorbid substance use disorders on the course of bipolar disorder: a review. Harv Rev Psychiatry 1998; 6:133–141Crossref, Medline, Google Scholar
3. Strakowski SM, DelBello MP, Fleck DE, Arndt S: The impact of substance abuse on the course of bipolar disorder. Biol Psychiatry 2000; 48:477–485Crossref, Medline, Google Scholar
4. Goodwin RD, Stayner DA, Chinman MJ, Wu P, Tebes JK, Davidson L: The relationship between anxiety and substance use disorders among individuals with severe affective disorders. Compr Psychiatry 2002; 43:245–252Crossref, Medline, Google Scholar
5. Dalton EJ, Cate-Carter TD, Mundo E, Parikh SV, Kennedy JL: Suicide risk in bipolar patients: the role of comorbid substance use disorders. Bipolar Disord 2003; 5:58–61Crossref, Medline, Google Scholar
6. Tohen M, Zarate CA Jr, Hennen J, Khalsa H-MK, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ: The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry 2003; 160:2099–2107Link, Google Scholar



