Symptom Stability in Adult Obsessive-Compulsive Disorder: Data From a Naturalistic Two-Year Follow-Up Study
Abstract
OBJECTIVE: Little is known about the longitudinal course of symptoms in adult patients with obsessive-compulsive disorder (OCD), although some evidence exists regarding symptom stability in children and adolescents. This study systematically investigated the temporal stability of individual symptoms and symptom dimensions of OCD in adult patients who were followed prospectively for 2 years. METHOD: One hundred seventeen adult outpatients with OCD from three U.S. sites were administered the Yale-Brown Obsessive Compulsive Scale symptom checklist four times over a period of 2 years. Eighty-one (69%), 83 (71%), and 67 (57%) patients were available 6 months, 1 year, and 2 years after initial screening, respectively. Different analytic methods assessed the stability of OCD symptoms within and between previously identified symptom dimensions. RESULTS: For the most part, patients maintained their symptoms throughout follow-up, although some symptoms were more stable than others. For the symptoms that changed, changes occurred within rather than between symptom dimensions; qualitative shifts from one dimension to another were rare. The strongest predictor of the presence of a particular symptom was having had that symptom in the past. Although most patients had received pharmacological and behavioral treatment during the follow-up period, changes within symptom dimensions could not be explained by overall clinical improvement over time. CONCLUSIONS: Symptoms of adult patients with OCD might be more stable across time than previously thought, with some symptoms waxing and waning within symptom dimensions and rarely involving shifts between dimensions. Longer follow-up studies involving larger samples are needed to better understand the fluctuations of OCD symptoms across time.
The symptoms of obsessive-compulsive disorder (OCD) are heterogeneous, in that any given patient with this diagnosis may have only one or, more commonly, several symptoms (1). For example, the Yale-Brown Obsessive Compulsive Scale symptom checklist (2, 3) lists more than 50 obsessions and compulsions, divided into 15 categories, any one of which, if of sufficient severity, could qualify a patient for a DSM-IV diagnosis of OCD. There has been much interest in accounting for the symptomatic heterogeneity of OCD in a manner that would ultimately correspond to biological markers, genetic transmission, or treatment response (4–6). Nonetheless, the efforts based on categorical classification of patients with different OCD symptom subtypes (i.e., washers, checkers, etc.) have been relatively fruitless, in part because there are so few monosymptomatic patients; therefore, the recruitment of sufficient numbers of subjects with “pure” OCD subtypes is impractical because such an approach excludes a majority of patients.
Recent factor analytic studies have reduced the symptoms of OCD to a few meaningful dimensions that can better account for the heterogeneous nature of the disorder because it is assumed that any given patient can have symptoms in one or more dimension. These studies have found converging results in spite of using different instruments, such as the Yale-Brown Obsessive Compulsive Scale symptom checklist (4, 6–9) and the Padua Inventory (10). The result of any single factor analytic study can be somewhat arbitrary because this statistical technique is sensitive to the scaling of variables and depends on the decision rules used for retaining factors and, therefore, might not fully capture the complex structure of OCD (unpublished data of D.M. Shera and J.G. Ibrahim).
Nonetheless, factor analytic studies have found remarkably similar symptom structures, ranging from three to five reliable dimensions (4, 6–10): 1) symmetry obsessions and repeating, counting, and ordering compulsions, 2) hoarding obsessions and compulsions, 3) contamination obsessions and cleaning compulsions, 4) aggressive obsessions and checking compulsions, and 5) sexual/religious obsessions and related compulsions.
Several studies have suggested that the dimensional approach might help guide research on the neurobiology and treatment of OCD. Indeed, the identified symptom dimensions have been found to be specifically related to sociodemographic variables, such as sex and age at onset (4, 6, 8), genetic factors (11), comorbid chronic tics and personality disorders (4, 6, 8, 12), and regional cerebral blood flow (5). Treatment response studies have shown that patients with hoarding and sexual/religious symptoms might be less likely to respond to serotonin reuptake inhibitors (SRIs) and behavior therapy (6, 13, 14). One hope is that this approach will help in developing more specialized treatments for each type of symptom or patient.
One potential challenge to the dimensional approach is the observation that OCD symptoms in a given individual can change over time. In the longest prospective study on the course of OCD published to date, which covered the natural history of the disorder over a period of 40 years (15), qualitative changes of OCD symptoms occurred in 58% of the patients (although few patients with an early monosymptomatic picture became polysymptomatic at follow-up). However, some of the definitions of symptoms in this study were idiosyncratic and, therefore, not directly comparable to the current Yale-Brown Obsessive Compulsive Scale symptom checklist categories (16). More information on the longitudinal course of OCD symptoms is available for child and adolescent populations (17–19).
To our knowledge, the only available study that specifically addressed OCD symptom stability using modern symptom descriptions is that of Rettew and co-workers (19), who followed 79 children and adolescents with OCD over a period of 2–7 years. They found that none of the subjects maintained the same constellation of symptoms from initial assessment to follow-up. However, Rettew et al. analyzed only individual symptoms, and they acknowledged that “many patients dramatically changed their ritualistic behavior without changing [symptom] categories” (p. 1054). Indeed, Rettew et al. suggested that a different way of grouping the symptoms of the Yale-Brown Obsessive Compulsive Scale symptom checklist might have revealed other developmental trends. It is plausible, then, that changes might occur within rather than between each of the OCD symptom dimensions identified by factor analytic methods.
Thus, although some symptom change over time has been documented in pediatric OCD, to our knowledge analogous data have yet to be published for adults with OCD. We analyzed data from a naturalistic 2-year follow-up study conducted in three OCD clinics, which involved repeated administrations of the Yale-Brown Obsessive Compulsive Scale symptom checklist over time. Data on the course and severity of obsessive-compulsive symptoms as well as patterns of remission and relapse for two of the sites (Brown University and Yale University) have been reported elsewhere (20). In the current report, our primary research questions were 1) Are individual symptoms of adult OCD stable across time? 2) Are previously identified symptom dimensions of OCD stable? 3) Are some symptoms more stable than others? 4) Can changes be attributed to the effects of treatment? 5) Do changes occur within symptom dimensions, or, are there shifts from one dimension to another?
Method
Patients
A consecutive sample of 117 patients with a primary diagnosis of OCD, being seen at three specialized university-based (Brown, Yale, and Harvard [Massachusetts General Hospital]) OCD clinics for evaluation or ongoing treatment, participated in the study after providing written informed consent. Sixty-four (55%) of the participants were men, and 53 (45%) were women. Their mean age was 34.9 years (SD=12.5). Their mean score on the total Yale-Brown Obsessive Compulsive Scale was 20.2 (SD=8.9), their mean score on the obsessions subscale was 10.05 (SD=4.6), and their mean score on the compulsions subscale was 10.1 (SD=5.2). Data comparability analyses showed no differences among the three sites in sex distribution, age, or Yale-Brown Obsessive Compulsive Scale scores.
Inclusion criteria were age of 18 years or older and a willingness to be followed for 2 years. The diagnosis of OCD was confirmed in all cases by experienced interviewers through use of a structured diagnostic interview (21). Patients with comorbid diagnoses were not excluded from the study, provided that OCD was the dominant disorder for which treatment was sought.
Of the initial group of patients, 81 (69%) attended their respective clinics at 6-month follow-up, 83 (71%) at 1-year follow-up, and 67 (57%) at 2-year follow-up. There were no statistically significant differences in baseline characteristics between subjects who did or did not participate in the follow-up evaluations. For the Brown and Yale sites, 45 (68%) of 66 patients who participated in the 2-year follow-up had received medium-to-high doses of SRIs for 12 weeks or more, and 12 (18%) had received an adequate trial of behavior therapy over the 2-year period (20). Treatment data were not available for the Massachusetts General Hospital site.
Clinical Measures
Instruments included the 10-item clinician-rated Yale-Brown Obsessive Compulsive Scale (2, 3) and the Yale-Brown Obsessive Compulsive Scale symptom checklist, a list of more than 50 common obsessions and compulsions organized under 13 major symptom categories plus two categories of miscellaneous obsessions and compulsions. The Yale-Brown Obsessive Compulsive Scale symptom checklist also includes a target symptom list of the four most prominent symptoms for each patient. These baseline measures were repeated at each follow-up.
Symptom Dimensions
Following the methods of previous studies (4, 6, 12), for each of the 13 major categories of the Yale-Brown Obsessive Compulsive Scale symptom checklist, if a patient identified at least one of the specific symptoms in a category as a principal or major problem, that category was assigned a score of 2. If a patient endorsed at least one of the specific symptoms but did not consider it a major problem, that category was assigned a score of 1. A score of 0 was assigned if a patient did not endorse any of the symptoms under that category. Thus, a score of 0, 1, or 2 was assigned to each of 13 categories—seven major obsessive symptom categories and six major compulsive categories of the Yale-Brown Obsessive Compulsive Scale symptom checklist. In the current study, the patients’ scores on the five symptom dimensions identified in a previous study (6) were computed by summing the scores of the symptom categories under each dimension; these scores were then used in all subsequent data analyses. The five symptom dimensions were symmetry/ordering, hoarding, contamination/cleaning, aggressive/checking, and sexual/religious obsessions.
Statistical Analyses
For each individual Yale-Brown Obsessive Compulsive Scale symptom category, McNemar’s tests were used to determine the chance that symptoms changed or remained unchanged across follow-up. To analyze changes in symptom severity (10-item Yale-Brown Obsessive Compulsive Scale) and within the five previously identified OCD symptom dimensions, we compared current symptoms at baseline and at 6-month, 1-year, and 2-year follow-ups and then applied repeated measures analyses of variance (ANOVAs). Degrees of freedom were adjusted by using the Greenhouse-Geisser epsilon when the results of the Mauchly Sphericity Test were significant. Because changes within symptom dimensions could be confounded with overall reduction in OCD severity attributable to treatment, the percent decrease from baseline to 2-year follow-up on the total Yale-Brown Obsessive Compulsive Scale score was included as a covariate in the analyses.
To assess the degree of change between previously identified OCD symptom dimensions, we tested a series of stepwise multiple regression models in which each symptom dimension at a given follow-up point was the dependent variable and all five OCD symptom dimensions at the immediately preceding follow-up point were entered as independent variables. Significance level was set at p<0.01 to control for possible type I errors due to multiple testing. The SPSS statistical package, version 9.0 (SPSS, Inc., Chicago) was used in all analyses.
Results
Changes Within Individual Categories of Obsessions and Compulsions
The frequencies of the 13 major symptom categories of the Yale-Brown Obsessive Compulsive Scale symptom checklist across time are shown in Table 1. Most patients retained their symptoms across follow-up. McNemar’s tests showed that the symptoms of some patients changed significantly from baseline to 6-month follow-up, that is, symptoms that had been present at baseline were no longer present at the second screening. Changes were more likely to occur in aggressive obsessions, as well as in cleaning, checking, counting, ordering, and hoarding compulsions. When we used a less stringent 0.05 significance level, we observed changes in contamination, hoarding, and symmetry obsessions as well. Changes in individual symptoms from 6 to 12 months and from 1-year to 2-year follow-up were much less likely.
Changes Within Symptom Dimensions
Repeated measures ANOVAs showed significant differences over time on the aggressive/checking (F=9.94, df=3, 150, p<0.001), symmetry/ordering (F=6.43, df=3, 150, p=0.001), and contamination/cleaning (F=4.16, df=3, 150, p=0.007) dimensions. The hoarding and sexual/religious dimensions remained mostly unchanged across time (Figure 1).
Effects of Treatment During Follow-Up
As mentioned earlier, most patients had received an adequate trial of an SRI and/or behavior therapy over the 2-year period. Repeated measures ANOVAs found significant improvements on the Yale-Brown Obsessive Compulsive Scale total score from pretreatment (mean=20.7, SD=9.6) to 2-year follow-up (mean=15.8, SD=8.9) (F=10.66, epsilon-corrected df=1.9, 85.1, p<0.001). More details on the 2-year clinical picture can be found elsewhere (20). Repeated measures analyses with the percent drop on the total Yale-Brown Obsessive Compulsive Scale over the 2-year period as a covariate yielded nonsignificant covariance coefficients, suggesting that changes within symptom dimensions of OCD were independent from the overall reduction in symptom severity.
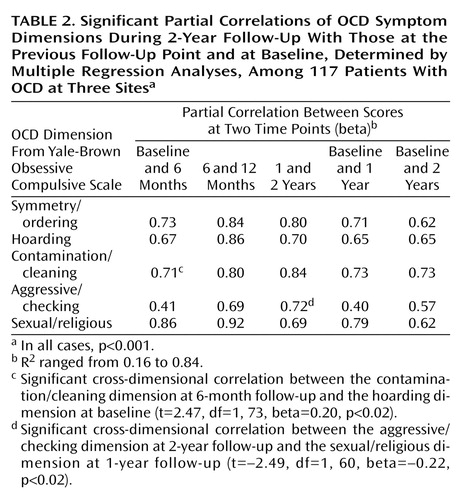
Changes (Shifts) Between Symptom Dimensions
Multiple regression analyses showed strong partial correlations between each OCD symptom dimension at a given follow-up point and the same dimension at the immediately previous point, whereas significant correlations between different dimensions were rare and small (Table 2). Similarly, there were strong partial correlations between each OCD symptom dimension at different follow-up points with respect to baseline scores on the same dimension. Overall, most partial correlations were greater than 0.60; the only exception was the aggressive/checking dimension, which had the smallest partial correlations across time.
Discussion
To our knowledge, this is the first study that prospectively evaluated the symptom stability of OCD symptoms in a group of well-characterized adult patients with OCD. Most patients retained their symptoms across follow-up, but, for some of them, symptoms that had been present at baseline were no longer present at 6-month follow-up. Analyses of individual obsessions and compulsions showed changes on most symptom categories from baseline to 6-month follow-up, but these were less likely to occur after 6 months. The symptoms that were most likely to change from baseline to 6-month follow-up were aggressive and contamination obsessions and checking, cleaning, hoarding, counting, and ordering compulsions. Similar changes were observed within previously identified OCD symptom dimensions (aggressive/checking, symmetry/ordering, and contamination/cleaning), which include most of the individual symptoms found most likely to change.
The remaining symptom dimensions (i.e., sexual/religious and hoarding) and some individual symptoms (i.e., somatic obsessions) tended to remain unchanged across follow-up. Similarly, Skoog and Skoog (15) reported that very few of their patients with an early monosymptomatic picture (mostly with somatic obsessions and compulsions) experienced changes across follow-up. Taken together, these results seem to suggest that some OCD symptoms are more stable across time than others. One possible explanation is that patients with certain symptoms might be more treatment resistant (6, 13, 14), and, therefore, those symptoms might be less likely to change over time. However, this was not supported by the data: the reported changes within symptom dimensions were unaffected by overall reductions on the Yale-Brown Obsessive Compulsive Scale severity scale. Future studies should investigate why some symptoms are more likely to fluctuate over time than others and whether different interventions (e.g., SRIs, monoamine oxidase inhibitors, cognitive behavior therapy, psychosurgery) are especially indicated to treat particular symptoms (6).
When analyses were performed to examine whether there were qualitative changes from one symptom dimension to another across follow-up, results showed that those were rare. Indeed, changes seemed to occur within rather than between OCD symptom dimensions. In fact, the strongest predictor of having a given symptom was having had that same symptom in the past, suggesting that adult patients with OCD present a fairly stable symptom constellation across time. These results are in contrast to the pediatric OCD literature, which has reported dramatic changes across time in children and adolescents with OCD (18, 19).
There are important methodological differences between our study and the National Institute of Mental Health studies of children and adolescents with OCD (19). In the latter, only individual symptoms were analyzed rather than symptom dimensions. In fact, Rettew et al. (19) suggested the possibility that the observed changes had actually occurred within rather than between symptom categories, although their design did not allow them to test this hypothesis. Alternatively, despite the striking similarity between the clinical presentation of OCD in children and in adults (17, 18), it is possible that pediatric OCD patients experience changes in their symptoms across ontogeny but that their symptoms stabilize once they reach adulthood. Whether OCD symptoms follow a specific maturational course in pediatric patients and then stabilize in adults is a hypothesis that deserves further examination.
We have proposed a modular model of OCD, which suggests a correspondence between the different symptom dimensions and dysfunction at different nodes within the neurocircuitry implicated in the disorder (5, 6). One hope is that such a correspondence might extend to the genetic underpinnings of OCD as well (11). The notion that symptom dimension and brain imaging profiles could serve as useful phenotypes for unraveling the underlying genetics would rely on a relative temporal stability of these clinical features. The results of this study suggest that, in adult patients with OCD, symptoms remain remarkably stable over time, providing some reassurance that such a strategy would be feasible.
The main limitation of the present study is that a 2-year follow-up period might be too short to evaluate the temporal course of OCD symptoms. Therefore, the results should be taken as preliminary. However, these results have important implications that could help guide future research. One practical implication is that future studies using this method might benefit from using both current and past symptoms of the Yale-Brown Obsessive Compulsive Scale symptom checklist in their analyses, because a one-time measure of OCD symptoms could easily neglect symptoms that are temporarily dormant. More importantly, this and other treatment response studies strongly suggest that more specialized treatment interventions need to be developed for patients with different symptoms, because the standard therapeutic approaches still leave many patients unimproved.
In summary, a consensus exists regarding the chronic nature and waxing and waning course of both adult and pediatric OCD (DSM-IV, 14, 15, 17, 18, 20, 22). However, the present study indicates that some symptoms (i.e., hoarding, sexual/religious, and somatic obsessions) could be more stable across time than others. For symptoms that are most likely to fluctuate across time (i.e., the contamination/cleaning, aggressive/checking, and symmetry/ordering categories), changes seem to occur within rather than between symptom categories. These results imply that patients might experience changes in the content of their concerns within symptom dimensions (e.g., a patient with contamination symptoms who is first concerned about cancer and then AIDS later in the course of follow-up). However, patients are not likely to experience qualitative changes in their type of concern, that is, between symptom dimensions. Therefore, adult patients with OCD might present a more stable symptom constellation than previously thought. Longer longitudinal studies involving larger patient samples of children and adults with OCD are needed to further understand the longer-term course of OCD symptoms and the relationship between childhood and adulthood forms of the disorder.
 |
 |
Received Sept. 28, 2000; revision received May 30, 2001; accepted Sept. 14, 2001. From the Department of Psychiatry, Imperial College School of Medicine, London; the Department of Psychiatry, Massachusetts General Hospital, Harvard Medical School, Boston; the Department of Psychiatry and Human Behavior, Brown University School of Medicine, Butler Hospital, Providence, R.I.; and the Department of Psychiatry, Yale University School of Medicine, New Haven, Conn. Address reprint requests to Dr. Mataix-Cols, Department of Psychiatry, Division of Neuroscience and Psychological Medicine, Imperial College School of Medicine, Stress Self-Help Clinic, 303 North End Rd., London, W14 9NS, U.K.; [email protected] (e-mail). Funded in part by the Spanish Ministerio de Educación y Cultura and an EU Marie Curie Fellowship (Dr. Mataix-Cols). The authors thank Prof. Isaac Marks and Dr. Homa Noshirvani for their useful comments.
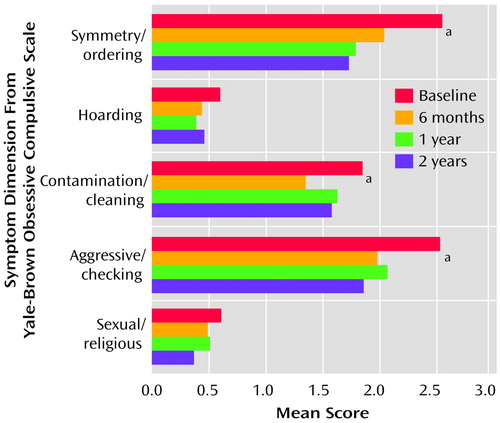
Figure 1. Symptom Dimensions of OCD Over 2 Years Among 117 Patients With OCD at Three Sitesa
aSignificant changes over time on repeated measures analyses of variance for the dimensions of symmetry/ordering (F=6.43, df=3, 150, p=0.001), contamination/cleaning (F=4.16, df=3, 150, p=0.007), and aggressive/checking (F=9.94, df=3, 150, p<0.001).
1. Rasmussen SA, Eisen JL: Clinical and epidemiological findings of significance to neuropharmacologic trials in obsessive-compulsive disorder. Psychopharmacol Bull 1988; 24:466-470Medline, Google Scholar
2. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006-1011Crossref, Medline, Google Scholar
3. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, II: validity. Arch Gen Psychiatry 1989; 46:1012-1016Crossref, Medline, Google Scholar
4. Baer L: Factor analysis of symptom subtypes of obsessive compulsive disorder and their relation to personality and tic disorders. J Clin Psychiatry 1994; 55:18-23Google Scholar
5. Rauch SL, Dougherty DD, Shin LM, Alpert NM, Manzo P, Leahy L, Fischman AJ, Jenike MA, Baer L: Neural correlates of factor-analyzed OCD symptom dimensions: a PET study. CNS Spectrums 1998; 3:37-43Crossref, Google Scholar
6. Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L: Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry 1999; 156:1409-1416Abstract, Google Scholar
7. Hantouche EG, Lancrenon S: Modern typology of symptoms and obsessive-compulsive syndromes: results of a large French study of 615 patients. Encephale 1996; 22:9-21Medline, Google Scholar
8. Leckman JF, Grice DE, Boardman J, Zhang H, Vitale A, Bondi C, Alsobrook J, Peterson BS, Cohen DJ, Rasmussen SA, Goodman WK, McDougle CJ, Pauls DL: Symptoms of obsessive-compulsive disorder. Am J Psychiatry 1997; 154:911-917Link, Google Scholar
9. Summerfeldt LJ, Richter MA, Antony MM, Swinson RP: Symptom structure in obsessive-compulsive disorder: a confirmatory factor-analytic study. Behav Res Ther 1999; 37:297-311Crossref, Medline, Google Scholar
10. van Oppen P, Hoekstra RJ, Emmelkamp PM: The structure of obsessive-compulsive symptoms. Behav Res Ther 1995; 33:15-23Crossref, Medline, Google Scholar
11. Alsobrook JP, Leckman JF, Goodman WK, Rasmussen SA, Pauls DL: Segregation analysis of obsessive-compulsive disorder using symptom-based factor scores. Am J Med Genet Neuropsychiatr Genet 1999; 88:669-675Crossref, Medline, Google Scholar
12. Mataix-Cols D, Baer L, Rauch SL, Jenike MA: Relation of factor-analyzed symptom dimensions of obsessive-compulsive disorder to personality disorders. Acta Psychiatr Scand 2000; 102:199-202Crossref, Medline, Google Scholar
13. Black DW, Monahan P, Gable J, Blum N, Clancy G, Baker P: Hoarding and treatment response in 38 nondepressed subjects with obsessive-compulsive disorder. J Clin Psychiatry 1998; 59:420-425Crossref, Medline, Google Scholar
14. Alonso MP, Menchón JM, Pifarré J, Mataix-Cols D, Torres L, Salgado P, Vallejo J: Long-term follow-up and predictors of clinical outcome in obsessive-compulsive patients treated with serotonin reuptake inhibitors and behavioral therapy. J Clin Psychiatry 2001; 62:535-540Crossref, Medline, Google Scholar
15. Skoog G, Skoog I: A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry 1999; 56:121-127Crossref, Medline, Google Scholar
16. Price LH, Rasmussen SA, Eisen JL: The natural history of obsessive-compulsive disorder. Arch Gen Psychiatry 1999; 56:131-132Crossref, Medline, Google Scholar
17. Flament MF, Koby E, Rapoport JL, Berg CJ, Zahn T, Cox C, Denckla M, Lenane M: Childhood obsessive-compulsive disorder: a prospective follow-up study. J Child Psychol Psychiatry 1990; 31:363-380Crossref, Medline, Google Scholar
18. Swedo SE, Rapoport JL, Leonard H, Lenane M, Cheslow D: Obsessive-compulsive disorder in children and adolescents: clinical phenomenology of 70 consecutive cases. Arch Gen Psychiatry 1989; 46:335-341Crossref, Medline, Google Scholar
19. Rettew DC, Swedo SE, Leonard HL, Lenane MC, Rapoport JL: Obsessions and compulsions across time in 79 children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 1992; 31:1050-1056Crossref, Medline, Google Scholar
20. Eisen JL, Goodman WK, Keller MB, Warshaw MG, DeMarco LM, Luce DD, Rasmussen SA: Patterns of remission and relapse in obsessive-compulsive disorder: a 2-year prospective study. J Clin Psychiatry 1999; 60:346-351Crossref, Medline, Google Scholar
21. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1989Google Scholar
22. Steketee G, Eisen JL, Dyck I, Warshaw M, Rasmussen SA: Predictors of course in obsessive-compulsive disorder. Psychiatry Res 1999; 89:229-238Crossref, Medline, Google Scholar



