A Review and Meta-Analysis of the Genetic Epidemiology of Anxiety Disorders
Abstract
OBJECTIVE: The authors conducted meta-analyses of data from family and twin studies of panic disorder, generalized anxiety disorder, phobias, and obsessive-compulsive disorder (OCD) to explore the roles of genetic and environmental factors in their etiology. METHOD: MEDLINE searches were performed to identify potential primary studies of these disorders. Data from studies that met inclusion criteria were incorporated into meta-analyses that estimated summary statistics of aggregate familial risk and heritability for each disorder. RESULTS: For family studies, odds ratios predicting association of illness in first-degree relatives with affection status of the proband (disorder present or absent) were homogeneous across studies for all disorders. The calculated summary odds ratios ranged from 4 to 6, depending on the disorder. Only for panic disorder and generalized anxiety disorder could the authors identify more than one large-scale twin study for meta-analysis. These yielded heritabilities of 0.43 for panic disorder and 0.32 for generalized anxiety disorder. For panic disorder, the remaining variance in liability could be attributed primarily to nonshared environment. For generalized anxiety disorder, this was true for men, but for women, a potentially significant role for common familial environment was also seen. CONCLUSIONS: Panic disorder, generalized anxiety disorder, phobias, and OCD all have significant familial aggregation. For panic disorder, generalized anxiety disorder, and probably phobias, genes largely explain this familial aggregation; the role of family environment in generalized anxiety disorder is uncertain. The role of nonshared environmental experience is significant, underscoring the importance of identifying putative environmental risk factors that predispose individuals to anxiety.
Anxiety disorders are common; lifetime prevalence for the group of disorders is estimated to be as high as 25% (1). They are highly comorbid with each other and with other psychiatric conditions (2), particularly mood disorders (3). Anxiety disorders carry a substantial burden of distress and impairment that is comparable to that of chronic “medical” disorders, such as diabetes (4–8). As such, their etiology has been, and continues to be, a major target of investigation.
A long history of primary studies has sought to determine whether anxiety disorders are familial and to estimate their heritability. A number of excellent, detailed reviews of the genetic epidemiology of anxiety disorders have also appeared (e.g., reference 9). Much knowledge has been amassed in this area; however, to date, there has been no attempt to summarize the information quantitatively. Therefore, a meta-analytic treatment of the data is timely, particularly as many research groups have begun to search for “anxiety genes.”
We have attempted to answer, by means of a meta-analysis of selected epidemiological studies, the following two questions for major anxiety disorders: 1) what is the magnitude of the familial aggregation of anxiety disorders? 2) what is the relative contribution of genetics and environment to their etiology?
We applied this method to the following anxiety disorders: panic disorder, generalized anxiety disorder, phobias, and obsessive-compulsive disorder (OCD). We were limited to family and twin studies, as we know of no available adoption studies of anxiety disorders.
Method
The basic goals of meta-analysis, as applied in this study to the genetic epidemiology of anxiety disorders, are 1) to determine the consistency between differing results by testing for heterogeneity across studies and 2) to combine data from multiple primary studies for the purpose of synthesizing the information, thus providing more reliable, precise, and less biased aggregate estimates of familial risk and heritability.
We performed a keyword-driven MEDLINE search to identify all potential primary studies for inclusion in our analyses. In addition, we searched the reference sections of these manuscripts and existing reviews for additional sources. We limited our analyses to studies involving adult subjects that estimated the risk in relatives for the same anxiety disorder as that diagnosed in the proband. Although some of the studies included in this analysis examined the question of familial and genetic sources of the comorbidity of anxiety disorders, this important issue is outside of the scope of this study.
We used the following inclusion criteria for the studies: 1) use of operationalized diagnostic criteria, to the exclusion of studies assessing only anxiety symptoms and older studies of anxiety neuroses; 2) systematic ascertainment of probands and relatives; 3) direct interviews with the majority of subjects, to the exclusion of family history studies; 4) diagnostic assessment of relatives performed with investigators blind to proband affection status; and 5) for family studies, inclusion of a comparison group. For some disorders, in which fewer studies were available, we relaxed the criterion for blind ascertainment of diagnosis only to increase our data pool for comparison. Many primary studies identified in the literature were rejected for failing one or more of these criteria. In particular, twin studies meeting the inclusion criteria were limited to, at most, one or two large independent samples per disorder.
Family studies may be thought of as a type of case-control study design, in which the patients are affected probands and the comparison subjects are individuals without a history of the disorder (10). The measure of interest is the binary outcome of a relative diagnosed as affected or unaffected, which allows construction of 2×2 contingency tables of affected versus unaffected relatives of patients and comparison subjects. We reported the odds ratio as the measure of association, owing to its desirable statistical property of invariance under study design (10) and greater familiarity to readers than, e.g., the tetrachoric correlation, which is less sensitive to prevalence (11). In addition, stratifying by study allows one to test for homogeneity across studies by means of the Breslow-Day statistic (12) and to calculate a summary odds ratio by means of the Mantel-Haenszel method (13). The SAS routine proc freq (14) was used to make these calculations. For panic disorder and OCD, for which the most data exist, we also calculated an aggregate risk by combining raw data from each of the studies.
For the twin studies, we were limited by the scarcity of studies that met our inclusion criteria; only two large twin samples that met our criteria and were used to study anxiety disorders exist: the Virginia Twin Registry (15) and the Vietnam Era Twin Registry (16). Data from the Virginia Twin Registry have been reported regarding panic disorder, generalized anxiety disorder, and phobias; data from the Vietnam Era Twin Registry have been published on panic disorder and generalized anxiety disorder. Therefore, we attempted meta-analysis using twin data for panic disorder and generalized anxiety disorder only, but we tabulated twin data for the other disorders where it was available.
We report several measures of twin resemblance, depending on availability. The proband-wise concordance is the proportion of affected co-twins of affected index twins. The tetrachoric correlation is between the members of a twin pair regarding their liability for the disorder; it assumes an underlying continuous trait with a threshold that distinguishes between unaffected and affected twins. Structural equation modeling provides estimates of variance in liability to a disorder that are attributable to additive genetic (a2), common familial environmental (c2), and individual-specific environmental (e2) factors (17).
For panic disorder and generalized anxiety disorder, we performed structural equation modeling by combining data from the two large twin studies using the statistical package Mx (18). To this end, we created 2×2 contingency tables of affection status for twin 1 versus twin 2 from the reported sample parameters for each study. The output of the modeling provided the fit of the model and the component estimates of variance. The fit of submodels created by placing limiting assumptions on the model (such as testing the significance of one of the variance components) was then compared to that of the full (saturated) model. Data from the Vietnam Era Twin Registry come from same-sex male twin pairs, whereas data from the Virginia Twin Registry come from same-sex female twins for panic disorder and male-male, female-female, and opposite-sex twin pairs in the most recent assessment of generalized anxiety disorder. Therefore, the most saturated models allowed for differing proportions of genetic and environmental variance between men and women, whereas the submodels tested the hypothesis that these were the same for the two genders. In setting up the model, significant differences in prevalence in the various groups required that different thresholds be assigned.
Finally, for panic disorder and generalized anxiety disorder, we attempted to perform an overall structural equation modeling of the combined twin and family data. In comparison to the population-based twin data, data from all of the family studies were from clinically ascertained probands. Therefore, some restrictive assumptions had to be made in order to combine them. Owing to differing prevalence estimates among the family studies that were obtained by use of unequal comparison groups, a threshold for each family study was not calculated from the sample characteristics as it was for the twin data, but, rather, it was assigned from a base prevalence rate obtained from National Comorbidity Survey data (1). In addition, because the family study data were not reported separately by gender or type of relative, we had to make the rather broad assumption that all of the first-degree relatives in these studies could be modeled as if they had the same genetic and environmental correlations as did their siblings (or dizygotic twins). We tested the validity of this assumption by including a special twin environmental parameter that differentiated between dizygotic resemblance in twin pairs and all first-degree relatives in the family studies. We also had to test the hypothesis that model parameters from clinical and community samples could be equated to obtain aggregate estimates. Since all of the family studies used clinical study groups and the larger twin studies were community-based, it was not possible to test these last two assumptions separately. For several studies, partially or wholly overlapping samples were studied in more than one report. In most cases, we chose the studies that contained the largest sample sizes or the most recent results.
Results
Panic Disorder
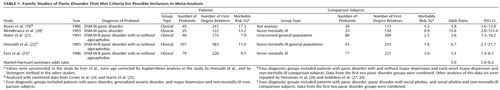
Five family studies of panic disorder, all from clinical populations, met our criteria for inclusion (Table 1). Studies excluded from our analysis are cited in the References (29–32). (For detailed reviews, refer to references 33–36). All five studies support the familial aggregation of panic disorder. Except for the study by Mendlewicz et al. (20), all of the odds ratios are similar; in no instance do they significantly differ from each other. The results of our meta-analysis show that there is a significant association between panic disorder in the probands and panic disorder in the first-degree relatives (Mantel-Haenszel statistic=47.8, df=1, p<0.0001); the hypothesis that the odds ratios for the five studies were homogeneous could not be rejected (Breslow-Day χ2=2.69, df=4, p=0.61). The summary odds ratio across the five studies was 5.0 (95% confidence interval [CI]=3.0–8.2), which strongly supports a familial component in liability to panic disorder. The unadjusted aggregate risk based on 1,356 total first-degree relatives of panic disorder probands was 10.0%, compared to 2.1% in 1,187 comparison relatives.
Three twin studies of panic disorder met our inclusion criteria (Table 2). We also tabulated two other (nonblind) studies but did not include them in the meta-analysis. The first three smaller studies support a role for genetic factors in the etiology of panic disorder. The two larger twin studies, performed on different samples and opposite genders, are consistent with each other in attributing 30%–40% of the variance in liability to additive genetics; the remaining variance in liability comes from individual-specific environments. The twin studies do not support a role for common family environment in the etiology of panic disorder. Combining the three blinded studies by means of structural equation modeling in Mx produced a best-fitting model that included only additive genetics and individual environmental factors, which is consistent with the results of the primary studies. In addition, we could constrain the genetic variance to be equal across the studies without a significant deterioration in model fit (Δχ2=3.43, df=2, p>0.10), which suggests that genes affect panic disorder similarly in men and women. The parameters of the best-fitting model are provided at the bottom of Table 2.
We then tested the broader model, combining the family study data with the twin data. We found that the special twin environmental parameter that differentiated between dizygotic twins and other first-degree relatives could be made equal to zero with no degradation in fit (Δχ2=0.003, df=1, p=0.95), which allowed us to equate parameters across studies. This combined data produced a best-fitting model that required only additive genetics and individual environment to account for liability to panic disorder, with a heritability estimate of 0.48 (95% CI=0.41–0.54).
Generalized Anxiety Disorder
Only one family study of generalized anxiety disorder met all of our inclusion criteria (20). In order to expand our sample, we included one additional study, that of Noyes et al. (40), which met all criteria except blind assessment. As indicated in Table 3, both studies supported the familial aggregation of generalized anxiety disorder, with an odds ratio greater than 1, and together they showed a significant association between generalized anxiety disorder in the probands and in their first-degree relatives (Mantel-Haenszel statistic=19.1, df=1, p<0.0001). A Breslow-Day test supported homogeneity of the odds ratio (Breslow-Day χ2=0.69, df=4, p=0.61), and we calculated the Mantel-Haenszel summary odds ratio as 6.1 (95% CI=2.5–14.9), which supports familial aggregation of generalized anxiety disorder.
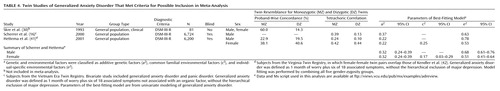
Two large twin studies met our inclusion criteria (16, 41), and we included one smaller controlled nonblinded study (30) in Table 4. The twin studies excluded are listed in the References (43, 44). The excluded study by Roy et al. (44) reported a bivariate analysis of major depression and generalized anxiety disorder in a sample of 1,484 male and female twins originally ascertained for affective illness from a combination of clinical and population sources. Although it met our inclusion criteria, because this study employed a complex ascertainment scheme, we chose not to use this data in our meta-analysis. Similar to what was done with the twin studies regarding panic disorder, we combined the two larger studies of generalized anxiety disorder by means of structural equation modeling. For consistency with the Scherrer et al. study (16), we used the definition of generalized anxiety disorder of 1 months’ minimum duration from a report by Hettema et al. (41) without diagnostic hierarchy. The best-fitting model predicted that 31.6% (95% CI=24%–39%) of the variance for liability to generalized anxiety disorder was attributable to additive genetics in both genders and that the same genes predispose men and women to generalized anxiety disorder. The model also estimated a small role for common familial environment in the women only, with the remaining variance due to individual-specific environment. Although not included in the meta-analysis, the study by Roy et al. (44) estimated an additive genetic variance of 14.3% and 49% for their narrow and broad definitions of generalized anxiety disorder, respectively, no role for common environmental factors, and no gender differences. Since we could not equate the model parameters across genders as was possible for panic disorder, we were unable to combine the twin and family data into one model.
Although only a few family and twin studies of generalized anxiety disorder exist that were appropriate for our analyses, they provided convincing evidence for familial aggregation. In addition, the twin studies suggested at least a modest role of genetics in familial aggregation and an uncertain role of common environment. (For a review of genetic studies of generalized anxiety disorder, see Woodman [35].)
Phobias
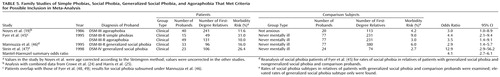
For the purposes of this meta-analysis, specific phobias, social phobia, generalized social phobia, and agoraphobia were grouped together owing to the scarcity of these studies in each of the individual categories. Four family studies of phobias met our criteria for inclusion in this analysis; they are listed in Table 5. All studies support the familial aggregation of phobias. Except for the Stein et al. study (47), all of the odds ratios are similar, and they are statistically consistent with each other. The results of our meta-analysis show that there is a significant association between phobias in probands and in their first-degree relatives (Mantel-Haenszel statistic=52.3, df=1, p<0.0001), and the hypothesis that the odds ratios for the five studies were homogeneous could not be rejected (Breslow-Day χ2=4.03, df=4, p=0.40). The summary odds ratio across the studies was 4.1 (95% CI=2.7–6.1), which strongly supports a familial risk for phobic disorders. (The family studies reviewed that did not meet the inclusion criteria are references 32, 50, and 51.)
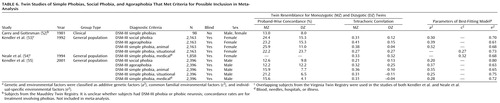
The only twin studies of phobias that met our inclusion criteria were reported by our group for the Virginia Twin Registry sample, which was described earlier. Included in Table 6 are the results from a report by Carey and Gottesman (52) of a nonblinded assessment of 49 twin pairs from the Maudsley Twin Registry made up of twins hospitalized for obsessional neurosis, obsessional personality disorder, or phobic neurosis. It is not clear whether DSM-III criteria for phobias or OCD were used in the study, and the authors provided concordance rates for various levels of treatment criteria. We chose to include their data for twins who had a treatment episode involving phobias (Table 6), as this appeared to be the definition most consistent with a DSM phobic disorder. (The twin studies we excluded are references 43, 56–60.)
The following discussion focuses on data from the Virginia Twin Registry. Kendler et al. (53) reported best-fitting models for social phobia, agoraphobia, and animal phobias that suggested additive genetics is responsible for twin resemblance in women and that there is no role for common environment. In situational phobias and phobias involving blood, needles, hospitals, or illness, reported in Neale et al. (54), the best-fitting models suggested just the opposite. This may not represent a real difference, however, since there may not have been sufficient power to differentiate between these two sources of variance (61). In fact, in a subsequent analysis that included measurement reliability from two assessments 8 years apart, the models predicted that twin resemblance was due solely to additive genetics for all but animal phobias and that when fears and phobias were combined by using a multiple threshold model, additive genetics alone accounted for twin resemblance in all of the phobic categories (62). We recently obtained similar results in a twin sample of men; the results are displayed in the bottom of Table 6(55).
Although we know of only one large adult twin sample in which phobia diagnoses were examined, it predicted that additive genetics is largely responsible for the familial aggregation seen in the family studies, which represents roughly 20%–40% of the variance seen, depending on the type of phobia. Its results are supported by a large population-based adolescent twin study of social phobia, major depression, and alcoholism (63), in which additive genetics accounted for 28% of the variance in risk for social phobia, with the remainder due to nonshared environment. (Refer to Carey [64] for a general review of phobias and Fyer [65] for a review of social phobia.)
OCD
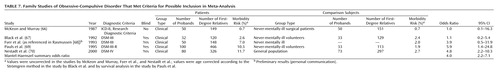
There were four family studies of OCD that met our inclusion criteria, plus one more that we included in Table 7, although its assessment of relatives was not blind to proband status. Separately, the family study data provided mixed support for the familial aggregation of OCD. Taken together, however, there was a significant association between OCD in the probands and OCD in their first-degree relatives (Mantel-Haenszel statistic=25.1, df=1, p<0.0001). In addition, the hypothesis that the odds ratios across the five studies were homogeneous could not be rejected (Breslow-Day χ2=4.48, df=4, p=0.34), which allowed us to calculate the Mantel-Haenszel summary odds ratio across the five studies, 4.0 (95% CI=2.2–7.1), which lent further support for the familial aggregation of OCD. The unadjusted aggregate risk based on 1,209 total first-degree relatives of the probands with OCD was 8.2%, compared to 2.0% in 746 comparison relatives. The family studies not meeting our inclusion criteria are cited in the References (71–84).
We could not identify any twin studies of OCD that met our inclusion criteria. The study by Carey and Gottesman (52), mentioned in the Phobias section of this report, included twin concordance rates for treatment of obsessive and compulsive symptoms. Other twin studies of obsessive-compulsive symptoms, obsessive-compulsive neurosis, or OCD were found (30, 39, 43, 85–89). Although these studies provided insight into the potential genetic basis of variables that are related to the OCD phenotype, speculations on the common genetic basis between these variables and OCD are outside of the scope of this article. (For reviews of the genetics of OCD, see references 68, 90–93.)
Discussion
Results
The results of this meta-analysis strongly support the following conclusions:
1. Panic disorder, generalized anxiety disorder, phobias, and OCD aggregate in families; the strongest evidence exists for panic disorder, for which the most data exist. The summary odds ratios are similar across the disorders, ranging from about 4 to 6.
2. The major source of familial risk is genetic. This is supported by two large-scale twin studies of panic disorder and generalized anxiety disorder and one of phobias. Since we know of no adoption studies on anxiety disorders, twin studies are the only available means of differentiating potential genetic versus common familial environmental etiologies for their familial aggregation. The models used to proportion the variance in liability into either genetic or familial environmental sources are based on the assumption that greater intrapair resemblance of monozygotic versus dizygotic twins for a phenotype is due to their greater genetic resemblance rather than any greater similarity of their environment, also known as the equal-environments assumption. Our studies from the Virginia Twin Registry included examination of various measures of common environment as possible sources of violation of this assumption; we came to consistently negative conclusions. Also, there have been several direct investigations of the equal-environments assumption in twin studies supportive of its validity (94–96).
3. Estimated heritabilities across the disorders are in the modest range, 30%–40%, significantly lower than for disorders such as schizophrenia and bipolar disorder. This leaves the largest proportion of the variance in liability to be mostly explained by individual environmental factors. This value, however, most likely represents an underestimation of true heritability. This is owing to the fact that measurement error (including diagnostic reliability and stability) and gene-environment interactions not accounted for in the models lead to inflation of estimates of the impact of specific environment. For example, our group recently performed an analysis of phobias that took into account measurement error by including data from two assessments of the same sample 8 years apart (62). The resulting estimated heritabilities across the phobias were in the 50%–60% range, compared to the point estimates of 30%–40% displayed in Table 6.
We limited our analysis to studies involving anxiety disorders. The relationship between anxiety symptoms seen in unselected individuals compared to those affected with an anxiety disorder is unclear. If symptoms and disorders exist on a single quantitative continuum based on number, severity, duration, and the like, then studies of anxiety symptoms may be informative regarding the genetics of anxiety disorders. Twin studies have indeed found genetic contributions to nonspecific anxiety symptoms (97), fears (53, 54, 56, 57, 60, 62, 98–100), symptoms of panic-phobia (101), and obsessions and compulsions (52, 88, 102).
Limitations
There are several potential limitations on the interpretation of these results. First, we may not have included all primary studies, owing either to their unavailability in the literature or to our exclusion criteria. It is unclear what impact this choice of quality versus quantity of information had on our summary statistics, but we predict that correlations between relatives would be diluted by using less rigorous standards, lowering estimates of familial aggregation and heritability. Second, because of the scarcity of twin studies for phobias and OCD, the validity and generalizability of the data for these disorders are limited compared to data for panic disorder and generalized anxiety disorder. Third, the relative contribution of genetic verses family environment is based on twin studies only, as adoption studies were not available and family studies do not provide these estimates. Finally, as previously discussed, since our genetic information is limited to twin samples, any undetected violations of the equal-environments assumption might lower the heritability estimates from those presented.
 |
 |
 |
 |
 |
 |
 |
Received Nov. 22, 2000; revision received March 22, 2001; accepted April 26, 2001. From the Virginia Institute for Psychiatric and Behavioral Genetics, Departments of Psychiatry and Human Genetics, Medical College of Virginia, Virginia Commonwealth University. Address reprint requests to Dr. Kendler, Virginia Institute for Psychiatric and Behavioral Genetics, Department of Psychiatry, P.O. Box 980126, Richmond, VA 23298-0126; [email protected] (e-mail). Funded by NIMH Training Fellowship grant MH-20030 (to Dr. Hettema), grant MH-01458 (to Dr. Neale), and grant MH-49492 (to Dr. Kendler).
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
2. Noyes R Jr, Hoehn-Saric R: The Anxiety Disorders. Cambridge, UK, Cambridge University Press, 1998Google Scholar
3. Maser JD, Cloninger CR (eds): Comorbidity of Mood and Anxiety Disorders. Washington, DC, American Psychiatric Press, 1990Google Scholar
4. Andrews G, Sanderson K, Beard J: Burden of disease: methods of calculating disability from mental disorder. Br J Psychiatry 1998; 173:123-131Crossref, Medline, Google Scholar
5. Olfson M, Fireman B, Weissman MM, Leon AC, Sheehan DV, Kathol RG, Hoven C, Farber L: Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry 1997; 154:1734-1740Link, Google Scholar
6. Rubin HC, Rapaport MH, Levine B, Gladsjo JK, Rabin A, Auerbach M, Judd LL, Kaplan R: Quality of well being in panic disorder: the assessment of psychiatric and general disability. J Affect Disord 2000; 57:217-221Crossref, Medline, Google Scholar
7. Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, Street L, Del Bene D, Liebowitz MR: Functional impairment in social phobia. J Clin Psychiatry 1994; 55:322-331Medline, Google Scholar
8. Kessler RC, DuPont RL, Berglund P, Wittchen H-U: Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. Am J Psychiatry 1999; 156:1915-1923Link, Google Scholar
9. Marks IM: Genetics of fear and anxiety disorders. Br J Psychiatry 1986; 149:406-418Crossref, Medline, Google Scholar
10. Khoury MJ, Beaty TH, Cohen BH: Fundamentals of Genetic Epidemiology. New York, Oxford University Press, 1993Google Scholar
11. Ridenour TA, Heath AC: A note on issues in meta-analysis for behavioral genetic studies using categorical phenotypes. Behav Genet 1999; 29:155-162Crossref, Medline, Google Scholar
12. Breslow NE, Day NE: Statistical Methods in Cancer Research, vol 1. Lyon, France, International Agency for Research on Cancer, 1980Google Scholar
13. Mantel N, Haenszel W: Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22:719-748Medline, Google Scholar
14. SAS/STAT Software, version 8. Cary, NC, SAS Institute, 1999Google Scholar
15. Kendler KS, Prescott CA: A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry 1999; 56:39-44Crossref, Medline, Google Scholar
16. Scherrer JF, True WR, Xian H, Lyons MJ, Eisen SA, Goldberg J, Lin N, Tsuang MT: Evidence for genetic influences common and specific to symptoms of generalized anxiety and panic. J Affect Disord 2000; 57:25-35Crossref, Medline, Google Scholar
17. Neale MC, Cardon LR: Methodology for Genetic Studies of Twins and Families. Dordrecht, the Netherlands, Kluwer Academic, 1992Google Scholar
18. Neale MC, Boker SM, Xie G, Maes HH: Mx: Statistical Modeling, 5th ed. Richmond, Medical College of Virginia of Virginia Commonwealth University, Department of Psychiatry, 1999Google Scholar
19. Noyes R Jr, Crowe RR, Harris EL, Hamra BJ, McChesney CM, Chaudhry DR: Relationship between panic disorder and agoraphobia: a family study. Arch Gen Psychiatry 1986; 43:227-232Crossref, Medline, Google Scholar
20. Mendlewicz J, Papadimitriou GN, Wilmotte J: Family study of panic disorder: comparison with generalized anxiety disorder, major depression and normal subjects. Psychiatr Genet 1993; 3:73-78Crossref, Google Scholar
21. Maier W, Lichtermann D, Minges J, Oehrlein A, Franke P: A controlled family study in panic disorder. J Psychiatr Res 1993; 27(suppl 1):79-87Google Scholar
22. Horwath E, Wolk SI, Goldstein RB, Wickramaratne P, Sobin C, Adams P, Lish JD, Weissman MM: Is the comorbidity between social phobia and panic disorder due to familial cotransmission or other factors? Arch Gen Psychiatry 1995; 52:574-582Crossref, Medline, Google Scholar
23. Fyer AJ, Mannuzza S, Chapman TF, Lipsitz J, Martin LY, Klein DF: Panic disorder and social phobia: effects of comorbidity on familial transmission. Anxiety 1996; 2:173-178Crossref, Medline, Google Scholar
24. Crowe RR, Noyes R, Pauls DL, Slymen D: A family study of panic disorder. Arch Gen Psychiatry 1983; 40:1065-1069Crossref, Medline, Google Scholar
25. Harris EL, Noyes R Jr, Crowe RR, Chaudhry DR: Family study of agoraphobia: report of a pilot study. Arch Gen Psychiatry 1983; 40:1061-1064Crossref, Medline, Google Scholar
26. Weissman MM, Wickramaratne P, Adams PB, Lish JD, Horwath E, Charney D, Woods SW, Leeman E, Frosch E: The relationship between panic disorder and major depression: a new family study. Arch Gen Psychiatry 1993; 50:767-780Crossref, Medline, Google Scholar
27. Goldstein RB, Weissman MM, Adams PB, Horwath E, Lish JD, Charney D, Woods SW, Sobin C, Wickramaratne PJ: Psychiatric disorders in relatives of probands with panic disorder and/or major depression. Arch Gen Psychiatry 1994; 51:383-394Crossref, Medline, Google Scholar
28. Goldstein RB, Wickramaratne PJ, Horwath E, Weissman MM: Familial aggregation and phenomenology of “early”-onset (at or before age 20 years) panic disorder. Arch Gen Psychiatry 1997; 54:271-278Crossref, Medline, Google Scholar
29. Hopper JL, Judd FK, Derrick PL, Burrows GD: A family study of panic disorder. Genet Epidemiol 1987; 4:33-41Crossref, Medline, Google Scholar
30. Skre I, Onstad S, Torgersen S, Lygren S, Kringlen E: A twin study of DSM-III-R anxiety disorders. Acta Psychiatr Scand 1993; 88:85-92Crossref, Medline, Google Scholar
31. Gruppo Italiano Disturbi d’Ansia: Familial analysis of panic disorder and agoraphobia. J Affect Disord 1989; 17:1-8Crossref, Medline, Google Scholar
32. Moran C, Andrews G: The familial occurrence of agoraphobia. Br J Psychiatry 1985; 146:262-267Crossref, Medline, Google Scholar
33. Weissman MM: Family genetic studies of panic disorder. J Psychiatr Res 1993; 27(suppl 1):69-78Google Scholar
34. Knowles JA, Weissman MM: Panic disorder and agoraphobia, in The American Psychiatric Press Review of Psychiatry, vol 14. Edited by Oldham JM, Riba MB. Washington, DC, American Psychiatric Press, 1995, pp 383-404Google Scholar
35. Woodman CL: The genetics of panic disorder and generalized anxiety disorder. Ann Clin Psychiatry 1993; 5:231-239Crossref, Medline, Google Scholar
36. Marazziti D, Rotondo A: Genetics of panic disorder. CNS Spectrums 1999; 4:62-70Medline, Google Scholar
37. Perna G, Caldirola D, Arancio C, Bellodi L: Panic attacks: a twin study. Psychiatry Res 1997; 66:69-71Crossref, Medline, Google Scholar
38. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Panic disorder in women: a population-based twin study. Psychol Med 1993; 23:397-406Crossref, Medline, Google Scholar
39. Torgersen S: Genetic factors in anxiety disorders. Arch Gen Psychiatry 1983; 40:1085-1089Crossref, Medline, Google Scholar
40. Noyes R Jr, Clarkson C, Crowe RR, Yates WR, McChesney CM: A family study of generalized anxiety disorder. Am J Psychiatry 1987; 144:1019-1024Link, Google Scholar
41. Hettema JM, Prescott CA, Kendler KS: A population-based study of generalized anxiety disorder in men and women. J Nerv Ment Dis (in press)Google Scholar
42. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Generalized anxiety disorder in women: a population-based twin study. Arch Gen Psychiatry 1992; 49:267-272Crossref, Medline, Google Scholar
43. Andrews G, Stewart G, Allen R, Henderson AS: The genetics of six neurotic disorders: a twin study. J Affect Disord 1990; 19:23-29Crossref, Medline, Google Scholar
44. Roy M-A, Neale MC, Pedersen NL, Mathe AA, Kendler KS: A twin study of generalized anxiety disorder and major depression. Psychol Med 1995; 25:1037-1049Crossref, Medline, Google Scholar
45. Fyer AJ, Mannuzza S, Chapman TF, Martin LY, Klein DF: Specificity in familial aggregation of phobic disorders. Arch Gen Psychiatry 1995; 52:564-573Crossref, Medline, Google Scholar
46. Mannuzza S, Schneier FR, Chapman TF, Liebowitz MR, Klein DF, Fyer AJ: Generalized social phobia: reliability and validity. Arch Gen Psychiatry 1995; 52:230-237Crossref, Medline, Google Scholar
47. Stein MB, Chartier MJ, Hazen AL, Kozak MV, Tancer ME, Lander S, Furer P, Chubaty D, Walker JR: A direct-interview family study of generalized social phobia. Am J Psychiatry 1998; 155:90-97Link, Google Scholar
48. Fyer AJ, Mannuzza S, Gallops MS, Martin LY, Aaronson C, Gorman JM, Liebowitz MR, Klein DF: Familial transmission of simple phobias and fears: a preliminary report. Arch Gen Psychiatry 1990; 47:252-256Crossref, Medline, Google Scholar
49. Fyer AJ, Mannuzza S, Chapman TF, Liebowitz MR, Klein DF: A direct interview family study of social phobia. Arch Gen Psychiatry 1993; 50:286-293Crossref, Medline, Google Scholar
50. Reich J, Yates W: Family history of psychiatric disorders in social phobia. Compr Psychiatry 1988; 29:72-75Crossref, Medline, Google Scholar
51. Mancini C, van Ameringen M, Szatmari P, Fugere C, Boyle M: A high-risk pilot study of the children of adults with social phobia. J Am Acad Child Adolesc Psychiatry 1996; 35:1511-1517Crossref, Medline, Google Scholar
52. Carey G, Gottesman II: Twin and family studies of anxiety, phobic, and obsessive disorders, in Anxiety: New Research and Changing Concepts. Edited by Klein DF, Rabkin J. New York, Raven Press, 1981, pp 117-136Google Scholar
53. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: The genetic epidemiology of phobias in women: the interrelationship of agoraphobia, social phobia, situational phobia, and simple phobia. Arch Gen Psychiatry 1992; 49:273-281Crossref, Medline, Google Scholar
54. Neale MC, Walters EE, Eaves LJ, Kessler RC, Heath AC, Kendler KS: Genetics of blood-injury fears and phobias: a population-based twin study. Am J Med Genet 1994; 54:326-334Crossref, Medline, Google Scholar
55. Kendler KS, Myers J, Prescott CA, Neale MC: The genetic epidemiology of irrational fears and phobias in men. Arch Gen Psychiatry 2001; 58:257-265Crossref, Medline, Google Scholar
56. Torgersen S: The nature and origin of common phobic fears. Br J Psychiatry 1979; 134:343-351Crossref, Medline, Google Scholar
57. Rose RJ, Ditto WB: A developmental-genetic analysis of common fears from early adolescence to early adulthood. Child Dev 1983; 54:361-368Crossref, Medline, Google Scholar
58. Phillips K, Fulker DW, Rose RJ: Path analysis of seven fear factors in adult twin and sibling pairs and their parents. Genet Epidemiol 1987; 4:345-355Crossref, Medline, Google Scholar
59. Stevenson J, Batten N, Cherner M: Fears and fearfulness in children and adolescents: a genetic analysis of twin data. J Child Psychol Psychiatry 1992; 33:977-985Crossref, Medline, Google Scholar
60. Page AC, Martin NG: Testing a genetic structure of blood-injury-injection fears. Am J Med Genet 1998; 81:377-384Crossref, Medline, Google Scholar
61. Neale MC, Eaves LJ, Kendler KS: The power of the classical twin study to resolve variation in threshold traits. Behav Genet 1994; 24:239-258Crossref, Medline, Google Scholar
62. Kendler KS, Karkowski LM, Prescott CA: Fears and phobias: reliability and heritability. Psychol Med 1999; 29:539-553Crossref, Medline, Google Scholar
63. Nelson EC, Grant JD, Bucholz KK, Glowinski A, Madden PAF, Reich W, Heath AC: Social phobia in a population-based female adolescent twin sample: co-morbidity and associated suicide-related symptoms. Psychol Med 2000; 30:797-804Crossref, Medline, Google Scholar
64. Carey G: Genes, fears, phobias, and phobic disorders. J Counseling and Development 1990; 68:628-632Crossref, Google Scholar
65. Fyer AJ: Heritability of social anxiety: a brief review. J Clin Psychiatry 2000; 54:10-12Google Scholar
66. McKeon P, Murray R: Familial aspects of obsessive-compulsive neurosis. Br J Psychiatry 1987; 151:528-534Crossref, Medline, Google Scholar
67. Black DW, Noyes R Jr, Goldstein RB, Blum N: A family study of obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49:362-368Crossref, Medline, Google Scholar
68. Rasmussen SA: Genetic studies of obsessive-compulsive disorder. Ann Clin Psychiatry 1993; 5:241-247Crossref, Medline, Google Scholar
69. Pauls DL, Alsobrook JP, Goodman W, Rasmussen S, Leckman JF: A family study of obsessive-compulsive disorder. Am J Psychiatry 1995; 152:76-84Link, Google Scholar
70. Nestadt G, Samuels J, Riddle M, Bienvenu OJ III, Liang KY, LaBuda M, Walkup J, Grados M, Hoehn-Saric R: A family study of obsessive-compulsive disorder. Arch Gen Psychiatry 2000; 57:358-363Crossref, Medline, Google Scholar
71. Lewis A: Problems of obsessional illness. Proc R Soc Med 1936; 29:325-336Medline, Google Scholar
72. Brown FW: Heredity in the psychoneuroses. Proc R Soc Med 1942; 35:785-790Medline, Google Scholar
73. Rudin E: Ein beitrag zur frage der zwangskrankheit insbesondere ihrer hereditaren beziehungen. Arch Psychiatrische Nervenkrankheit 1953; 191:14-54Crossref, Google Scholar
74. Kringlen E: Obsessional neurotics: a long-term follow-up. Br J Psychiatry 1965; 111:700-722Crossref, Google Scholar
75. Lo WH: A follow-up study of obsessional neurotics in Hong Kong Chinese. Br J Psychiatry 1967; 113:823-832Crossref, Medline, Google Scholar
76. Rosenberg CM: Familial aspects of obsessional neurosis. Br J Psychiatry 1967; 113:405-413Crossref, Medline, Google Scholar
77. Insel TR, Hoover C, Murphy DL: Parents of patients with obsessive-compulsive disorder. Psychol Med 1983; 13:807-811Crossref, Medline, Google Scholar
78. Rasmussen SA, Tsuang MT: Clinical characteristics and family history in DSM-III obsessive-compulsive disorder. Am J Psychiatry 1986; 143:317-322Link, Google Scholar
79. Lenane MC, Swedo SE, Leonard H, Pauls DL, Sceery W, Rapoport JL: Psychiatric disorders in first degree relatives of children and adolescents with obsessive compulsive disorder. J Am Acad Child Adolesc Psychiatry 1990; 29:407-412Crossref, Medline, Google Scholar
80. Riddle MA, Scahill L, King R, Hardin MT, Towbin KE, Ort SI, Leckman JF, Cohen DJ: Obsessive compulsive disorder in children and adolescents: phenomenology and family history. J Am Acad Child Adolesc Psychiatry 1990; 29:766-772Crossref, Medline, Google Scholar
81. Bellodi L, Sciuto G, Diaferia G, Ronchi P, Smeraldi E: Psychiatric disorders in the families of patients with obsessive-compulsive disorder. Psychiatry Res 1992; 42:111-120Crossref, Medline, Google Scholar
82. Nicolini H, Weissbecker K, Mejia JM, Sanchez de Carmona M: Family study of obsessive-compulsive disorder in a Mexican population. Arch Med Res 1993; 24:193-198Medline, Google Scholar
83. Thomsen PH: Obsessive-compulsive disorder in children and adolescents: a study of parental psychopathology and precipitating events in 20 consecutive Danish cases. Psychopathology 1995; 28:161-167Crossref, Medline, Google Scholar
84. Sciuto G, Pasquale L, Bellodi L: Obsessive compulsive disorder and mood disorders: a family study. Am J Med Genet 1995; 60:475-479Crossref, Medline, Google Scholar
85. Inouye E: Similar and dissimilar manifestations of obsessive-compulsive neurosis in monozygotic twins. Am J Psychiatry 1965; 121:1171-1175Link, Google Scholar
86. Marks IM, Crowe M, Drewe E, Young J, Dewhurst WG: Obsessive-compulsive neurosis in identical twins. Br J Psychiatry 1969; 115:991-998Crossref, Medline, Google Scholar
87. McGuffin P, Mawson D: Obsessive compulsive neurosis: two concordant twin pairs. Br J Psychiatry 1980; 137:285-287Crossref, Medline, Google Scholar
88. Clifford CA, Murray RM, Fulker DW: Genetic and environmental influences on obsessional traits and symptoms. Psychol Med 1984; 14:791-800Crossref, Medline, Google Scholar
89. Kim SW, Dysken MW, Kline MD: Monozygotic twins with obsessive-compulsive disorder. Br J Psychiatry 1990; 156:435-438Crossref, Medline, Google Scholar
90. Rasmussen SA, Tsuang MT: The epidemiology of obsessive compulsive disorder. J Clin Psychiatry 1984; 45:450-457Medline, Google Scholar
91. Black DW: Epidemiology and genetics of OCD: a review and discussion of future directions for research. CNS Spectrums 1996; 1:10-16Google Scholar
92. Nicolini H, Cruz C, Camarena B, Paez F, De La Fuente JR: Understanding the genetic basis of obsessive-compulsive disorder. CNS Spectrums 1999; 4:32-48Crossref, Medline, Google Scholar
93. Pauls DL, Alsobrook JP: The inheritance of obsessive-compulsive disorder. Child Adolesc Psychiatr Clin North Am 1999; 8:481-496Crossref, Medline, Google Scholar
94. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: A test of the equal environment assumption in twin studies of psychiatric illness. Behav Genet 1993; 23:21-27Crossref, Medline, Google Scholar
95. Hettema JM, Neale MC, Kendler KS: Physical similarity and the equal-environment assumption in twin studies of psychiatric disorders. Behav Genet 1995; 25:327-335Crossref, Medline, Google Scholar
96. Kendler KS, Gardner CO Jr: Twin studies of adult psychiatric and substance dependence disorders: are they biased by differences in the environmental experiences of monozygotic and dizygotic twins in childhood and adolescence? Psychol Med 1998; 28:625-633Crossref, Medline, Google Scholar
97. Jardine R, Martin NG, Henderson AS: Genetic covariation between neuroticism and the symptoms of anxiety and depression. Genet Epidemiol 1984; 1:89-107Crossref, Medline, Google Scholar
98. Rose RJ, Miller JZ, Pogue-Geile MF, Cardwell GF: Twin-family studies of common fears and phobias. Prog Clin Biol Res 1981; 69(part B):169-174Google Scholar
99. Neale MC, Walters EE, Eaves LJ, Maes HH, Kendler KS: Multivariate genetic analysis of twin-family data on fears: Mx models. Behav Genet 1994; 24:119-139Crossref, Medline, Google Scholar
100. Neale MC, Fulker DW: A bivariate path analysis of fear data on twins and their parents. Acta Genet Med Gemellol (Roma) 1984; 33:273-286Crossref, Medline, Google Scholar
101. Kendler KS, Walters EE, Truett KR, Heath AC, Neale MC, Martin NG, Eaves LJ: A twin-family study of self-report symptoms of panic-phobia and somatization. Behav Genet 1995; 25:499-515Crossref, Medline, Google Scholar
102. Jonnal AH, Gardner CO, Prescott CA, Kendler KS: Obsessive and compulsive symptoms in a general population sample of female twins. Am J Med Genet 2000; 96:791-796Crossref, Medline, Google Scholar



