Beyond Clinical Utility: Broadening the DSM-V Research Appendix to Include Alternative Diagnostic Constructs
Over the past 15 years, researchers have argued that DSM-IV criteria are hindering investigation into the etiology, pathophysiology, and genetics of mental disorders (1 – 3) and have proposed changes to DSM-V to make it more useful for research. These include moving from a categorical to a dimensional approach more friendly to research (4 – 14) and adopting a “genetic nosology” that seeks to classify patients into categories that correspond to distinct genetic entities (15) . However, because DSM must serve many masters (16) , the prospect of including diagnostic constructs useful for researchers but unfamiliar, burdensome, or of unknown utility to clinicians creates a dilemma: how can DSM-V maintain its role as a common diagnostic language facilitating research efforts without seriously compromising its clinical utility?
One possible solution is to have two versions of DSM-V: one for clinical use and the other for research. This approach was adopted by ICD-10, which provides descriptions and guidelines for clinical use and diagnostic criteria for use by researchers. Although having separate classifications would allow each to be optimized for its intended audience, maintaining divergent classification schemes would stymie communication between clinical and research communities and likely undermine the credibility of the entire diagnostic enterprise.
A better alternative is to broaden the scope of the DSM “criteria sets and axes provided for further study” appendix beyond its current role as a holding tank for proposed categories to include diagnostic constructs intended to facilitate research into the neurobiology and genetics of mental disorders. Potential candidates for this broadened appendix might include dimensional approaches judged too complex or unfamiliar for clinical use, endophenotypes not directly indicative of disorder (17 , 18) , subtypes and specifiers useful primarily in research settings, and risk factors for development of disorders.
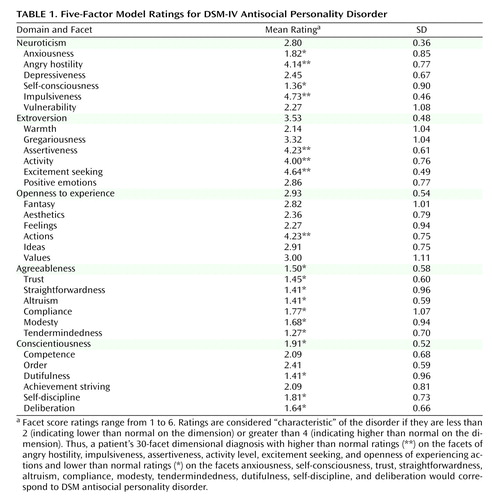
In order to maximize their research utility, these alternative diagnostic entities should be accompanied by explicit guidelines for reliable assessment. This might entail recommending existing assessment instruments or developing new ones. Moreover, these research diagnostic entities should arise out of an empirically based consensus process involving the broadest possible range of researchers to enhance “buy in” of the definitions. Furthermore, a mechanism should be established to allow for updating the appendix definitions in case they are rendered obsolete by new empirical findings. Finally, cross-walks should be developed in order to make it easier for clinicians to apply research findings based on these research diagnostic constructs to clinical practice. Cross-walking from dimensional approaches to DSM categories is conceptually straightforward, since dimensional diagnoses can be converted to categories by establishing threshold cutoff points across the dimensions (19) . For example, Table 1 illustrates the depiction of antisocial personality disorder in terms of the 30 facets (dimensions) of the five-factor model of personality disorder derived from an aggregation of expert ratings (20) .
Including alternative standardized definitions in a DSM-V appendix would provide the research community with diagnostic options still contained within the “official” DSM-V umbrella and thus serve to loosen the “intellectual straitjacket” imposed by the current DSM categorical system ( 21 , p. 3) without creating divergent systems. A welcome side effect is that it may help “de-reify” DSM categories by highlighting their status as provisional man-made constructs open to rethinking in light of evolving knowledge, in turn helping to clarify the intended role of DSM as a useful tool for clinical practice and research rather than as the “bible” of mental disorders (22) .
1. Kendell R, Jablensky A: Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 2003; 160:4–12Google Scholar
2. Hyman S: Foreword, in Advancing DSM: Dilemmas in Psychiatric Diagnosis. Edited by Phillips K, First M, Pincus H. Arlington, VA, American Psychiatric Association, 2003, pp xi–xixGoogle Scholar
3. Charney D, Barlow D, Botteron K, Cohen J, Goldman D, Gur R, et al: Neuroscience research agenda to guide development of a pathophysiologically based classification system, in A Research Agenda for DSM-V. Edited by Kupfer D, First M, Regier D. Arlington, VA, American Psychiatric Association, 2002, pp 31–84Google Scholar
4. Cloninger C: A new conceptual paradigm from genetics and psychobiology for the science of mental health. Aust N Z J Psychiatry 1998; 33:174–186Google Scholar
5. Lenzenweger M: Schizophrenia: refining the phenotype, resolving the endophenotype. Behav Res Ther 1999; 37:281–295Google Scholar
6. Livesley W, Jang K: Toward an empirically-based classification of personality disorder. J Personality Disorder 2000; 14:137–151Google Scholar
7. Meyer R: Finding paradigms for the future of alcoholism research: an interdisciplinary perspective. Alcohol Clin Exp Res 2001; 25:1393–1406Google Scholar
8. Peralta V, Cuesta M, Giraldo C, Cardenas A, Gonzales F: Classifying psychotic disorder: issues regarding categorical vs dimensional approaches and time frame to assess symptoms. Eur Arch Psychiatry Clin Neurosci 2002; 252:12–18Google Scholar
9. Serreti A, Macciardi F, Smeraldi E: Identification of symptomatologic patterns concern in major psychoses: proposal for a phenotype definition. Am J Med Genet 1996; 67:393–400Google Scholar
10. Van Os J, Gilvarry C, Bale E, Van Horn E, Tattan T, White I, et al: A comparison of the utility of dimensional and categorical representations of psychosis. Psychol Med 1999; 29:595–606Google Scholar
11. Clark L: Temperament as a unifying concept in the study of personality and psychopathology. J Abnorm Psychol 2005; 114:505–521Google Scholar
12. Goldberg D: A dimensional model for common mental disorders. Br J Psychiatry 1996; 168(suppl 30):44–49Google Scholar
13. Krueger R, Piasecki T: Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behav Res Ther 2002; 40:485–499Google Scholar
14. Widiger T, Samuel D: Diagnostic categories or dimensions: a question for the Diagnostic and Statistical Manual of Mental Disorders–5th ed. J Abnormal Psychol 2005; 114:494–504Google Scholar
15. Tsuang M, Faraone S, Lyons N: Identification of the phenotype in psychiatric genetics. Eur Arch Psychiatry Clin Neurosci 1993; 243:131–142Google Scholar
16. Maser J, Patterson T: Spectrum and nosology: implications for DSM-V. Psychiatr Clin N Am 2002; 25:855–885Google Scholar
17. Braff D, Geyer M, Swerdlow N: Human studies of prepulse inhibition of startle: normal subjects, patients, groups, and pharmacological studies. Psychopharmacology (Berl) 2001; 156:234–258Google Scholar
18. Calkins M, Iacono W: Eye movement dysfunction in schizophrenia: a heritable characteristic for enhancing phenotype definition. Am J Med Genet 2000; 97:72–76Google Scholar
19. Kraemer H, Noda A, O’Hara R: Categorical versus dimensional approaches to diagnosis: methodological challenges. J Psychiatr Res 2004; 38:17–25Google Scholar
20. Lynam D, Widiger T: Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. J Abnorm Psychol 2001; 110:401–412Google Scholar
21. Van Praag H: Two-tier diagnosing in psychiatry. Psychiatr Res 1990; 34:1–11Google Scholar
22. Kutchins H, Kirk SA: Making Us Crazy—DSM: The Psychiatric Bible and the Creation of Mental Disorders. New York, Free Press, 1997Google Scholar