A Meta-Analysis of Head-to-Head Comparisons of Second-Generation Antipsychotics in the Treatment of Schizophrenia
Abstract
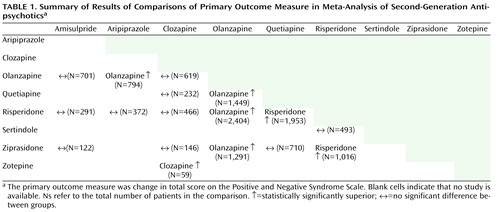
Objective: Whether there are differences in efficacy among second-generation antipsychotics in the treatment of schizophrenia is a matter of heated debate. The authors conducted a systematic review and meta-analysis of blinded studies comparing second-generation antipsychotics head-to-head. Method: Searches of the Cochrane Schizophrenia Group’s register (May 2007) and MEDLINE (September 2007) were conducted for randomized, blinded studies comparing two or more of nine second-generation antipsychotics in the treatment of schizophrenia. All data were extracted by at least three reviewers independently. The primary outcome measure was change in total score on the Positive and Negative Syndrome Scale; secondary outcome measures were positive and negative symptom subscores and rate of dropout due to inefficacy. The results were combined in a meta-analysis. Various sensitivity analyses and metaregressions were used to examine bias. Results: The analysis included 78 studies with 167 relevant arms and 13,558 participants. Olanzapine proved superior to aripiprazole, quetiapine, risperidone, and ziprasidone. Risperidone was more efficacious than quetiapine and ziprasidone. Clozapine proved superior to zotepine and, in doses >400 mg/day, to risperidone. These differences were due to improvement in positive symptoms rather than negative symptoms. The results were rather robust with regard to the effects of industry sponsorship, study quality, dosages, and trial duration. Conclusions: The findings suggest that some second-generation antipsychotics may be somewhat more efficacious than others, but the limitations of meta-analysis must be considered. In tailoring drug treatment to the individual patient, small efficacy superiorities must be weighed against large differences in side effects and cost.
Drug choice in the treatment of schizophrenia has been controversial. Second-generation antipsychotic drugs, which have a low propensity to cause extrapyramidal side effects, were introduced in the 1990s. As their cost represents a large proportion of mental health budgets, totaling $11.7 billion in the United States in 2005 (1) , there is a debate as to their superior effectiveness compared with lower-cost first-generation antipsychotics, such as haloperidol. Meta-analyses have shown that some second-generation antipsychotics (amisulpride, clozapine, olanzapine, and risperidone) are more efficacious than first-generation antipsychotics (2 , 3) . Some evidence suggests that even these superiorities may be due to an inappropriate choice of the comparator first-generation antipsychotic, the dosage of the comparator antipsychotic, or lack of prophylactic antiparkinson medication (4 , 5) . Despite these controversies, second-generation antipsychotics have become the most frequently prescribed drugs in some countries, including the United States. The question of whether there are efficacy differences between these drugs thus becomes very important.
The Cochrane Handbook notes that because of a multiplicity of possible confounders, indirect comparisons derived from meta-analyses comparing second-generation antipsychotics with first-generation antipsychotics do not provide firm proof for an efficacy difference between second-generation antipsychotics (6) . The stakes are high for patients, because the four second-generation antipsychotics that have turned out to be more efficacious than first-generation antipsychotics in meta-analyses either commonly induce substantial weight gain (clozapine and olanzapine [7] ) or substantially increase prolactin levels (amisulpride and risperidone [8] ). Side effects are very important, but on the other hand, because schizophrenia is a disease that lasts throughout life, and so even a small increment in efficacy could increase the patient’s chances of leading a more normal life. In this context, we present a meta-analysis of blinded trials comparing each second-generation antipsychotic against other second-generation antipsychotics.
Method
Search
We searched the Cochrane Schizophrenia Group’s (CSG) register for randomized, at least single-blind trials with all 36 possible head-to-head comparisons of nine second-generation antipsychotics in the treatment of schizophrenia or related disorders (schizoaffective, schizophreniform, or delusional disorder, any diagnostic criteria). Two reviewers independently inspected all reports. The last search of the CSG register was made in May 2007. We also searched MEDLINE through September 2007. The CSG register is compiled by regular searches of electronic databases (BIOSIS, CINAHL, Dissertation Abstracts, EMBASE, LILACS, MEDLINE, PSYNDEX, PsycINFO, RUSSMED, Sociofile), supplemented by the hand searching of journals and conference proceedings (9) . All manufacturers of second-generation antipsychotics were contacted for further studies. Only studies that met the Cochrane Handbook ’s quality criterion A or B were included (6) . Nonblinded studies were excluded because we found that open studies favored the sponsor (3) . There were no language restrictions.
Data Extraction and Outcomes
All data were extracted independently by at least three reviewers (S.L., K.K., C.R.-K., H.H., F.S., C.A.L., S.S.). The primary outcome measure was change in total score on the Positive and Negative Syndrome Scale (PANSS); secondary outcomes measures were positive and negative symptom subscores as well as rate of dropout due to insufficient efficacy. Results based on mixed-effects models and last-observation-carried-forward results were preferred to completer analyses, but when only the latter were available, they were used. First authors and manufacturers were contacted for missing data.
Meta-Analytic Calculations
We analyzed continuous outcomes using weighted (by N) mean differences and their 95% confidence interval (CI), since this preserves the original PANSS units, which are intuitively interpreted (e.g., a weighted mean difference of 5 means a 5-point difference in PANSS score between the two groups). For sensitivity analyses, we used the standardized effect size Hedges’ g to include a few more studies (13.3%) that used scales other than the PANSS. For missing standard deviations, we either derived them from other statistics or used the average standard deviations of the other studies. Risk ratios were used for the dichotomous measure. Number needed to treat was calculated as the inverse of the risk difference where appropriate. The studies were pooled with the random-effects model of Der-Simonian and Laird (10) . We explored study heterogeneity by a chi-square test of homogeneity.
Addressing Potential Moderator and Quality Variables
Unrestricted-maximum-likelihood-random-effects metaregression was used to assess the effects of mean daily dose, dose ratio, study quality as rated by the Jadad et al. scale (11) , study duration, and pharmaceutical company sponsorship on the primary outcome measure.
All studies were included in the main analysis. In secondary analyses of the primary outcome, we excluded studies with certain characteristics that could have biased the results. This procedure, referred to as sensitivity analysis in meta-analysis, addresses the robustness of the results. We excluded studies that were sponsored by manufacturers of the drugs being compared, single-blind studies, lower-quality studies (Jadad score <3 [11] ), first-episode studies, effectiveness studies, studies from phase 2 of the Clinical Antipsychotic Trials in Intervention Effectiveness (CATIE) study (the same subjects as those in phase 1 were rerandomized [ 12 , 13 ]), and Chinese studies (because of potential ethnic differences in metabolism or differences in methodological rigor). We also addressed first-episode studies and treatment-resistant populations separately; we analyzed studies with clozapine dosages above 400 mg/day separately; and we analyzed clozapine studies of at least 3 or 6 months’ duration separately. We used a fixed-effects model instead of the random-effects model.
Pharmaceutical companies sometimes do not publish studies that did not favor their drug. We used funnel plots (14) and Orwin’s fail-safe method (15) to estimate whether such a publication bias exists.
All calculations were made with Stata, release 7 (Stata Corp., College Station, Tex.), and Comprehensive Meta-Analysis, version 2 (16) . All analyses were two-tailed with alpha set at 0.05 without adjustments for multiple comparisons, except for the homogeneity test, in which alpha was set to 0.1. (More information is provided in the data supplement that accompanies the online edition of this article.)
Results
The search yielded 3,620 citations. Of 612 studies inspected, 319 were excluded: 44 studies with no or inadequate randomization; 23 studies with no appropriate drug group; 230 open-label studies (181 from China); one study with inappropriate participants; six studies with no usable data; and 15 studies that used groups of second-generation antipsychotics. We included 293 publications on 78 studies with 167 relevant arms and 13,558 participants (only the principal publications are referenced). Nine studies included amisulpride, four aripiprazole, 28 clozapine, 48 olanzapine, 21 quetiapine, 44 risperidone, two sertindole, nine ziprasidone, and two zotepine.
Forty-nine studies were mainly sponsored by pharmaceutical companies, and 22 were publicly funded; funding was uncertain for seven studies despite written queries. The participants had relatively chronic courses of illness, with mean ages in the mid-30s, but five trials included only first-episode patients. The diagnostic criteria used were mainly those of DSM-III-R, DSM-IV, and ICD-10 (for details, see the online data supplement).
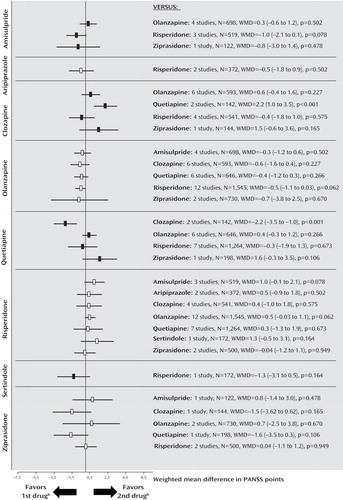
Primary Outcome Measure: PANSS Total Score
The pooled effect sizes of each second-generation antipsychotic versus every other one are shown in Figure 1 (forest plots with the single studies can be found in the online data supplement). It should be noted that all results are shown twice. For example, the comparison between amisulpride and olanzapine is described under “amisulpride versus other second-generation antipsychotics” as well as under “olanzapine versus other second-generation antipsychotics.” Despite the redundancy, the results are easier to understand in this format; otherwise the reader interested in a given drug would have to look up the findings in different sections, making it difficult to see the gestalt. To save space, we present here, for the significant results, only the number of participants combined for the two second-generation antipsychotics compared, the difference in PANSS scores (weighted mean difference), and the p value, and, for nonsignificant results, the number of participants combined for the two second-generation antipsychotics compared. Negative values mean superiority of the first second-generation antipsychotic throughout. All statistical details are presented in figures and tables. The data were rather homogeneous, and the few cases of significant heterogeneity are reported in the text.
a Numbers in parentheses are 95% confidence intervals. WMD=weighted mean difference.
b Data based on Brief Psychiatric Rating Scale.
c The first drug is the one written vertically on the left side, and the second is the one written horizontally on the right side of the graph.
Amisulpride
There were no significant differences between amisulpride and olanzapine (N=701), risperidone (N=291), and ziprasidone (N=122).
Aripiprazole
Aripiprazole was less efficacious than olanzapine in two studies sponsored by aripiprazole’s manufacturer (N=794, weighted mean difference=5.0, p=0.002). Two further studies found no significant difference compared with risperidone (N=372).
Clozapine
Clozapine was not significantly different from olanzapine (N=619), quetiapine (N=232), risperidone (N=466), and ziprasidone (N=146). Clozapine was significantly more efficacious than zotepine (N=59, weighted mean difference=–6.0, p=0.002). The comparison with risperidone was significantly heterogeneous due to one study sponsored by clozapine’s manufacturer (17) ; excluding the study did not change the overall results.
Olanzapine
Olanzapine was significantly more efficacious than aripiprazole (N=794, weighted mean difference=–5.0, p=0.002), quetiapine (N=1,449, weighted mean difference=–3.7, p<0.001), risperidone (N=2,404, weighted mean difference=–1.9, p=0.006), and ziprasidone (N=1,291, weighted mean difference=–8.3, p<0.001). No significant difference between olanzapine and amisulpride (N=701) or clozapine (N=619) emerged.
Quetiapine
Quetiapine was significantly less efficacious than olanzapine (N=1,449, weighted mean difference=3.7, p<0.001) and risperidone (N=1,953, weighted mean difference=3.2, p=0.003). There was no significant difference compared with clozapine (N=232) and ziprasidone (N=710).
Risperidone
Risperidone was significantly more efficacious than quetiapine (N=1,953, weighted mean difference=–3.2, p=0.003) and ziprasidone (N=1,016, weighted mean difference=–4.6, p=0.002). It was less efficacious than olanzapine (N=2,404, weighted mean difference=1.9, p=0.006). No difference compared with amisulpride (N=291), aripiprazole (N=372), clozapine (N=466), and sertindole (N=493) emerged.
Sertindole
There was no significant difference between sertindole and risperidone in two studies sponsored by sertindole’s manufacturer, one in treatment-resistant patients, which found results with risperidone to be 7 points better, the other without this criterion finding sertindole 3.5 points better (N=493), leading to significant heterogeneity.
Ziprasidone
Ziprasidone was less efficacious than olanzapine (N=1,291, weighted mean difference=8.3, p<0.001) and risperidone (N=1,016, weighted mean difference=4.6, p=0.002). No significant differences compared with amisulpride (N=122), clozapine (N=146), and quetiapine (N=710) were found.
Zotepine
Zotepine was less efficacious than clozapine (N=59, weighted mean difference=6.0, p=0.002).
Secondary Outcomes: Positive and Negative Symptoms
The findings suggest that a substantial portion of the efficacy differences was due to superior improvement in positive symptoms. Results for positive symptoms paralleled those found for overall symptoms except that olanzapine was not significantly more efficacious than risperidone ( Figure 2 ; see also the online data supplement). There were no significant differences for negative symptoms, with the exception of a superiority of quetiapine compared with clozapine in two small Chinese studies of first-episode schizophrenia ( Figure 3 ). The comparisons of quetiapine with risperidone and olanzapine with ziprasidone were heterogeneous, and the results did not change when outliers were excluded (see also the online data supplement).
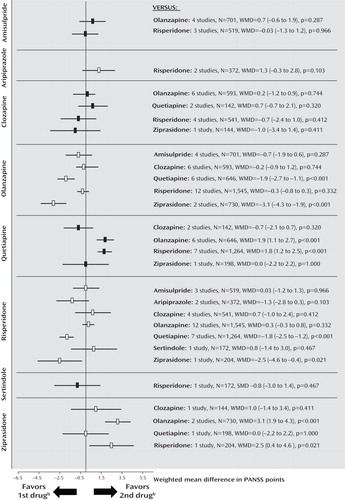
a Numbers in parentheses are 95% confidence intervals. WMD=weighted mean difference.
b The first drug is the one written vertically on the left side, and the second is the one written horizontally on the right side of the graph.
a Numbers in parentheses are 95% confidence intervals. WMD=weighted mean difference.
b The first drug is the one written vertically on the left side, and the second is the one written horizontally on the right side of the graph.
Dropout Due to Inefficacy of Treatment
The rates of dropout due to poor efficacy were consistent with the primary outcome measure, except that clozapine was significantly more effective than risperidone, and amisulpride was superior to ziprasidone. Furthermore, there was no significant difference in a single study comparing aripiprazole and olanzapine, and no significant difference between risperidone and ziprasidone ( Figure 4 ; see also the online data supplement).
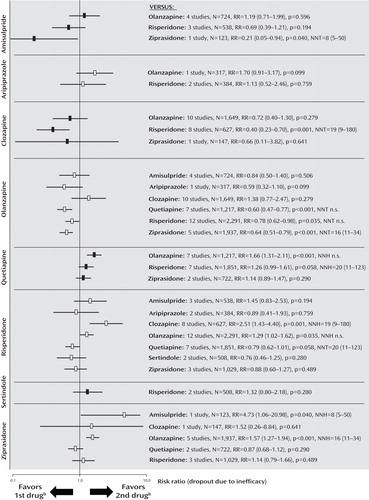
a Numbers in parentheses are 95% confidence intervals. RR=risk ratio; NNT/NNH=number needed to treat/number needed to harm; n.s.=not significant.
b The first drug is the one written vertically on the left side, and the second is the one written horizontally on the right side of the graph.
Metaregressions
Metaregression did not detect significant effects of study duration, antipsychotic dosages or dose ratios, or study quality. Nor were there significant effects for sponsorship, with the exception of clozapine versus risperidone (coefficient=6.3 in the expected direction, p=0.015).
Sensitivity Analyses
The results of the extensive sensitivity analyses (pharmaceutical sponsorship, single-blind studies, lower-quality studies, effectiveness studies, CATIE phase 2, first-episode studies, Chinese studies, etc.) did not alter the primary findings (see the online data supplement). The important results are summarized below.
Pharmaceutical sponsorship and study quality
Excluding studies sponsored by pharmaceutical companies (see the online data supplement) or excluding studies with a Jadad quality score <3 did not change the results.
First-episode and treatment-resistant populations
The five first-episode studies showed no difference between second-generation antipsychotics. Most studies of treatment-resistant patients involved clozapine, which was not more efficacious than olanzapine (N=7, N=570, weighted mean difference=–0.2, 95% CI=–3.6 to 3.2), risperidone (N=5, N=471, weighted mean difference=–1.3, 95% CI=–5.8 to 3.2) or ziprasidone (N=1, N=146, weighted mean difference=0.5, 95% CI=–6.7 to 7.7).
Clozapine dose
In studies with mean clozapine dosages above 400 mg/day, clozapine was superior to risperidone (N=2, N=335, weighted mean difference=–6.6, 95% CI=–11.5 to –1.7), but not olanzapine (N=2, N=154, weighted mean difference=2.4, 95% CI=–2.4 to 7.3). There were no data for other drugs.
Sensitivity analysis using Hedges’ g
The only change when adding studies using scales other than the PANSS (using Hedges’ g) was that amisulpride was significantly more efficacious than risperidone for negative symptoms (see the online data supplement).
Publication bias
Funnel plots failed to detect publication bias. The fail-safe number of unpublished studies that would make the results no longer statistically significant was a median of 19 (see the online data supplement).
Discussion
This the first meta-analysis of the efficacy of all second-generation antipsychotics in randomized trials that compare two or more of these agents head-to-head. The main results are summarized in Table 1 , and selected side effects are summarized in Table 2 . Olanzapine was more efficacious than aripiprazole, quetiapine, risperidone, and ziprasidone, and its efficacy was similar to that of amisulpride and clozapine. Risperidone was less efficacious than olanzapine, but more efficacious than quetiapine and ziprasidone. The pattern of superior outcomes in terms of positive symptoms subscore and dropouts due to inefficacy paralleled that of the PANSS total score, whereas there was little difference on negative symptom score. The findings are similar to those in phase 1 of CATIE (olanzapine > [risperidone=quetiapine=ziprasidone]) for its efficacy measures—time to dropout due to poor efficacy, time with good response, and PANSS total score (4) . They are also consistent with meta-analyses comparing second-generation antipsychotics with first-generation antipsychotics (2 , 3 , 21) . In the most recent of these (3) , the following pattern emerged: clozapine (Hedges’ g=–0.52), amisulpride (Hedges’ g=–0.31), olanzapine (Hedges’ g=–0.28), and risperidone (Hedges’ g=–0.13) were significantly more efficacious than first-generation antipsychotics, while aripiprazole, quetiapine, ziprasidone, and zotepine were only as efficacious as the older drugs. Thus, the only clear deviation was that we expected better results from clozapine, which was only more efficacious than zotepine, and more efficacious than risperidone in terms of dropout due to inefficacy.
The results were remarkably consistent, although the studies were sponsored by different companies. Our recent analysis (22) using blind raters showed that pharmaceutical sponsors highlight the benefits of their own second-generation antipsychotics in the abstract. In meta-analysis, the outcomes that will be presented are predefined, which avoids the selective presentation of favorable results. Indeed, Davis et al. (23) recently extracted data in a predefined manner and found no industry bias in comparing the numerical results of industry-sponsored and non-industry-sponsored studies. We performed sensitivity analyses and metaregressions with sponsor, dose, study quality, treatment resistance, study origin, and trial duration as moderators and found only a few differences. We also included only blinded randomized trials because we recently found that lack of blinding can clearly bias the results in this competitive area (3) .
The analysis of positive and negative symptom subscores on the PANSS suggested that most of the differences between drugs were due to positive symptoms rather than negative symptoms. Many studies selected patients with predominantly positive symptoms, and this design may be less sensitive for detecting negative symptom changes. The results based on dropouts due to insufficient efficacy were by and large consistent with results on the primary outcome measure. The few first-episode studies found no differences between agents. Such patients differ substantially from multiepisode patients, and more research on treatment of this population is needed.
Most studies available for analysis involved olanzapine (N=48), followed by risperidone (N=44), clozapine (N=28), and quetiapine (N=21), while few or no studies compared the other second-generation antipsychotics against one another (see the online data supplement). For example, since amisulpride was not distinguishable in efficacy from olanzapine and risperidone—which is consistent with amisulpride’s better efficacy compared with first-generation antipsychotics (2 , 3 , 21) —comparisons with other second-generation antipsychotics would be essential to verify that it really is a more effective second-generation antipsychotic, as suggested by the open randomized European First-Episode Schizophrenia Trial (24) . In the only comparison with ziprasidone at full dosage (sponsored by its manufacturer), amisulpride was given in low doses (100–200 mg/day), and positive symptoms were omitted from the report (25) . Nevertheless, amisulpride was superior in terms of dropouts due to inefficacy.
In our opinion, clozapine is a more efficacious drug because it has consistently been shown to be more effective than first-generation antipsychotics (2 , 21 , 26) , as well as other second-generation antipsychotics in CATIE phase 2 and in the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS), which could not be included here (12 , 13 , 27) . The clozapine group of CATIE phase 2 was a nonblinded study arm (12) , and CUtLASS compared clozapine with a number of second-generation antipsychotics as a group. Weekly blood tests in the clozapine group may have improved monitoring (27) . Clinical experience, including relapses when patients are switched from clozapine and antisuicidal properties of clozapine, also suggests its superiority (28) .
The most likely explanation for not finding clozapine superior here is that most studies used low or very low clozapine dosages; five used dosages under about 210 mg/day, and several had an upper limit of 400 mg/day. In the few studies in which mean dosages exceeded 400 mg/day, clozapine was more efficacious than risperidone. In two pivotal studies (29 , 30) demonstrating clozapine’s superiority to first-generation antipsychotics, the mean dosages were 600 mg/day and 523 mg/day. Randomized, blinded dose-finding studies (in which a dosage of 600 mg/day was found to be best [31] ) and our review of five controlled plasma-level studies (32) showed that low clozapine dosages do not produce results as good as high dosages. Clozapine requires slow titration and a long enough trial (33) , but most studies in our meta-analysis were relatively long, and metaregression/sensitivity analyses of studies lasting at least 3 or 6 months did not show a superiority of clozapine. The sensitivity analysis of treatment-resistant patients failed to show a superiority of clozapine, but the criteria varied and the patients may not have been as refractory as those in the pivotal studies (29 , 30) . Hardly any studies had a run-in phase to confirm refractoriness.
Meta-analysis can only reflect (and be as good as) the underlying studies. Since 20 of 22 studies did not find clozapine superior (the exceptions were references 17 and 34 ), a narrative review would have reached similar conclusions. Our finding taken together with the dose-response findings tentatively suggests that relatively high doses of clozapine might be needed for some patients. A sufficiently powered double-blind independent study with high dosages in treatment-refractory patients is needed.
Many limitations of meta-analyses must be considered in assessing our findings. In essence, meta-analysis is an observational technique based on originally controlled studies. The studies are a sample from a hypothetical population of studies, and all depends on how well they represent the population. Meta-analysis summarizes similar but not identical studies, and despite extensive sensitivity analyses, the “averaging apples with oranges” (heterogeneity) problem can never be fully ruled out. For example, we combined studies using different statistics (e.g., last observation carried forward, mixed models). Missing standard deviations had to be estimated from the other studies. Adjustments for multiple testing are usually not made in meta-analyses, but because of the many tests applied, a number of findings may well be due to chance alone, although most were consistent across measures (PANSS total and positive symptom scores, dropout due to inefficacy). In contrast, many comparisons of the less studied second-generation antipsychotics were underpowered. The statistical power of metaregression is especially weak, one reason being that it analyzes the influence of moderators at the level of studies rather than of patients.
What are the implications of our findings for the choice of drug? First, we must consider the magnitude of the efficacy differences. We found the effect sizes to range between 1.9 (olanzapine versus risperidone) and 8.3 (olanzapine versus ziprasidone) PANSS points, or 0.11 to 0.29 effect size units. These effect sizes are small to medium differences according to Cohen’s classification (35) . The clinical relevance of the difference between olanzapine and risperidone (effect size 0.11) based on a large sample size (N=2,404) is especially doubtful. For perspective, the average difference between second-generation antipsychotics and placebo in a recent meta-analysis was only 10 PANSS points and the effect size was 0.51 (20) . To a certain extent, the advantage of one over another second-generation antipsychotic can be viewed in the context of the antipsychotic-placebo difference of 10 PANSS points, but we would hasten to add that this is an indirect and imprecise comparison, particularly considering the differences between active-control trials and placebo-control trials (e.g., reference 36 ). On the other hand, schizophrenia afflicts patients for life, and even a small benefit may be important.
Second, exploding health care costs are making the price of medication important, and some second-generation antipsychotics (amisulpride, risperidone, and zotepine), as well as the first-generation antipsychotics, are now off patent.
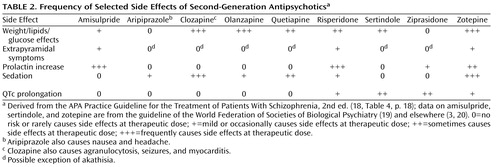
Third, side effects are extremely important in choice of drug, because the efficacy of a medication can be interpreted only in the context of its adverse effect profile. There are many side effects that we would have to analyze in 36 possible drug comparisons. Some of these side effects are measured in several ways, and we would have to do a number of metaregressions. It would not be possible to present the resulting information in one paper. Rare side effects would require epidemiological databases. The large differences in side effects among second-generation antipsychotics are well known. As summarized in the APA Practice Guideline for the Treatment of Patients With Schizophrenia, Second Edition (18) , clozapine and olanzapine are the most likely to lead to weight gain and glucose and lipid abnormalities (see Table 2 ), followed by quetiapine and then risperidone (see also references 7 , 37 , 38) . Aripiprazole and ziprasidone are relatively benign. There can be dramatic consequences, such as type 2 diabetes, diabetic ketoacidosis, heart attack, and stroke. Extrapyramidal symptoms and tardive dyskinesia are important (see reference 39 for a review). Amisulpride and risperidone carry a risk of some dose-related extrapyramidal symptoms and substantial increase in prolactin levels (more so than haloperidol [40] ), which can be associated with osteoporosis, galactorrhea, amenorrhea, and sexual dysfunction. The use of clozapine is restricted to refractory patients because of the risk of agranulocytosis, but it also carries a risk of seizures, anticholinergic effects, constipation, sedation, postural hypotension, hypersalivation, myocarditis, and pancreatitis. Sertindole and ziprasidone carry the strongest risk of QTc prolongation among second-generation antipsychotics. Large differences in side effects are often more important than small efficacy differences for individual patients. The clinician should also consider the patient’s past treatment responses, including efficacy and adverse events, the patient’s preferences, and medical vulnerabilities, including family history. For example, olanzapine would not be a first choice for a patient with a vulnerability to diabetes, and the high risk of weight gain does not make it a drug for every patient. Finally, there are substantial differences between individual patients in how they respond to these drugs. The balancing of efficacy and side effects must be tailored to the individual patient, the setting, and the health system.
1. Vital signs. Clin Psychiatr News 2007; 35:1Google Scholar
2. Davis JM, Chen N, Glick ID: A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 2003; 60:553–564Google Scholar
3. Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM: A meta-analysis comparing second-generation and first-generation antipsychotics for placebo. Lancet (in press)Google Scholar
4. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RSE, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK: Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353:1209–1223Google Scholar
5. Leucht S, Wahlbeck K, Hamann J, Kissling W: New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003; 361:1581–1589Google Scholar
6. Higgins JPT, Green S (eds): Cochrane Handbook for Systematic Reviews of Interventions 4.2.5, in The Cochrane Library, issue 3, 2005. Chichester, UK, John Wiley & Sons, 2005Google Scholar
7. Newcomer JW: Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 2005; 19:1–93Google Scholar
8. Haddad PM, Wieck A: Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features, and management. Drugs 2004; 64:2291–2314Google Scholar
9. Adams CE, Coutinho E, Davis JM, Duggan L, Lee C, Leucht S, Tharyan P: Cochrane Schizophrenia Group, in The Cochrane Library. Chichester, UK, John Wiley & Sons, 2006Google Scholar
10. Der-Simonian R, Laird N: Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177–188Google Scholar
11. Jadad A, Moore A, Carroll D, Jenkinson C, Reynolds DJM, Gavanagh DJ, McQuay HJ: Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17:1–12Google Scholar
12. McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, Swartz MS, Perkins DO, Keefe RSE, Davis CE, Severe J, Hsiao JK, CATIE Investigators: Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry 2006; 163:600–610Google Scholar
13. Stroup TS, Lieberman JA, McEvoy JP, Swartz MS, Davis SM, Rosenheck RA, Perkins DO, Keefe RSE, Davis CE, Severe J, Hsiao JK, CATIE Investigators: Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic. Am J Psychiatry 2006; 163:611–622Google Scholar
14. Egger M, Davey SG, Schneider M, Minder C: Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–634Google Scholar
15. Orwin RG: A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics 1983; 8:157–159Google Scholar
16. Borenstein M, Hedges LV, Higgins JPT, Rothstein H: Comprehensive Meta-Analysis, version 2. Englewood, NJ, Biostat, 2006 (www.meta-analysis.com)Google Scholar
17. Azorin J-M, Spiegel R, Remington G, Vanelle J-M, Péré J-J, Giguere M, Bourdeix I: A double-blind comparative study of clozapine and risperidone in the management of severe chronic schizophrenia. Am J Psychiatry 2001; 158:1305–1313Google Scholar
18. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Schizophrenia, 2nd ed. Am J Psychiatry 2004; 161(Feb suppl)Google Scholar
19. Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Moller HJ: World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: acute treatment of schizophrenia. World J Biol Psychiatry 2005; 6:132–191Google Scholar
20. Leucht S, Arbter D, Engel RR, Kissling W, Davis JM: How effective are second-generation antipsychotic drugs? a meta-analysis of placebo-controlled trials. Mol Psychiatry (Epub ahead of print, Jan 8, 2008)Google Scholar
21. Geddes J, Freemantle N, Harrison P, Bebbington P: Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 2000; 321:1371–1376Google Scholar
22. Heres S, Davis J, Maino K, Jetzinger E, Kissling W, Leucht S: Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine: an exploratory analysis of head-to-head comparison studies of second-generation antipsychotics. Am J Psychiatry 2006; 163:185–194Google Scholar
23. Davis JM, Chen N, Glick ID: Issues that may determine the outcome of antipsychotic trials: industry sponsorship and extrapyramidal side effect. Neuropsychopharmacology 2008; 33:971–975Google Scholar
24. Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IPM, Gheorghe MD, Rybakowski JK, Galderisi S, Libiger J, Hummer M, Dollfus S, Lopez-Ibor JJ, Hranov LG, Gaebel W, Peuskens J, Lindefors N, Riecher-Rossler A, Grobbee DE: Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet 2008; 371:1085–1097Google Scholar
25. Olie JP, Spina E, Murray S, Yang R: Ziprasidone and amisulpride effectively treat negative symptoms of schizophrenia: results of a 12-week, double-blind study. Int Clin Psychopharmacol 2006; 21:143–151Google Scholar
26. Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B: Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry 2001; 158:518–526Google Scholar
27. Lewis SW, Davies L, Jones P, Barnes TRE, Murray RM, Kerwin R, Taylor D, Hayhurst KP, Marwick A, Lloyd H, Dunn G: Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technol Assess 2006; 10:iii–iv, ix–xi, 1–165Google Scholar
28. Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, Bourgeois M, Chouinard G, Islam MZ, Kane J, Krishnan R, Lindenmayer JP, Potkin S: Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003; 60:82–91Google Scholar
29. Kane JM, Honigfeld G, Singer J, Meltzer H, and the Clozaril Collaborative Study Group: Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988; 45:789–796Google Scholar
30. Rosenheck R, Cramer J, Xu WC, Thomas J, Henderson W, Frisman L, Fye C, Charney D: A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. N Engl J Med 1997; 337:809–815Google Scholar
31. Simpson GM, Josiassen RC, Stanilla JK, de Leon J, Nair C, Abraham G, Odom-White A, Turner RM: Double-blind study of clozapine dose response in chronic schizophrenia. Am J Psychiatry 1999; 156:1744–1750Google Scholar
32. Davis JM, Chen N: Dose-response and dose equivalence of antipsychotics. J Clin Psychopharmacol 2004; 24:192–208Google Scholar
33. Meltzer HY, Bastani B, Kwon KY, Ramirez LF, Burnett S, Sharpe J: A prospective study of clozapine in treatment-resistant schizophrenic patients, I: preliminary report. Psychopharmacology (Berl) 1989; 99(suppl):S68–S72Google Scholar
34. Lin CC, Bai YM, Chen JY, Wang YC, Liou YJ, Chao CH, Lai IC, Tsai KY, Chiu HJ: Switching from clozapine to zotepine in schizophrenic patients: a randomised single blind controlled study. Eur Neuropsychopharmacol 2003; 13:318Google Scholar
35. Cohen J: Statistical Power Analysis for the Behavioral Sciences. New York, Academic Press, 1969Google Scholar
36. Kemmler G, Hummer M, Widschwendter C, Fleischhacker W: Dropout rates in placebo-controlled and active-control clinical trials of antipsychotic drugs: a meta-analysis. Arch Gen Psychiatry 2005; 62:1305–1312Google Scholar
37. Lambert BL, Cunningham FE, Miller DR, Dalack GW, Hur K: Diabetes risk associated with use of olanzapine, quetiapine, and risperidone in Veterans Health Administration patients with schizophrenia. Am J Epidemiol 2006; 164:672–681Google Scholar
38. Meyer JM, Davis VG, Goff DC, McEvoy JP, Nasrallah HA, Davis SM, Rosenheck RA, Daumit GL, Hsiao J, Swartz MS, Stroup TS, Lieberman JA: Change in metabolic syndrome parameters with antipsychotic treatment in the CATIE Schizophrenia Trial: Prospective data from phase 1. Schizophr Res 2008; 101:273–286Google Scholar
39. Tarsy D, Baldessarini RJ, Tarazi FI: Effects of newer antipsychotics on extrapyramidal function. CNS Drugs 2002; 16:23–46Google Scholar
40. Kleinberg DL, Davis JM, de Coster R, Van Baelen B, Brecher M: Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol 1999; 19:57–61Google Scholar