Axis I Comorbidity of Borderline Personality Disorder
Abstract
Objective:The purpose of this study was to assess the lifetime rates of occurrence of a full range of DSM-III-R axis I disorders in a group of patients with criteria-defined borderline personality disorder and comparison subjects with other personality disorders. Method:The axis I comorbidity of 504 inpatients with personality disorders was assessed by interviewers who were blind to clinical diagnosis and who used a semistructured research interview of demonstrated reliability.Results:Four new findings emerged from this study. First, anxiety disorders were found to be almost as common among borderline patients (N=379) as mood disorders but far more discriminating from axis II comparison subjects (N=125). Second, posttraumatic stress disorder (PTSD) was found to be a common but not universal comorbid disorder among borderline patients, a finding inconsistent with the view that borderline personality disorder is actually a form of chronic PTSD. Third, male and female borderline patients were found to differ in the type of disorder of impulse in which they “specialized.” More specifically, substance use disorders were significantly more common among male borderline patients, while eating disorders were significantly more common among female borderline patients. Fourth, a lifetime pattern of complex comorbidity (i.e., met DSM-III-R criteria for both a disorder of affect and a disorder of impulse at some point before the patients’ index admission) was found to have strong positive predictive power for the borderline diagnosis as well as a high degree of sensitivity and specificity. Conclusions:These results suggest that the lifetime pattern of axis I comorbidity characteristic of borderline patients and distinguishing for the disorder is a particularly good marker for borderline personality disorder. Am J Psychiatry 1998; 155: 1733-1739
Borderline patients often present for evaluation or treatment with one or more comorbid axis I disorders. Initially, these symptom disorders may mask the underlying borderline psychopathology, impeding accurate diagnosis and making treatment planning difficult. Over time, these disorders often prove to be treatment resistant; additional axis I disorders may also develop. Because of the frequency with which these clinically difficult situations occur, a substantial amount of research concerning the axis I comorbidity of borderline personality disorder has been conducted.
Fifteen studies that have assessed the rate of more than one or two axis I disorders in patients with criteria-defined borderline personality disorder have been published (1–15). In general, these studies have found that borderline patients often meet DSM criteria for a number of common axis I disorders, particularly major depression (3, 4,8, 10, 11, 13–15) and substance abuse(1, 3–5, 7, 8, 10, 13–15). These studies have also found that a substantially higher percentage of borderline patients than comparison subjects have met DSM criteria for a chronic affective disorder (1, 2, 15) or a substance use disorder(2, 3, 7, 12, 15). In addition, two studies have found that borderline patients are at heightened risk for developing an anxiety disorder (2,12).
Despite the consistency of these findings, the generalizability of the results of these studies has been limited by five main methodological problems. First, only slightly more than half of these studies used a semistructured research interview to assess the presence or absence of borderline personality disorder(2, 4, 5, 8, 10, 12, 13, 15). Second, only one study assessed the axis I comorbidity of borderline patients and comparison subjects by interviewers who were blind to clinically obtained information, including axis I and II diagnoses given before entry into the study (15). Third, only seven of the studies assessed the lifetime rate of axis I disorders by using semistructured interviews of demonstrated reliability(2, 4, 5, 10, 12, 13, 15). Fourth, only six of these studies reported on a full range of axis I disorders (24, 8, 9, 14, 15). Fifth, only five of these studies used a comparison group that consisted exclusively of subjects with axis II disorders (1, 6, 10, 13, 15).
The present study builds upon the design of these earlier studies by incorporating all five of the following features. First, borderline status was assessed according to well-defined research criteria with semistructured interviews of proven reliability and validity. Second, axis I comorbidity was assessed by interviewers who were blind to clinical diagnoses. Third, these assessments were made by using a semistructured interview with demonstrated reliability. Fourth, the rates of occurrence of a full range of axis I disorders were not only assessed but reported. Fifth, a rigorously diagnosed group of patients with personality disorders was used as comparison subjects.
The present study is also, to the best of our knowledge, the first large-scale controlled study to assess the axis I comorbidity of borderline personality disorder according to DSM-III-R criteria. In addition, it is the first study to assess the effect of gender on the axis I comorbidity exhibited by borderline patients.
METHOD
All subjects were inpatients at McLean Hospital in Belmont, Mass., who were admitted between March 1991 and December 1995. Each patient was initially screened to determine that he or she 1) was between the ages of 18 and 50; 2) had normal or better intelligence; 3) had no history or current symptoms of a serious organic condition that might be associated with the development of psychiatric symptoms (e.g., multiple sclerosis, lupus erythematosus), schizophrenia, or bipolar I disorder; and 4) had been given a definite or probable axis II diagnosis by the admitting physician (who also rated each patient’s level of impairment with the Global Assessment of Functioning Scale [GAF] contained in DSM-III-R).
Written informed consent was obtained from each patient. Three semistructured diagnostic interviews were then administered to each patient by one of five interviewers (E.D.D., A.E.S., A.T., A.L., V.R.) who were blind to the patient’s clinical diagnoses. These instruments were 1) the Structured Clinical Interview for DSM-III-R (16) (which included a posttraumatic stress disorder [PTSD] module that was devised at McLean Hospital and used subthreshold criteria for mania to determine the presence of hypomanic episodes and bipolar II disorder)—a semistructured interview designed to assess the lifetime frequency of many of the most common axis I disorders described in DSM-III-R, 2) the Revised Diagnostic Interview for Borderlines (DIB-R)—a semistructured interview that can reliably distinguish clinically diagnosed borderline patients from those with other axis II disorders (17), and 3) the Diagnostic Interview for DSM-III-R Personality Disorders (18)—a semistructured interview that reliably assesses the presence of the 13 axis II disorders described in DSM-III-R. All five interviewers had been trained in the administration and scoring of these instruments by the first author (M.C.Z.), who is one of the developers of both the DIB-R and Diagnostic Interview for DSM-III-R Personality Disorders. Adequate levels of interrater reliability had been obtained during this training period, which consisted of 15 conjoint interviews (e.g., pairwise kappa of 0.85 or higher on the DIB-R and DSM-III-R diagnoses of borderline personality disorder).
Because there is a certain degree of overlap between a few of the DIB-R criteria for borderline personality disorder and certain of the axis I disorders being studied (major depression/dysthymia, generalized anxiety disorder/simple phobia/panic disorder, alcohol/drug abuse/dependence, and the binge eating aspect of bulimia and/or eating disorder not otherwise specified), we removed these items from the DIB-R and found that all patients who had initially met DIB-R criteria for borderline personality disorder continued to do so. This is probably because of the severity of the borderline psychopathology of the inpatients in the study (i.e., they scored 9 or 10 on the DIB-R, which has a maximum score of 10), as well as the weighted scoring system of the DIB-R, which has over 100 questions that are used to rate 22 summary statements—only four of which were affected in any way by removing these more specific items. We performed a parallel procedure for the DSM-III-R criteria for borderline personality disorder (i.e., removed the affective instability criterion, since it reflects one element of bipolar II disorder and removed the criterion pertaining to two patterns of impulsive behavior [if the patient both abused a substance and engaged in eating binges]). Again, no patient’s borderline status changed, probably because most borderline patients in the study met seven or eight of the DSM-III-R criteria for borderline personality disorder.
Between-group comparisons involving categorical data were computed by using the chi-square statistic corrected for continuity; between-group comparisons involving continuous data (age and socioeconomic status) were computed by using Student’s t test. The Bonferroni correction for multiple comparisons was applied where appropriate. Multivariate analyses were also conducted by using logistic regression methods with presence/absence of borderline personality disorder as the dependent variable and axis I disorders that were found to be significant in univariate analyses (p<0.05) as the independent variables.
RESULTS
All told, 520 patients were interviewed. Three hundred seventy-nine patients met both DIB-R and DSM-III-R criteria for borderline personality disorder, and 125 met DSM-III-R criteria for at least one nonborderline axis II disorder. Thirteen of the comparison subjects (10%) met DSM-III-R criteria for an odd cluster disorder, 59 (47%) met DSM-III-R criteria for an anxious cluster disorder, and 38 (30%) met DSM-III-R criteria for a dramatic cluster disorder. Another 45 (36%) met DSM-III-R criteria for personality disorder not otherwise specified (which was operationally defined in the Diagnostic Interview for DSM-III-R Personality Disorders as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R). Sixteen others were excluded from further analyses because they either met criteria for schizophrenia (N=2) or bipolar I disorder (N=2) or failed to met DSM-III-R criteria for any axis II disorder, including personality disorder not otherwise specified (N=12).
Demographically, borderline patients were found to be very similar to comparison subjects in terms of their marital status, race, and socioeconomic background. More specifically, about two- thirds of each group had never been married (70% versus 64%), 11% of each group was nonwhite, and each group had a mean socioeconomic status, as measured by the five-point Hollingshead-Redlich scale (19) (1=highest, 5=lowest), of 2.6 (SD=1.3). However, borderline patients were found to be slightly, but significantly, younger than axis II comparison subjects (mean=27.6 years, SD=6.9, versus mean=29.2, SD=8.9) (t=2.10, df=502, p=0.04). In addition, a significantly higher percentage of borderline patients (78%) than comparison subjects (56%) were women (χ2=21.99, df=1, p=0.00001). The admitting physician’s GAF rating of impairment was about the same for both groups (mean=28.7, SD=7.1, versus mean=29.5, SD=8.4).
We initially compared the lifetime axis I comorbidity of borderline patients and axis II comparison subjects. Because a significantly higher percentage of borderline patients than comparison subjects were women, two subanalyses to examine the role of gender were also conducted. Because the results of these analyses were somewhat different for male and female borderline patients and comparison subjects, we decided to present our results for men and women separately, as well as our overall results comparing the mixed-gender group of borderline patients and comparison subjects.
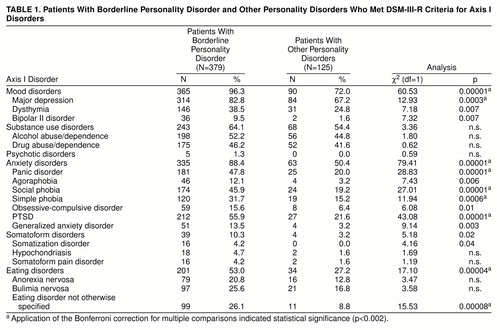
Table 1 compares borderline patients and axis II comparison subjects on lifetime rates of axis I disorders. At the Bonferroni-corrected alpha level of p<0.002, a significantly higher percentage of borderline patients than comparison subjects met DSM-III-R criteria for six specific disorders (major depression, panic disorder, social phobia, simple phobia, PTSD, and eating disorder not otherwise specified) and three types of disorder (mood, anxiety, and eating disorders).
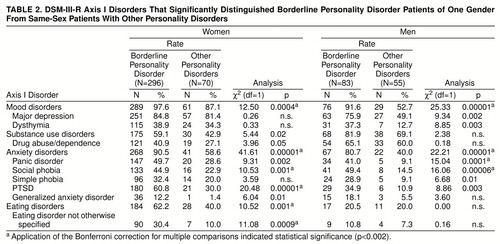
Table 2 presents the rates of axis I disorders that significantly distinguished borderline patients of one gender from same-sex comparison subjects. At the Bonferroni-corrected alpha level of p<0.002, a significantly higher percentage of female borderline patients than female comparison subjects met DSM-III-R criteria for three specific disorders (social phobia, PTSD, and eating disorder not otherwise specified) and three types of disorder (mood, anxiety, and eating disorders). At this stringent alpha level, a significantly higher percentage of male borderline patients than male comparison subjects met DSM-III-R criteria for two specific disorders (panic disorder and social phobia) and two types of disorder (mood and anxiety disorders).
While male and female borderline patients had similar rates of comorbidity in the areas of psychotic disorders (about 1%), somatoform disorders (about 10%), anxiety disorders (over 80%), and mood disorders (over 90%), they were also found to be significantly different from one another in the areas of substance use disorders and eating disorders. At the Bonferroni-corrected alpha level of p<0.002, a significantly higher percentage of male than female borderline patients met DSM-III-R criteria for alcohol abuse/dependence (74% versus 46%) (χ2=18.16, df=1, p=0.00002), drug abuse/dependence (65% versus 41%) (χ2=14.29, df=1, p=0.0002), and overall substance abuse/dependence (82% versus 59%) (χ2=13.68, df=1, p=0.0002). In contrast, a significantly higher percentage of female than male borderline patients met DSM-III-R criteria for anorexia nervosa (25% versus 7%) (χ2=10.91, df=1, p=0.001), bulimia nervosa (30% versus 10%) (χ2=13.15, df=1, p=0.0003), eating disorder not otherwise specified (almost all cases were of binge eating disorder or purging disorder) (30% versus 11%) (χ2=11.86, df=1, p=0.0006), and the overall eating disorder category (62% versus 21%) (χ2=43.55, df=1, p=0.00001). In addition, female borderline patients were significantly more likely than male borderline patients to have met DSM-III-R criteria for PTSD (61% versus 35%) (χ2=16.51, df=1, p=0.00005).
We next conducted multivariate analyses that mirrored the three sets of univariate analyses described earlier in this article. We found that the same disorders were highly significant in discriminating a mixed-gender group of borderline patients from a mixed-gender group of comparison subjects (χ2=90.57, df=1, p<0.00001), same-sex borderline patients from same-sex comparison subjects (women: χ2=41.40, df=1, p<0.00001; men: χ2=35.35, df=1, p<0.00001), and male from female borderline patients (χ2=65.70, df=1, p<0.00001).
Suspecting that the overall pattern of comorbidity displayed by borderline patients was more discriminating than the rates of separate types of disorders, we ran a series of logistic regressions and found that a summary measure representing what we have termed complex comorbidity better discriminated borderline patients from comparison subjects than each of the six types of axis I disorders studied (data not shown). The operational definition of complex comorbidity is that a patient has met the DSM-III-R criteria for a broadly defined disorder of affect (a mood disorder and an anxiety disorder) and meets DSM-III-R criteria for a disorder of impulsivity (a substance use disorder or an eating disorder or both). Overall, a significantly higher percentage of borderline patients than comparison subjects met DSM-III-R criteria for a combination of disorders of affect and impulsivity (73% versus 27%) (χ2=82.95, df=1, p<0.00001). The same pattern of comorbidity was found to be discriminating for female borderline and female comparison subjects (76% versus 34%) (χ2=42.52, df=1, p<0.00001), as well as for male borderline and male comparison subjects (65% versus 18%) (χ2=27.38, df=1, p<0.00001).
Table 3 shows the conditional probabilities of this pattern of complex comorbidity in our group of axis II patients. As can be seen, the pattern of complex comorbidity has a high degree of sensitivity, specificity, and positive predictive power. Looking only at positive predictive power, these data indicate that a pattern of complex comorbidity as we have defined it will successfully predict a borderline diagnosis 84%–90% of the time, depending on gender, in a group of nonpsychotic inpatients.
A broader definition of complex comorbidity (meeting criteria for a mood and/or anxiety disorder and a disorder of impulsivity) yielded a weaker model overall (χ2=33.41, df=1, p<0.00001). For the total group, this model had high sensitivity (100%) and positive predictive power (0.75) but no specificity or negative predictive power. Similar results were found for groups restricted to women (χ2=17.37, df=1, p<0.0001) and men (χ2=14.59, df=1, p=0.0001).
DISCUSSION
Four important findings emerge from this study. Our first major finding is that anxiety disorders were found to be only somewhat less common among borderline patients than mood disorders but far more frequently seen in borderline patients than in axis II comparison subjects. Over 90% of the borderline patients in this study met DSM-III-R criteria for a mood disorder. Mood disorders were also found to be significantly more common among borderline patients than axis II comparison subjects. These findings are consistent with those of most earlier studies (1–4, 8, 10–15). However, almost 90% of our borderline patients met DSM-III-R criteria for an anxiety disorder, while only about 50% of comparison subjects met anxiety disorder criteria. More specifically, about half of the borderline patients met DSM-III-R criteria for panic disorder, social phobia, or PTSD; about a third met DSM-III-R criteria for a simple phobia; and about a sixth met DSM-III-R criteria for agoraphobia, obsessive-compulsive disorder (OCD), and generalized anxiety disorder. These proportions were all smaller among the comparison subjects. In addition, anxiety disorders in general and panic disorder, social phobia, and PTSD in particular discriminated borderline patients from comparison subjects among both women and men.
These results extend the results of prior studies that have found a significant association between borderline personality disorder and anxiety disorders (2,12), since they demonstrate that anxiety disorders are both almost as common as mood disorders among borderline patients and far more discriminating. However, these results contradict the relatively low rates of anxiety disorder comorbidity found in most of the 11 studies that assessed anxiety disorder comorbidity at all (1, 2, 4–6, 8–10, 12, 14, 15). This discrepancy may be due to the fact that most of these 11 studies either assessed the presence of these disorders with unstructured methods of inquiry (i.e., chart review or clinical interview) (1, 6, 9, 14) or reported the rates of occurrence of only a few anxiety disorders, although their presence was assessed by semistructured research interview (2, 4, 5, 10, 12). Thus, the low-moderate degree of comorbidity between borderline personality disorder and anxiety disorders found in most previous studies that assessed this area of comorbidity may have been due to a failure to examine or report this area of phenomenology systematically.
These results suggest that clinicians should pay more attention to the anxiety symptoms and syndromes of their borderline patients. This is particularly so given the success of tricyclic antidepressants, selective serotonin reuptake inhibitors, and benzodiazepines in treating panic disorder, OCD, and social phobia (20–28) and the usefulness of cognitive behavioral techniques in treating the symptoms and behavioral sequelae of a number of the most common anxiety disorders (29, 30).
Our second major finding is that PTSD was found to be a common but not ubiquitous comorbid disorder among borderline patients. Overall, 56% of the borderline patients met DSM-III-R criteria for this disorder, with 61% of the female and 35% of the male borderline patients meeting criteria for PTSD. We also found that a significantly higher percentage of borderline patients of both genders met DSM-III-R criteria for this disorder than same-sex axis II comparison subjects.
Only two other studies have assessed this area of comorbidity. Koenigsberg and his colleagues (9) found that no borderline patient was given a primary axis I diagnosis of PTSD, which might suggest that clinicians saw other disorders, such as major depression, as being more important. Hudziak and his associates (8) found that 28% of a sample of female borderline outpatients met criteria for PTSD. This percentage is very different from the 61% of female borderline patients determined to satisfy PTSD criteria in the current study. It seems unlikely that this disparity in comorbidity rates is due to treatment status, since 75% of the borderline outpatients in the Hudziak et al. study (8) had been hospitalized at least once for psychiatric reasons. Rather, this difference is probably due to differences in the method of assessing the presence of borderline personality disorder. While both studies used the DIB-R to determine a patient’s study group assignment (17), we used the standard score of 8 (out of 10) as our cutoff, while Hudziak et al. (8) used the lower score of 7. By using a cutoff associated with a specificity of only 0.55, Hudziak et al. potentially included in their sample a substantial number of patients who would be classified as nonborderline by standard DIB-R criteria (17).
The high degree of comorbidity between borderline personality disorder and PTSD found in the current study is consistent with the results of numerous studies that have found that borderline patients often report traumatic childhood experiences (10, 31–39). However, the fact that the rate of PTSD among borderline patients was found to be substantially less than 100% is inconsistent with the theory that borderline personality disorder might better be conceptualized as a chronic form of PTSD (40). Even in this very disturbed group of borderline inpatients, almost half had never met criteria for PTSD. This finding, in turn, suggests that borderline personality disorder may have different etiologies in different subgroups of patients. In this regard, it has been variously hypothesized that the development of borderline personality disorder conforms to a diathesis-stress model (41) or is best explained by a multifactorial model (42,43). Either of these explanatory models is consistent with the data reported here. It may be that borderline patients who do not report a history of seriously traumatic events may have a stronger inborn temperamental vulnerability to the development of borderline personality disorder. It may also be that only some types of reported childhood trauma are associated with the development of comorbid borderline personality disorder and PTSD.
Our third major finding is that male and female borderline patients exhibited somewhat different patterns of axis I comorbidity. While a high percentage of borderline patients of both genders met DSM-III-R criteria for a mood disorder or an anxiety disorder or both, they differed in the type of disorder of impulse in which they “specialized.” More specifically, substance use disorders were found to be significantly more common in the histories of male than female borderline patients. In contrast, eating disorders, particularly eating disorder not otherwise specified, were found to be significantly more common in the histories of female than male borderline patients. This new finding is consistent with the clinical observation that male patients are typically overrepresented in substance abuse programs, while female patients are typically overrepresented in eating disorders programs. This is not to say that no male borderline patients meet criteria for eating disorders or that no female borderline patients meet criteria for substance use disorders. Indeed, we found that about half of our female borderline patients had abused substances at some point in their lives, while about a fifth of our male borderline patients had a history of serious eating disorders. However, about 40% more female than male borderline patients in this study had used food self-destructively, while about 25% more male than female borderline patients had used alcohol, drugs, or both self-destructively.
Our fourth major finding is that a pattern of complex comorbidity had strong positive predictive power for the borderline diagnosis. This is a particularly important finding because the number of multiple and shifting comorbid axis I disorders commonly experienced by borderline patients over the course of their lives has frequently made it difficult for clinicians to accurately diagnose and ultimately treat the underlying personality pathology. In contrast, our data indicate that the pattern of complex lifetime axis I comorbidity evidenced by borderline patients is a useful marker for the borderline diagnosis.
Our data also indicate that a pattern of meeting lifetime criteria for both a disorder of affect and a disorder of impulse has strong sensitivity and specificity for the borderline diagnosis. More specifically, about 75% of borderline patients exhibit this pattern of comorbidity, and about 75% of axis II comparison subjects do not. While previous reports have found that the subsyndromal phenomenology of borderline personality disorder is both highly characteristic and distinguishing (44,45), this study is the first to suggest that the pattern of axis I comorbidity reported by borderline patients is equally notable and discriminating.
This finding, in turn, lends a degree of support to the view that borderline personality disorder is a valid disorder, since it has a characteristic clinical picture that can be delimited from that of other axis II disorders (46). Alternatively, a history of a variety of axis I disorders, particularly if they had an early onset, may have a role in the development of what is commonly seen as borderline psychopathology.
The major limitation of the present study is that its results may not be generalizable to milder outpatient cases of borderline personality disorder. While previous studies have found that a substantial percentage of borderline outpatients have previously been hospitalized (47, 48), the results of this study may not be applicable to borderline patients with very mild forms of the disorder.
Taken together, the results of this study suggest that the axis I comorbidity of borderline personality disorder follows a pattern of complexity that clinicians can use as a marker for underlying borderline psychopathology. The use of this marker may, in turn, lead to more accurate diagnosis of and more effective treatment planning for patients with borderline personality disorder.
Received Sept. 10, 1997; revision received March 12, 1998; accepted July 9, 1998. From the Laboratory for the Study of Adult Development, McLean Hospital; and the Department of Psychiatry, Harvard Medical School, Boston. Address reprint requests to Dr. Zanarini, McLean Hospital, 115 Mill St., Belmont, MA 02478; [email protected] (e-mail). Supported in part by NIMH grant MH-47588.
 |
 |
 |
1. Akiskal HS: Subaffective disorders: dysthymic, cyclothymic and bipolar II disorders in the “borderline” realm. Psychiatr Clin North Am 1981; 4:25–46Crossref, Medline, Google Scholar
2. Alnaes R, Torgersen S: The relationship between DSM-III symptom disorders (axis I) and personality disorders (axis II) in an outpatient population. Acta Psychiatr Scand 1988; 78:485–492Crossref, Medline, Google Scholar
3. Andrulonis PA, Vogel NG: Comparison of borderline personality subcategories to schizophrenic and affective disorders. Br J Psychiatry 1984; 144:358–363Crossref, Medline, Google Scholar
4. Coid JW: An affective syndrome in psychopaths with borderline personality disorder. Br J Psychiatry 1993; 162:641–650Crossref, Medline, Google Scholar
5. Dahl AA: Some aspects of the DSM-III personality disorders illustrated by a consecutive sample of hospitalized patients. Acta Psychiatr Scand Suppl 1986; 328:61–67Crossref, Medline, Google Scholar
6. Frances A, Clarkin JF, Gilmore M, Hurt SW, Brown R: Reliability of criteria for borderline personality disorder: a comparison of DSM-III and the Diagnostic Interview for Borderline Patients. Am J Psychiatry 1984; 141:1080–1084Link, Google Scholar
7. Fyer MF, Frances AJ, Sullivan T, Hurt SW, Clarkin J: Comorbidity of borderline personality disorder. Arch Gen Psychiatry 1988; 45:348–352Crossref, Medline, Google Scholar
8. Hudziak JJ, Boffeli TJ, Kriesman JJ, Battaglia MM, Stanger C, Guze SB: Clinical study of the relation of borderline personality disorder to Briquet’s syndrome (hysteria), somatization disorder, antisocial personality disorder, and substance abuse disorders. Am J Psychiatry 1996; 153:1598–1606Link, Google Scholar
9. Koenigsberg HW, Kaplan RD, Gilmore MM, Cooper AM: The relationship between syndrome and personality disorder in DSM-III: experience with 2,462 patients. Am J Psychiatry 1985; 142:207–212Link, Google Scholar
10. Links PS, Steiner M, Offord DR, Eppel A: Characteristics of borderline personality disorder: a Canadian study. Can J Psychiatry 1988; 33:336–340Crossref, Medline, Google Scholar
11. McGlashan TH: The borderline syndrome, II: is it a variant of schizophrenia or affective disorder? Arch Gen Psychiatry 1983; 40:1319–1323Google Scholar
12. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Doidge N, Rosnick L, Gallaher PE: Comorbidity of axis I and axis II disorders. Am J Psychiatry 1995; 152:571–578Link, Google Scholar
13. Perry JC, Cooper SH: Psychodynamics, symptoms, and outcome in borderline and antisocial personality disorders and bipolar type II affective disorder, in The Borderline: Current Empirical Research. Edited by McGlashan TH. Washington, DC, American Psychiatric Press, 1985, pp 21–41Google Scholar
14. Pope HG, Jonas JM, Hudson JI, Cohen BM, Gunderson JG: The validity of DSM-III borderline personality disorder. Arch Gen Psychiatry 1983; 40:23–30Crossref, Medline, Google Scholar
15. Zanarini MC, Gunderson JG, Frankenburg FR: Axis I phenomenology of borderline personality disorder. Compr Psychiatry 1989; 30:149–156Crossref, Medline, Google Scholar
16. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R, Version 1.0 (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
17. Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL: The Revised Diagnostic Interview for Borderlines: discriminating BPD from other Axis II disorders. J Personality Disorders 1989; 3:10–18Crossref, Google Scholar
18. Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG: The Diagnostic Interview for Personality Disorders: interrater and test-retest reliability. Compr Psychiatry 1987; 28:467–480Crossref, Medline, Google Scholar
19. Hollingshead AB: Two-Factor Index of Social Position. New York, Psychological Corp, 1957Google Scholar
20. Griest J, Chouinard G, DuBoff E, Halaris A, Kim SW, Koran L, Liebowitz M, Lydiard RB, Rasmussen S, White K, Sikes C: Double-blind parallel comparison of three doses of sertraline and placebo in outpatients with obsessive-compulsive disorder. Arch Gen Psychiatry 1995; 52:289–295Crossref, Medline, Google Scholar
21. Tollefson GD, Rampey AH, Potvin JH, Jenike MA, Rush AJ, Dominguez RA, Koran LM, Shear MK, Goodman W, Genduso LA: A multicenter investigation of fixed-dose fluoxetine in the treatment of obsessive-compulsive disorder. Arch Gen Psychiatry 1994; 51:559–567Crossref, Medline, Google Scholar
22. Zohar J, Judge R, OCD Paroxetine Study Investigators: Paroxetine versus clomipramine in the treatment of obsessive-compulsive disorder. Br J Psychiatry 1996; 169:468–474Crossref, Medline, Google Scholar
23. Beauclair L, Fontaine R, Annable L, Holobow N, Chouinard G: Clonazepam in the treatment of panic disorder: a double-blind, placebo-controlled trial investigating the correlation between clonazepam concentration in plasma and clinical response. J Clin Psychopharmacol 1994; 14:111–114Crossref, Medline, Google Scholar
24. Chouinard G, Annable L, Fontaine R, Solyom L: Alprazolam in the treatment of generalized anxiety and panic disorders: a double-blind, placebo-controlled study. Psychopharmacology (Berl) 1982; 77:229–233Crossref, Medline, Google Scholar
25. Jefferson JW: Antidepressants in panic disorder. J Clin Psychiatry 1997; 58(suppl 2):20–24Google Scholar
26. Oehrberg S, Christensen PE, Behnke K, Borup AL, Severin B, Soegaard J, Calberg H, Judge R, Ohstrom JK, Manniche PM: Paroxetine in the treatment of panic disorder: a randomized double-blind, placebo-controlled study. Br J Psychiatry 1995; 167:373–379Crossref, Google Scholar
27. Mancini C, Van Amerigen M: Paroxetine in social phobia. J Clin Psychiatry 1996; 57:519–522Crossref, Medline, Google Scholar
28. Rosenbaum JF, Pollack RA: The psychopharmacology of social phobia and comorbid disorders. Bull Menninger Clin 1994; 52(suppl A):67–83Google Scholar
29. Gould RA, Otto MW, Pollack MH: A meta analysis of treatment outcome for panic disorder. Clin Psychol Rev 1995; 15:819–844Crossref, Google Scholar
30. Christensen H, Hadzi-Pavlovi D, Andrews G, Mattick R: Behavior therapy and tricyclic medication in the treatment of obsessive-compulsive disorder. J Consult Clin Psychol 1987; 55:701–711Crossref, Medline, Google Scholar
31. Herman JL, Perry JC, van der Kolk BA: Childhood trauma in borderline personality disorder. Am J Psychiatry 1989; 146:490–495Link, Google Scholar
32. Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM: Childhood sexual and physical abuse in adult patients with borderline personality disorder. Am J Psychiatry 1990; 147:1008–1013Link, Google Scholar
33. Paris J, Zweig-Frank H, Guzder J: Psychological risk factors for borderline personality disorder in female patients. Compr Psychiatry 1994; 35:301–305Crossref, Medline, Google Scholar
34. Paris J, Zweig-Frank H, Guzder J: Risk factors for borderline personality in male outpatients. J Nerv Ment Dis 1994; 182, 375–380Google Scholar
35. Salzman JP, Salzman C, Wolfson AN, Albanese M, Looper J, Ostacher M, Schwartz J, Chinman G, Land W, Miyawaki E: Association between borderline personality structure and history of childhood abuse in adult volunteers. Compr Psychiatry 1993; 34:254–257Crossref, Medline, Google Scholar
36. Shearer SL, Peters CP, Quaytman MS, Ogden RL: Frequency and correlates of childhood sexual and physical abuse histories in adult female borderline inpatients. Am J Psychiatry 1990; 147:214–216Link, Google Scholar
37. Westen D, Ludolph P, Misle B, Ruffins S, Block J: Physical and sexual abuse in adolescent girls with borderline personality disorder. Am J Orthopsychiatry 1990; 60:55–66Crossref, Medline, Google Scholar
38. Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR: Childhood experiences of borderline patients. Compr Psychiatry 1989; 30:18–25Crossref, Medline, Google Scholar
39. Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, Levin A, Yong L, Frankenburg FR: Reported pathological childhood experiences associated with the development of borderline personality disorder. Am J Psychiatry 1997; 154:1101–1106Link, Google Scholar
40. Herman JL, van der Kolk BA: Traumatic antecedents of borderline personality disorder, in Psychological Trauma. Edited by van der Kolk BA. Washington, DC, American Psychiatric Press, 1987, pp 111–126Google Scholar
41. Stone MH: The Borderline Syndromes: Constitution, Personality, and Adaptation. New York, McGraw-Hill, 1980Google Scholar
42. Paris J: Personality disorders: a biopsychosocial model. J Personality Disorders 1993; 7:255–264Crossref, Google Scholar
43. Zanarini MC, Frankenburg FR: Pathways to the development of borderline personality disorder. J Personality Disorders 1997; 11:93–104Crossref, Google Scholar
44. Gunderson JG, Kolb JE: Discriminating features of borderline patients. Am J Psychiatry 1978; 135:792–796Link, Google Scholar
45. Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL: Discriminating borderline personality disorder from other axis II disorders. Am J Psychiatry 1990; 147:161–167Link, Google Scholar
46. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983–987Link, Google Scholar
47. Skodol AE, Buckley P, Charles E: Is there a characteristic pattern to the treatment history of clinic outpatients with borderline personality? J Nerv Ment Dis 1983; 171:405–410Google Scholar
48. Swartz M, Blazer D, George L, Winfield I: Estimating the prevalence of borderline personality disorder in the community. J Personality Disorders 1990; 4:257–272Crossref, Google Scholar



