Morbidity Risk for Obsessive-Compulsive Spectrum Disorders in First-Degree Relatives of Patients With Eating Disorders
Abstract
OBJECTIVE: A hypothesis that eating disorders are a phenomenological variant of obsessive-compulsive disorder (OCD) has been proposed. This study was conducted to determine whether anorexia nervosa and bulimia, the two main eating disorders, are familial and whether the risk for obsessive-compulsive spectrum disorders (OCD and tic disorders) is higher in families of patients with eating disorders. METHOD: The morbidity risk for obsessive-compulsive spectrum disorders in first-degree relatives of 136 female probands with eating disorders (84 with anorexia nervosa, 52 with bulimia) was compared to that for first-degree relatives of 72 female comparison subjects. RESULTS: The morbidity risk for obsessive-compulsive spectrum disorders was significantly higher among the 436 relatives of the eating disorder probands than among the 358 relatives of the comparison subjects (9.69% versus 0%). This finding was independent of any comorbid diagnosis of an obsessive-compulsive spectrum disorder in the eating disorder probands. The eating disorder group and the comparison group did not differ in familial risk for eating disorders and tic disorders. CONCLUSIONS: To better understand the genetic components of eating disorders, these disorders should be considered as part of the obsessive-compulsive spectrum of disorders.
Several hypotheses that have advanced a common etiopathological background for eating disorders have linked cultural, environmental, genetic, physiological, and psychological factors to risk for these disorders (1). Genetic predisposing factors to anorexia nervosa and bulimia nervosa have been investigated separately in twin and familial studies. Twins studies have found concordance rates for anorexia nervosa of 48.5%–71.0% among monozygotic twins and 0%–10% among dizygotic twins (2–4). Concordance rates for bulimia range from 22.9%–83.0% for monozygotic twins and 0%–27.0% for dizygotic twins (5–7).
Family studies suggest that first-degree relatives of anorexia nervosa probands have a risk rate of 2%–8% for anorexia nervosa and 1.0%–4.7% for bulimia (8–16). The familial risk for bulimia in first-degree relatives of probands with bulimia has been observed to range from 0% (17) to 9.6% (18). Lilenfeld et al. (19) noted a higher familial risk only for subthreshold forms of eating disorders both in anorexia nervosa probands and bulimia probands.
The high prevalence of depressive symptoms in patients with eating disorders has led many researchers to focus on risk for affective disorders in the families of those patients. However, interest in the relationship between eating disorders and anxiety disorders has increased (20). In particular, researchers have hypothesized that eating disorders are part of the obsessive-compulsive spectrum of disorders, which includes obsessive-compulsive disorder (OCD) and tic disorders/Tourette’s syndrome. Several authors have suggested that anorexia nervosa could be considered a form of OCD (21–26). Lilenfeld et al. (19) found an elevated risk for obsessive-compulsive personality disorder but not for OCD among the relatives of anorexia nervosa probands.
The co-occurrence of eating disorders and OCD has been correlated with severity of eating disorders (27–29) but has not been associated with specific eating disorder diagnoses (30). The relationship between eating disorders and OCD has also been suggested by a higher rate of a lifetime diagnosis of eating disorder in OCD patients (8.3%–12.0%) than in the general population (1% for anorexia nervosa and 4% for bulimia) (14, 31–34).
The obsessive and compulsive behaviors often observed in patients with eating disorders, regardless of whether the behaviors are related to food, have generally been assumed to be caused or even exacerbated by malnutrition. Keys et al. (35) observed that normal subjects under conditions of semistarvation developed a range of anorexic and obsessional features.
To test the hypothesis that eating disorders and OCD have a common etiopathogenetic background, we studied the prevalence of obsessive-compulsive spectrum disorders (36–38) in the first-degree relatives of probands with eating disorders. Assuming a link between eating disorders and obsessive-compulsive spectrum disorders, we expected a higher frequency of these disorders among first-degree relatives of eating disorder probands than in a group of comparison subjects from the general population.
Method
Subjects
Eating disorder probands
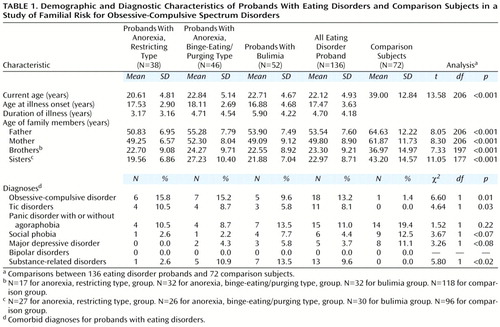
A total of 136 female patients with eating disorders were recruited over an 18-month period from consecutive admissions to the eating disorders center of San Raffaele Hospital in Milan, Italy. The patients’ clinical diagnoses, determined with DSM-IV criteria for eating disorders, were anorexia nervosa, restricting type, for 38 patients; anorexia nervosa, binge eating/purging type, for 46 patients; and bulimia for 52 patients. The subjects’ demographic and clinical characteristics are reported in Table 1.
After the patients were enrolled, their permission was obtained to contact and interview their first-degree relatives. Clinical information was obtained for 436 biological first-degree relatives of the eating disorder probands. A total of 300 of these relatives—136 pairs of parents, 81 brothers, and 83 sisters—were evaluated directly by the study team.
Comparison group
The comparison subjects were 72 female surgical patients treated for knee pathologies at the day hospital of San Raffaele Hospital. These patients were consecutively seen over a 4-month screening period (refusal rate, 27%) and have been described elsewhere (39). These individuals represented the general population. After asking the comparison subjects’ permission to contact their first-degree relatives, family histories of possible psychiatric disorders were collected for 358 first-degree relatives (72 pairs of parents, 118 brothers, and 96 sisters) with the help of the proband and one first-degree relative as an informant.
Diagnostic Procedures
Eligibility criteria
Patients who were clinically diagnosed with eating disorders were eligible for the study if they provided informed consent and had their diagnosis confirmed independently by a clinician using the National Institute of Mental Health Diagnostic Interview Schedule (DIS) (40). The DSM-III-R and DSM-IV criteria for eating disorders are the same, but subtypes of anorexia nervosa are distinguished in DSM-IV. We used available clinical information to classify each anorexic individual according to the DSM-IV anorexia subtypes. Patients with an eating disorder not otherwise specified (12.3% of the 155 patients originally recruited for the study) were excluded from the study. The age at onset of the eating disorder was defined as the earliest age at which the proband fully satisfied criteria for a DSM-IV diagnosis of eating disorder. The method described for evaluation of the eating disorder probands was also used for the comparison group.
Family history interviews
After the proband’s diagnoses had been confirmed and the family pedigree drawn, the relatives of the proband were contacted individually. The relatives who provided written informed consent were evaluated by a clinician with the DIS. The DIS was administered to 75% of the fathers, 79% of the mothers, 4% of the brothers, and 9% of the sisters of the probands. The high refusal rate among the siblings was due partly to the young age of many siblings (<18 years).
The interviewers were blind to the proband’s diagnosis. However, complete blindness may have been hampered owing to the anorectic appearance of some probands and to probands’ or relatives’ comments about diagnoses, specific somatic treatments, or treatment settings.
Interviewers obtained clinical information on the psychiatric family history of the relatives who were not directly interviewed by using the DIS sequence of questions with the proband and at least one first-degree relative as informants. DSM-IV diagnoses were generated for each first-degree relative.
Data Analysis
The significance of the difference in age between the eating disorder probands and the comparison subjects was assessed with Student’s t test. Analysis of variance was used to assess differences among eating disorder subgroups in current age and age at onset of the disorder. Chi-square analysis was used to assess any differences in frequency of comorbid psychiatric diagnoses between the eating disorder probands and the comparison subjects.
We evaluated the morbidity risk for eating disorders, OCD, and tic disorders/Tourette’s syndrome, both together and separately, in the first-degree relatives of the three subgroups of eating disorder probands and of the comparison subjects. For each group, the morbidity risk was computed as the ratio between the number of affected individuals and number of affected individuals plus the number of at-risk individuals.
An appropriate age correction for unaffected relatives at risk was introduced for each study group. The distribution of age at onset of OCD, eating disorders, and tic disorders/Tourette’s syndrome in three separate groups of patients treated at San Raffaele Hospital (107 patients with OCD, 120 patients with eating disorders, and 40 patients with tic disorders/Tourette’s syndrome) was evaluated with the survival analysis stepwise method, as implemented with BMDP statistical software (41). Age at onset was the dependent variable in the model, and gender was the covariate. From those distributions, we obtained the probability of being affected with the various disorders and the corresponding age correction for subjects at risk among the first-degree relatives of the eating disorder probands and the comparison subjects.
To avoid limitations due to the lack of statistical independence in the analysis of affected relatives, we used chi-square tests to compare the distributions of families with either no members or with one or more members affected with eating disorders or obsessive-compulsive spectrum disorders in each subgroup of eating disorder probands and in the comparison group. Data for nuclear families were analyzed. We performed the analyses by using various definitions of the affected phenotype in the relatives, including eating disorders, OCD, tic disorder, OCD plus tic disorders (obsessive-compulsive spectrum disorders), and eating disorders plus obsessive-compulsive spectrum disorders.
Results
Current age and age at onset of eating disorder of the eating disorder probands did not differ significantly in the three eating disorder subgroups (Table 1). The mean duration of illness was significantly different among the three groups (F=5.20, df=2, 135, p<0.007); the probands affected with anorexia, restricting type, had a markedly shorter duration of illness than did the probands with bulimia. This difference may have been related to the tendency of persons with the restricting type of anorexia to seek psychiatric consultation earlier, given the severity of their physical symptoms.
The eating disorder probands and the comparison subjects differed significantly in current age. The first-degree relatives of the eating disorder probands differed significantly in age from the first-degree relatives of the comparison subjects.
Analysis of the frequency of comorbid diagnoses showed that the eating disorder probands differed significantly from the comparison subjects in the proportion of subjects with a diagnosis of OCD, tic disorders, and substance-related disorders (Table 1). No significant differences for other psychiatric diagnoses were observed.
The total study group included relatives who were directly interviewed and relatives who were not directly interviewed. The diagnoses of the relatives who were not interviewed were made on the basis of family history information. This procedure may have underestimated psychiatric morbidity. Nevertheless, the morbidity risk for obsessive-compulsive spectrum disorders and eating disorders for the interviewed relatives (9.01%) and for the relatives who were not interviewed (13.71%) was not significantly different (z test for differences between proportions=1.45, p=0.15); therefore, we grouped the interviewed relatives together with the relatives who were not interviewed in the analyses. We compared the overall group of eating disorder probands and their relatives with the comparison subjects and their relatives. We also compared each subgroup of eating disorder probands and their relatives with the comparison subjects and their relatives, introducing the Bonferroni correction for multiple testing for each set of comparisons (seven tests in each set) (significant p value=0.05/7, or p≤0.0071).
Eating Disorders
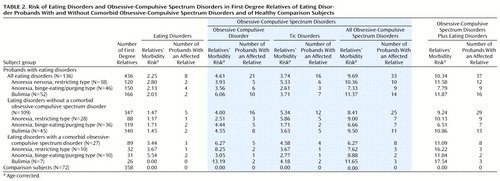
We determined the number of families in which an eating disorder occurred in a first-degree relative of the eating disorder proband or the comparison subject (Table 2). The number of families with affected relatives was no greater in the eating disorder group than in the comparison group (χ2=2.96, df=1, p=0.09). No differences between groups were observed in the number of families with affected parents (χ2=0.43, df=1, p=0.51) or in the number of families with affected siblings (χ2=1.37, df=1, p=0.24).
OCD
The morbidity risk for OCD in the first-degree relatives of the 136 eating disorder probands, corrected for age, was calculated (Table 2).
A significant difference in the number of first-degree relatives with OCD was found between the overall group of families of eating disorder probands and the comparison families (χ2=12.37, df=2, p=0.002). There was no significant difference between groups in the number of parents with OCD (χ2=5.22, df=1, p=0.02). However, the siblings of probands with bulimia were significantly more likely to have a diagnosis of OCD than were the siblings of the comparison subjects (χ2=7.9, df=1, p=0.005).
The morbidity risk for OCD was analyzed separately in the families of eating disorder probands without and with a comorbid diagnosis of an obsessive-compulsive spectrum disorder (109 families and 27 families, respectively). The first-degree relatives in the families of the 109 probands without a comorbid obsessive-compulsive spectrum disorder were significantly more likely to have OCD than were the relatives of the comparison subjects (χ2=9.84, df=1, p=0.002), but there was no significant difference in the number of relatives with OCD between the subgroup of 28 probands with anorexia, restricting type, and the comparison group (χ2=4.70, df=1, p=0.03) (Table 2). There were no significant differences between the families of the 109 probands and the comparison families in the number of parents with OCD (χ2=5.35, df=1, p=0.02) or the number of siblings with OCD (χ2=2.56, df=1, p=0.11).
The first-degree relatives in the families of the 27 eating disorder probands with a comorbid obsessive-compulsive spectrum disorder were significantly more likely to have OCD than were the relatives of the comparison subjects (χ2=14.04, df=2, p<0.0001), but there was no significant difference in the number of relatives with OCD between the subgroup of 10 probands with anorexia, binge-eating/purging type, and the comparison group (χ2=1.35, df=1, p=0.25) (Table 2). The parents of the 27 eating disorder probands with a comorbid obsessive-compulsive spectrum disorder were more likely to have OCD than the parents of the comparison subjects (χ2=10.45, df=1, p=0.001), even though the parents of the 10 probands with anorexia, binge-eating/purging type, were no more likely to have OCD than the parents of the comparison subjects (χ2=1.35, df=1, p=0.25). The siblings in the 27 families of eating disorder probands with a comorbid obsessive-compulsive spectrum disorder were no more likely to have OCD than siblings in the comparison families (χ2=0.26, df=1, p=0.61).
No intergroup differences were observed among the relatives of the various subgroups of eating disorder probands.
Tic Disorders
The first-degree relatives in the overall group of eating disorder probands were not significantly more likely to have a tic disorder than were the relatives of the comparison subjects (χ2=9.18, df=2, p=0.01) (Table 2). However, tic disorders were significantly more likely among the relatives of the probands with bulimia (χ2=10.27, df=2, p=0.006) and among the relatives of the probands with anorexia, restricting type (χ2=9.16, df=1, p=0.002), than among the relatives of the comparison subjects.
The first-degree relatives in the families of the 109 eating disorder probands without a comorbid obsessive-compulsive spectrum disorder were no more likely to have a tic disorder than were the relatives of the comparison subjects (χ2=6.80, df=1, p=0.009). However, tic disorders were significantly more likely in the families of the probands with anorexia, restricting type, without a comorbid obsessive-compulsive spectrum disorder than in the comparison families (χ2=10.04, df=1, p=0.002).
The siblings of the 27 eating disorder probands with a comorbid obsessive-compulsive spectrum disorder were more likely to have tic disorders than were the siblings of the comparison subjects (χ2=11.12, df=1, p<0.001). Tic disorders were more likely among the relatives of the probands with bulimia in these 27 families than among the relatives of the comparison subjects (χ2=7.62, df=1, p=0.006).
No intergroup differences were observed among the relatives of the various subgroups of eating disorder probands.
Obsessive-Compulsive Spectrum Disorders
The families of the eating disorder probands were significantly more likely to include first-degree relatives affected with obsessive-compulsive spectrum disorders than were the families of the comparison subjects (χ2=20.77, df=2, p<0.001) (Table 2). The parents of the eating disorder probands were significantly more likely have obsessive-compulsive spectrum disorders than the parents of the comparison subjects (χ2=10.72, df=1, p=0.001). The families of the eating disorder probands were more likely to include affected siblings than were the comparison families (χ2=8.21, df=1, p=0.004); this difference was due to the significantly higher number of affected siblings in the families of the probands with bulimia than in the comparison families (χ2=10.99, df=1, p<0.001) and the higher number of affected siblings in the families of the probands with anorexia, restricting type, than in the comparison families (χ2=7.12, df=1, p=0.008).
The families of the 109 eating disorder probands without a comorbid obsessive-compulsive spectrum disorder included significantly more first-degree relatives who were affected with these disorders than did the comparison families (χ2=19.16, df=2, p<0.001). The parents of the eating disorder probands were more likely to be affected than the parents of the comparison subjects (χ2=9.07, df=1, p=0.003); this difference was due to the higher number of affected parents in the families of the probands with bulimia and with anorexia, restricting type, than in the comparison families (χ2=9.31, df=1, p=0.002 and χ2=7.31, df=1, p=0.007, respectively). The siblings of the probands with bulimia and with anorexia, restricting type, were more likely to be affected than the siblings of the comparison subjects (χ2=7.56, df=1, p=0.006 and χ2=7.32, df=1, p=0.007, respectively).
The first-degree relatives in the subset of the 27 families of the eating disorder probands with a comorbid obsessive-compulsive spectrum disorder were more likely to have an obsessive-compulsive spectrum disorder than the relatives of the comparison subjects (χ2=23.21, df=2, p<0.001). Only the fathers of the probands with anorexia, binge-eating/purging type, were no more likely to be affected than the fathers of the comparison subjects (χ2=1.19, df=1, p=0.28). The siblings of the probands with bulimia were significantly more likely to be affected than the siblings of the comparison subjects (χ2=21.42, df=1, p<0.001).
No intergroup differences were observed among the relatives of the various subgroups of eating disorder probands.
Eating Disorders Plus Obsessive-Compulsive Spectrum Disorders
The rates of both eating disorders and obsessive-compulsive spectrum disorders were significantly higher in the first-degree relatives of the eating disorder probands than in the relatives of the comparison subjects (10.34% versus 0%) (χ2=23.83, df=2, p<0.001). The rates were higher in the relatives of the probands with anorexia, restricting type (11.3%) (χ2=25.52, df=2, p<0.001), the relatives of the probands with anorexia, binge-eating/purging type (8.1%) (χ2=15.25, df=2, p<0.001), and the relatives of the probands with bulimia (12.9%) (χ2=25.44, df=2, p<0.001), compared separately with the rate in the relatives of the comparison subjects.
No significant intergroup differences in the rate of eating disorders plus obsessive-compulsive spectrum disorders were found in the relatives of the eating disorders subgroups.
The parents and the siblings of the eating disorder probands had a significantly higher morbidity risk for these disorders than did the parents and siblings of the comparison subjects (χ2=13.03, df=2, p=0.001 and χ2=11.72, df=2, p=0.003, respectively). Only the siblings of the probands with anorexia, binge-eating/purging type, had a morbidity risk that did not differ significantly from that of the siblings of the comparison subjects (χ2=6.48, df=2, p<0.04).
The first-degree relatives of the 109 eating disorder probands without a comorbid obsessive-compulsive spectrum disorder had a significantly higher rate of both eating disorders and obsessive-compulsive spectrum disorders than the relatives of the comparison subjects (χ2=22.81, df=2, p<0.001), and the affected relatives in this subgroup accounted for most of the affected relatives in the overall group of families of the eating disorder probands. The parents of this subgroup of 109 probands were significantly more likely to have an eating disorder or an obsessive-compulsive spectrum disorder than the parents of the comparison subjects (χ2=12.39, df=2, p=0.002), and the siblings in this group were significantly more likely to be affected than the siblings of the comparison subjects (χ2=10.02, df=2, p=0.007), although the siblings of probands with anorexia, binge-eating/purging type, did not differ from the siblings of the comparison subjects in their rate of these disorders (χ2=4.08, df=3, p=0.13).
The rate of eating disorders or obsessive-compulsive spectrum disorders was higher in the families of the 27 eating disorder probands with a comorbid obsessive-compulsive spectrum disorder and in each of the eating disorder subgroups than in the comparison families (χ2=23.21, df=3, p<0.001). The parents of these 27 eating disorder probands were more likely to be affected with these disorders than the parents of the comparison subjects (χ2=14.04, df=2, p<0.001). Their siblings were more likely to be affected than the siblings of the comparison subjects (χ2=14.04, df=2, p<0.001); most of this difference was accounted for by the higher rate in the siblings of the probands with bulimia than in the siblings of the comparison subjects (χ2=21.42, df=1, p<0.001).
Discussion
This study examined the occurrence of obsessive-compulsive spectrum disorders among first-degree relatives in 136 nuclear families of eating disorder probands in Italy. The DSM-IV distinction between the restricting and the binge-eating types of anorexia nervosa was used, despite our awareness that many patients diagnosed with restricting-type anorexia may later develop binge-eating/purging type anorexia or bulimia (42). The rate of crossover from anorexia to bulimia is reported to range from 10% to 50%.
The higher morbidity risk for obsessive-compulsive spectrum disorders in the first-degree relatives of the patients with eating disorders (10.34%) lends further support to the proposal that obsessive and compulsive symptoms in eating disorder patients should not be considered signs of an additional diagnosis, but rather part of the eating disorder, and that obsessive-compulsive disorder and eating disorders are phenotypic expressions of the same liability.
Eating disorder patients without a comorbid obsessive-compulsive spectrum disorder might develop such a disorder later; although we found no difference in age between the eating disorder probands with and without a comorbid obsessive-compulsive spectrum disorder, even though those with a comorbid diagnosis were slightly older (by 2 years).
The comorbidity of obsessive-compulsive spectrum disorders in eating disorder probands did not influence familial liability for obsessive-compulsive spectrum disorders, despite the significantly greater familial risk for these disorders among the parents of probands with bulimia and anorexia, restricting type, than in the parents of the 109 eating disorder probands without comorbid obsessive-compulsive spectrum disorders. No differences in morbidity risk were found for first-degree relatives of eating disorder probands with and without a comorbid obsessive-compulsive spectrum disorder (data not shown). Unlike our results, the findings of Lilenfeld et al. (19) showed that stratification by proband comorbidity status influenced the adjusted risk ratios for OCD in first-degree relatives. However, even after Lilenfeld et al. adjusted the risk ratios for OCD for the sex, age, and interview status of the relatives in their study, relatives of patients with anorexia nervosa and bulimia had a significantly higher risk for OCD than did the relatives of the comparison subjects. Our finding of an absence of difference in familial risk for eating disorders between the eating disorders group and the comparison group is similar to the finding of Lilenfeld et al. (19) of no increased risk for anorexia nervosa and bulimia in the relatives of patients with eating disorders. From this we can conclude that when eating disorders are considered independently of obsessive-compulsive spectrum disorders, no evidence of a familial risk for eating disorders is found.
Although prevalence studies performed to date have considered anorexia and bulimia as two distinct categories, we found no differences in the morbidity risk for obsessive-compulsive spectrum disorders in comparisons of the eating disorders subgroups, suggesting that relatives of patients with anorexia and those of patients with bulimia share the same liability for obsessive-compulsive spectrum disorders.
Nevertheless, we observed a tendency toward higher morbidity risk for OCD and related disorders in some relatives: sisters of patients with bulimia (morbidity risk=12.13%), sisters of patients with anorexia, binge-eating/purging type (morbidity risk=13.35%), brothers of patients with bulimia (morbidity risk=18.23%), and brothers of patients with anorexia, restricting type (morbidity risk=27.36%). In general, the sisters of the eating disorder probands had a higher morbidity risk for obsessive-compulsive spectrum disorders, whereas the morbidity risk observed in their mothers was comparable to that of their fathers. We observed a higher occurrence of tic disorders in male relatives (fathers and brothers), in accordance with earlier findings that female relatives of OCD probands are affected with OCD and male relatives with tic disorders (43, 44). However, OCD was not associated with a particular subtype of eating disorder in our study, and the overlap in morbidity risk for OCD among eating disorder subgroups provided indirect proof of a link between these disorders.
The main limitation of this study derives from the methods used to collect some clinical information from first-degree relatives. The family history method we used could have influenced the estimated true prevalence of eating disorders and OCD in first-degree relatives. Another problem was the choice of the techniques used to analyze nonindependent data.
The increased familial risk for obsessive-compulsive spectrum disorders in the families of the eating disorder probands suggests the need to further test the hypothesis of a genetic component for this risk. To better define the features of this liability, we have planned a segregation analysis of these family data that will consider eating disorders and OCD as a common phenotype (manuscript in preparation). These findings could enable us to define more accurately the relationship between the psychopathological aspects of eating disorder and OCD diagnoses, to better describe the common structure shared by the two disorders, and to improve treatment for eating disorders and OCD.
 |
 |
Received April 20, 1998; revisions received Aug. 5 and Sept. 1, 1999, and July 7, 2000; accepted Oct. 17, 2000. From the Istituto Scientifico H. San Raffaele, Department of Neuropsychiatric Sciences, University of Milan School of Medicine. Address reprint requests to Dr. Bellodi, Istituto Scientifico H. San Raffaele, Department of Neuropsychiatric Sciences, University of Milan School of Medicine, 29 via Prinetti, 20127 Milan, Italy. The authors thank Dr. Marco Locatelli for comments on this report.
1. Treasure JL, Holland J: Genes and aetiology of eating disorders, in The New Genetics of Mental Illness. Edited by McGuffin P, Murray RM. Woburn, Mass, Butterworth-Heinemann, 1991, pp 198–211Google Scholar
2. Nowlin NS: Anorexia nervosa in twins: case report and review. J Clin Psychiatry 1983; 44:101–105Google Scholar
3. Holland A, Hall A, Murray R, Russel GFM, Crisp AH: Anorexia nervosa: a study of 34 twin pairs and one set of triplets. Br J Psychiatry 1984; 145:414–419Crossref, Medline, Google Scholar
4. Holland AJ, Sicotte N, Treasure J: Anorexia nervosa: evidence for a genetic basis. J Psychosom Res 1988; 32:561–571Crossref, Medline, Google Scholar
5. Fichter MM, Noegel R: Concordance for bulimia nervosa in twins. Int J Eat Disord 1990; 9:255–263Crossref, Google Scholar
6. Hsu LKG, Chesler BE, Santhouse R: Bulimia nervosa in 11 sets of twins: a clinical report. Int J Eat Disord 1990; 9:275–282Crossref, Google Scholar
7. Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L: The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991; 148:1627–1637Google Scholar
8. Theader S: A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl 1970; 214:1–194Medline, Google Scholar
9. Cantwell DP, Sturzenberger S, Burroughs J, Salkin B, Green JK: Anorexia nervosa: an affective disorder? Arch Gen Psychiatry 1977; 34:1087–1093Google Scholar
10. Crisp AH, Hsu LK, Harding B, Harshom J: Clinical features of anorexia nervosa: a study of consecutive series of 102 female patients. J Psychosom Res 1980; 24:179–191Crossref, Medline, Google Scholar
11. Hudson JI, Pope HG Jr, Jonas JM, Yurgelun-Todd D: Family history study of anorexia nervosa and bulimia. Br J Psychiatry 1983; 142:133–138Crossref, Medline, Google Scholar
12. Gershon ES, Schreiber JL, Hamovit JR, Dibble ED, Kaye W, Nurnberger JI Jr, Andersen AE, Ebert M: Clinical findings in patients with anorexia nervosa and affective illness in their relatives. Am J Psychiatry 1984; 141:1419–1422Google Scholar
13. Strober M, Morrell W, Burroughs J, Salkin B, Jacobs C: A controlled family study of anorexia nervosa. J Psychiatr Res 1985; 119:239–246Crossref, Google Scholar
14. Halmi KA, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J: Comorbidity of psychiatric diagnoses in anorexia nervosa. Arch Gen Psychiatry 1991; 48:712–718Crossref, Medline, Google Scholar
15. Woodside D: Anorexia nervosa and bulimia nervosa in children and adolescents. Curr Opin Pediatr 1993; 5:415–418Medline, Google Scholar
16. Strober M, Lambert C, Morrell W, Burroughs J, Jacobs C: A controlled family study of anorexia nervosa: evidence of familial aggregation and lack of shared transmission with affective disorders. Int J Eat Disord 1990; 9:239–253Crossref, Google Scholar
17. Logue CM, Crowe RR, Bean JA: A family study of anorexia and bulimia. Compr Psychiatry 1989; 30:179–188Crossref, Medline, Google Scholar
18. Kassett JA, Gershon ES, Maxwell ME, Guroff JJ, Kazuba DM, Smith AL, Brandt HA, Jimerson DC: Psychiatric disorders in the first-degree relatives of probands with bulimia nervosa. Am J Psychiatry 1989; 146:1468–1471Google Scholar
19. Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C, Rao R, Strober M, Bulik CM, Nagy L: A controlled family study of anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1998; 55:603–610Crossref, Medline, Google Scholar
20. Bulik CM: Anxiety disorders and eating disorders: a review of their relationship. New Zealand J Psychol 1995; 24:51–62Google Scholar
21. Palmer HD, Jones M: Anorexia nervosa as a manifestation of compulsive neurosis. Arch Neurol Psychiatry 1939; 41:856–860Crossref, Google Scholar
22. Du Bois F: Compulsion neurosis with cachexia (anorexia nervosa) Am J Psychiatry 1949; 106:107–115Google Scholar
23. Rothenberg A: Eating disorder as a modern obsessive-compulsive syndrome. Psychiatry 1986; 153:6–15Google Scholar
24. Rothenberg A: Differential diagnosis of anorexia nervosa and depressive illness: a review of 11 studies. Compr Psychiatry 1986; 29:427–432Crossref, Google Scholar
25. Kaye WH, Weltzin T, Hsu LKG: Relationship between anorexia nervosa and obsessive-compulsive behaviors. Psychiatr Annals 1993; 23:365–373Crossref, Google Scholar
26. Solyom L, Freeman RJ, Miles JE: A comparative psychometric study of anorexia nervosa and obsessive neurosis. Can J Psychiatry 1982; 27:282–286Crossref, Medline, Google Scholar
27. Thiel A, Brooks A, Ohlmeier M, Jacoby GE, Schussler G: Obsessive-compulsive disorder among patients with anorexia and bulimia nervosa. Am J Psychiatry 1995; 152:72–75Link, Google Scholar
28. Tovim DI, Marilov V, Crisp AH: Personality and mental state (PSE) within anorexia nervosa. J Psychosom Res 1979; 23:321–325Crossref, Medline, Google Scholar
29. Thornton C, Russell J: Obsessive-compulsive comorbidity in the dieting disorders. Int J Eat Disord 1997; 21:83–87Crossref, Medline, Google Scholar
30. Braun DL, Sunday SR, Halmi KA: Psychiatric comorbidity in patients with eating disorders. Psychol Med 1994; 24:859–867Crossref, Medline, Google Scholar
31. Kasvikis YG, Sakiris F, Marks IM, Basoglu M, Noshirvani H: Past history of anorexia nervosa in women with obsessive-compulsive disorder. Int J Eat Disord 1986; 5:1069–1075Google Scholar
32. Zribi S, Chambon O, Cottraux J: Anorexia nervosa: a frequent antecedent of obsessive-compulsive disorder. Encephale 1989; 15:355–358Medline, Google Scholar
33. Rubenstein CS, Pigott TA, L’Heureux F, Hill JL, Murphy DL: A preliminary investigation of the lifetime prevalence of anorexia and bulimia nervosa in patients with obsessive compulsive disorder. J Clin Psychiatry 1992; 53:309–314Medline, Google Scholar
34. Fahy TA, Osacar A, Marks I: History of eating disorders in female patients with obsessive-compulsive disorder. Int J Eat Disord 1993; 14:439–443Crossref, Medline, Google Scholar
35. Keys A, Brozek J, Heuschel A: The Biology of Human Starvation, vol 1. Minneapolis, University of Minnesota Press, 1950Google Scholar
36. Pauls DL, Leckman JF: The inheritance of Gilles de la Tourette’s syndrome and associated behaviors. N Engl J Med 1986; 315:993–997Crossref, Medline, Google Scholar
37. Kurlan P: Tourette’s syndrome: current concepts. Neurology 1989; 39:1625–1630Google Scholar
38. Santangelo S, Pauls DL, Lavori PW, Goldstein JM, Faraone SV, Tsuang MT: Assessing risk for the Tourette spectrum of disorders among first-degree relatives of probands with Tourette syndrome. Am J Med Genet 1996; 67:107–116Crossref, Medline, Google Scholar
39. Battaglia M, Bernardeschi L, Politi E, Bertella S, Bellodi L: Comorbidity of panic and somatization disorder: a genetic-epidemiological approach. Compr Psychiatry 1995; 36:411–420Crossref, Medline, Google Scholar
40. Robins LN, Helzer JE, Cottler L, Golding E: National Institute of Mental Health Diagnostic Interview Schedule, version III, revised. St. Louis, Washington University, Department of Psychiatry, 1989Google Scholar
41. Dixon WJ (ed): BMDP Statistical Software Manual to Accompany the 7.0 Software Release, vols 1–3. Berkeley, University of California Press, 1992Google Scholar
42. Keel PK, Mitchell JE: Outcome in bulimia nervosa. Am J Psychiatry 1997; 154:313–321Link, Google Scholar
43. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnoses: a methodological study. Arch Gen Psychiatry 1982; 39:879–883Crossref, Medline, Google Scholar
44. Pauls DL, Alsobrook JP II, Goodman W, Rasmussen S, Leckman JF: A family study of obsessive-compulsive disorder. Am J Psychiatry 1995; 152:76–84Link, Google Scholar



