Two-Year Syndromal and Functional Recovery in 219 Cases of First-Episode Major Affective Disorder With Psychotic Features
Abstract
OBJECTIVE: Psychotic affective disorders are the most prevalent idiopathic psychoses, but their outcome from onset has rarely been studied. In this study, the authors determined the rate and latency of syndromal recovery and rates of functional recovery after first lifetime hospitalization in patients with first-episode psychotic affective disorders. METHOD: From first lifetime hospitalization in 1989–1996, 219 patients with a DSM-IV psychotic affective illness were assessed at intervals over 24 months. Time to syndromal recovery (no longer meeting DSM-IV episode criteria) was assessed by survival analysis, and functional recovery (regaining baseline vocational and residential status) was rated. Factors associated with recovery were identified by bivariate and multivariate methods. RESULTS: By 3, 6, 12, and 24 months after first hospitalization, syndromal recovery was attained by 65.1%, 83.7%, 91.1%, and 97.5%, respectively, of subjects. Time to syndromal recovery (6.1 weeks to 50% of subjects recovered) was shorter for patients who had bipolar disorder, were married, were age 30 or older at onset, lacked comorbidity, required relatively brief hospitalization, and received fewer medicines. Functional recovery by 6 (30.4%) and 24 months (37.6% of patients) was 2.6–2.7 times less likely than syndromal recovery; 63.1% of those recovering syndromally did not recover functionally by 2 years. Functional recovery was associated with older age at onset and shorter hospitalization. Annual recovery rates remained stable as mean hospital length of stay decreased 3.6-fold over the 8-year study period. CONCLUSIONS: Syndromal recovery was attained by most psychotic affective disorder patients soon after hospitalization, but only one-third recovered functionally by 24 months. The findings suggest that these very common psychotic illnesses can carry a grave functional prognosis from the initial episode and first hospitalization.
Prediction of course and outcome from the onset of severe and potentially recurring or chronic affective illness with psychosis has major public health importance. Estimated lifetime prevalence of mania and major depression in the United States are, respectively, 1.6% and 14.7% (1). Psychotic features including delusions and hallucinations are common in major affective disorders. About 75% of patients with mania (2) and 14% with major depression (3) have such features. Thus lifetime prevalence of major affective disorders with psychotic features probably exceeds 3% of the general population, making these, by far, the most common idiopathic psychotic disorders.
Some recent studies report poor outcomes in many bipolar disorder patients (2, 4–9). Most of these studies include patients at various stages of illness, but few of the study subjects are experiencing their first illness episode and many have had multiple episodes. Because prior episodes strongly predict future episodes of major affective disorders (10, 11), studies with a high proportion of multiple-episode patients probably overrepresent patients with a relatively poor prognosis. Outcomes in first-episode patients followed prospectively typically are less adverse than those in multiple-episode patients or mixed samples, and treatment is more effective if patients are not already chronically ill (12–14).
Several first-episode studies focusing on patients with affective disorder with psychotic features, using contemporary diagnostic and outcome criteria, have been conducted to validate diagnoses, define illness course and treatment response, and identify predictors of long-term outcome (13, 15–17). However, with one recent exception (17), none has involved more than 100 subjects followed up for longer than 18 months. First-episode studies involving large samples assembled early in psychotic illnesses, with long-term follow-up, are required for robust identification of early predictors of outcome free of the long-term confounding effects of illness, disability, and treatment.
Most outcome studies of bipolar disorder have focused on general clinical outcomes, episode frequency, or clinically determined syndromal recovery rates (4, 5, 8, 18–22). Very few have applied operationally defined measures of recovery based on contemporary diagnostic criteria (9, 10, 17, 23, 24) or distinguished syndromal from functional recovery (9, 17). We found previously that symptomatic recovery was attained by 80% of patients with bipolar disorders by 6 months after initial hospitalization, while only 21% were working at their expected level (25), and that marked disparity between syndromal and functional recovery was sustained at 4-year follow-up (2). Similarly, Strakowski et al. (17) found recently that 56% of patients with psychotic affective disorders achieved syndromal recovery, but only 35% returned to premorbid functional status within a year of first hospitalization.
Since 1989, the McLean First-Episode Project has been following a large number of patients with a first-episode psychotic affective disorder prospectively from their first lifetime hospitalization (23, 25–29). This report is based on 24 months of follow-up, completed between 1991 and 1998, of 219 adults with a DSM-IV bipolar or major depressive disorder with psychotic features. We assessed the rate and latency of syndromal recovery and rates of functional recovery to baseline residential and occupational status and identified descriptors associated with recovery.
METHOD
This prospective naturalistic but structured follow-up study involved inpatients recruited between 1989 and 1996 at McLean Hospital, a teaching hospital of Harvard Medical School. Diagnoses were updated in 1998 to meet DSM-IV criteria. Treatment, although uncontrolled, was monitored throughout the study and was representative of contemporary community standards.
Inclusion criteria were 1) age 15–75 years, 2) a first hospitalization, 3) a first lifetime episode of a major affective disorder with psychotic features including hallucinations, delusions, thought disorder, or grossly disorganized behavior at admission, and 4) meeting the DSM-IV lifetime criteria for primary bipolar disorder or major depressive episode, both with psychotic features. All subjects gave written informed consent, and McLean Hospital Institutional Review Board reviewed and approved the study protocol.
Exclusion criteria were 1) delirium associated with drug or alcohol abuse, 2) a previous psychiatric hospitalization, unless for detoxification, 3) IQ less than 70 or a DSM-IV organic mental disorder, 4) ill for more than 1 year, and 5) previous antipsychotic or mood stabilizer treatment for more than 3 months total. A specialized research assistant identified potential subjects by daily screening of all patients with psychotic symptoms in preadmission and new admission assessments. The research assistant verified identification of prospective subjects in daily reviews with treating psychiatrists.
Baseline Measures
DSM-III-R axis I diagnoses were based on interviews using the Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P) (30) carried out by raters with master’s-level training and more than 5 years of clinical experience. The interviewers maintained high levels of interrater reliability, as described below. Detailed clinical narratives were prepared from all available information (SCID-P, medical records, and interviews with family members and primary clinicians) and presented to two senior research psychiatrists (M.T., C.M.Z.). They applied a best-estimate procedure (31) to determine baseline primary and comorbid diagnoses. DSM-IV diagnoses were ascertained by reapplication of the best-estimate procedure based on all available clinical data accumulated during follow-up, including repeat assessments using the SCID-P at 24 months.
Clinical and demographic variables recorded at initial hospitalization included age, sex, race, education, employment status, and living situation. At discharge, data on duration of initial hospital length of stay and discharge medications were recorded. Assessment of comorbidity considered 1) other current and lifetime DSM-IV axis I disorders, 2) current and lifetime comorbid alcohol or other substance use disorders, and 3) concurrent medical illnesses. The assessment was based on review of medical records and the results of the SCID-P examination and on interviews with patients, relatives, and treating clinicians conducted by research assistants trained to obtain such data reliably. Patients were evaluated within 72 hours of admission and weekly thereafter until discharge.
Primary assessment scales included 1) an expanded, 36-item McLean version of the Brief Psychiatric Rating Scale (BPRS) (32), including 35 individual items and a global score (all rated for severity, 0–7), as well as a total summed score, and subscale scores for psychosis, mania, and depression, all as reported previously (23, 28, 33); 2) the Clinical Global Impression (CGI) (34), rated 1–7; and 3) the Global Assessment of Functioning Scale (30), scored 1–100. Functional outcome was rated for occupational status with the standardized Modified Vocational Status Index, scored 1–7, and for residential status with a Modified Location Code Index, scored 1–9, detailed previously (2, 13, 23, 25, 28). The Modified Vocational Status Index assesses seven occupational levels: 1) full-time gainful employment; 2) homemaker or student; 3) part-time gainful employment (30 hours/week or more); 4) retired; 5) full- or part-time volunteer; 6) on medical or psychiatric leave of absence; and 7) unemployed, whether or not expected to work. The Modified Location Code Index rates 9 levels of living situation: 1) head of household or functional household member, 2) alone or with peer, 3) with family member under minimal supervision, 4) unsupervised boarding home, 5) cooperative apartment, 6) halfway house, 7) with family member under close supervision, 8) open quarter-way house or transitional care unit on hospital grounds, or 9) hospitalized. Baseline occupational and residential status were rated as the highest level achieved 1 year or less before hospitalization, based on information from medical records, family members, and subjects.
Outcome Measures
Systematic reevaluations were conducted at 6-, 12-, and 24-month follow-up after hospital admission by an experienced, master’s-level rater (P.G.-M.) blinded to baseline information. The serial follow-up interviews followed a structured format. Follow-up information was obtained face-to-face or in telephone interviews of subjects, supplemented with information from close relatives or other household members with the patient’s consent, as reported previously (2, 13, 28, 33, 35). Most follow-up assessments (90%) were by telephone. Sixty percent involved the subject only, and 40% also involved relatives and friends, usually (90% of the time) with subject present. In the rare instances when the subject was not present, project interviewers carefully probed for essential information, especially data needed for SCID diagnostic purposes, and asked key questions in multiple formats to provide a means to verify information given by informants.
Information from follow-up interviews included sociodemographic changes, intervening course of primary and comorbid disorders, current occupational and residential status, recent medications and doses, symptomatic status relevant to syndromal recovery, and estimated time to syndromal recovery. The Streamlined Longitudinal Interview Clinical Evaluation (11), which assesses psychosocial status; three measures of functioning, the Global Assessment of Functioning Scale, the Modified Vocational Status Index, and the Modified Location Code Index; and the SCID-P were used in the follow-up interview.
Recovery
Syndromal recovery was defined as no longer meeting criteria for an ongoing DSM-IV illness episode (23, 36, 37), using a conceptualization of recovery proposed by Frank et al. (36). Criteria for syndromal recovery were 1) all DSM-IV mania A severity criteria less than 3 (range=1–7), no B criterion rated greater than 3, and no two B criteria rated 3; 2) no DSM-IV depression criterion rated greater than 3 and no more than three criteria rated 3 and a CGI score of 2 or less; and 3) results sustained for 8 weeks or longer, with latency to syndromal recovery scored as days from hospital admission to the start of the interval of sustained recovery. Functional recovery (yes/no), defined by comparing ratings on the Modified Vocational Status Index (vocational status) and Modified Location Code Index (living situation) at entry versus 6- and 24-month follow-up, required return to at least baseline levels of both measures.
Reliability
Interrater reliability was evaluated for the SCID-P for primary (intraclass correlation coefficient [ICC]=0.92) and secondary (ICC=0.90) diagnoses (2, 13, 23, 28, 33). High interrater reliability was also obtained for the 36-item expanded BPRS (ICC=0.96) (2, 23, 28). Excellent agreement between telephone and in-person interviews was obtained for the outcome assessment (ICC=0.90) (35, 38).
Data Preparation
Each subject was first designated recovered or not recovered by 6 and 24 months, based on the syndromal and functional criteria, and the time to syndromal recovery was recorded. Age at onset was dichotomized (less than 30 versus 30 or older); onset or prodrome type was rated rapid (less than 6 months) or gradual (6 months or longer). Principal DSM-IV diagnoses were 1) bipolar disorder, manic or mixed episode with psychotic features (bipolar depressed and not otherwise specified were not encountered; schizoaffective diagnoses were excluded), or 2) major depressive episode with psychotic features. Because average length of stay diminished yearly, individual length of stay (days) was normalized by binary characterization of hospitalization as short (25th percentile or lower) or long (75th percentile or higher) within each year. Individual BPRS items were rated as nonsevere or severe (ratings of 0–4 versus 5–7); depressive, manic, and psychotic subtotal ratings of the 36-item BPRS scale (28, 33, 35, 38) were similarly dichotomized, and total scores were median-split into high and low subgroups.
Statistical Analyses
Rates of 24-month syndromal and functional recovery were compared for subgroups with contingency tables (chi-square, or Fisher’s exact p for comparisons involving fewer than 10 subjects per group). Rank-based parametric tests compared distributions of continuous variables in subgroups. Factors with suggestive or significant (p<0.10) bivariate associations with recovery status were retained for multivariate analyses. Cox proportional hazards models (for time to syndromal recovery) and multiple logistic regression models (for functional recovery) evaluated candidate explanatory variables for independent association with recovery status. Deciles of fitted values and partial residual plot methods were used to test goodness-of-fit of multivariate models (39). Explanatory variables with adjusted odds ratios (for multiple logistic regression) or hazard ratios (for Cox regression) substantially different from 1.00 (p<0.10) were entered into final regression models. Distributions of days to recovery and computed time to 50% probability of recovery (with 95% confidence interval [CI]) were compared between subgroups of interest by Kaplan-Meier survival analysis. These comparisons were evaluated with Mantel-Cox log-rank (chi-square) tests (40). Robust methods were used in these calculations (41). Continuous data are reported as means. Linear regression (r) or Spearman nonparametric rank methods (rs) were used in computing correlation coefficients. Statistical analyses used commercial microcomputer programs (Stata, Stata Corporation, College Station, Tex.; Statview-V, SAS Institute, Cary, N.C.).
RESULTS
Subject Characteristics
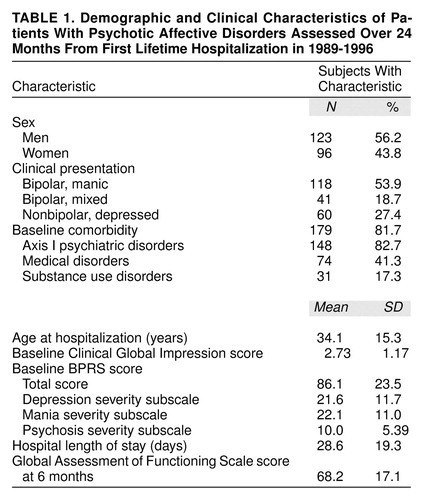
At study entry (1989–1996), 784 patients in first lifetime psychiatric hospitalizations were identified; 334 (42.6%) had psychotic affective illness, and 219 of those patients (65.6%), consisting of 123 men and 96 women, were recruited and retained 6 months or longer. Nonrecruitment or exclusion of the 115 potential subjects (34.4%) reflected failure to meet all inclusion/exclusion criteria for 51 of those patients (44.3%), refusal to participate for 25 (21.7%), inability to complete initial assessments due to short length of stay or administrative reasons for 20 (17.4%), failure to locate at 6 months for 17 (14.8%), or death within 6 months for two (1.8%). Among the 219 recruits, 199 (90.9%) were followed-up for 6–24 months; 18 (8.2%) were lost to follow-up, and two (0.9%) died after 6 months. No significant differences in demographic, clinical, and other descriptive characteristics were found among those followed for 6 months or longer (N=199; 59.6%), lost to follow-up (N=20; 6.0%), and not recruited (N=115; 34.4%; not shown). Diagnoses, based on all information available, included bipolar disorders for 159 of the 219 subjects (72.6%) (118 of whom had bipolar disorder, manic [74.2%] and 41 of whom had bipolar disorder, mixed state [25.8%]) and major depressive disorder for 60 patients (27.4%), all with psychotic features. Of the 219 subjects, 179 (81.7%) had a comorbid axis I psychiatric disorder, substance use disorder, or medical disorder. Patient characteristics are summarized in table 1.
Time to Syndromal Recovery
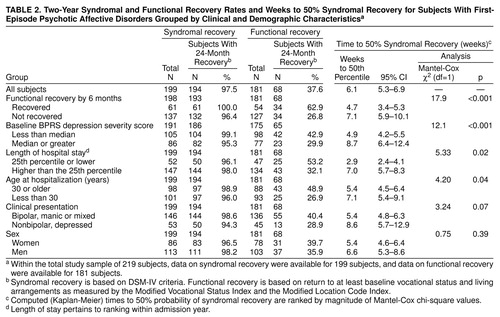
Most of the 199 study patients with syndromal recovery data (N=194; 97.5%) achieved syndromal recovery by 24 months after admission (table 2). Individual time to syndromal recovery averaged 12.6 weeks (SD=16.9, range=0.71–97.1, median=5.90). In survival analyses evaluating time to syndromal recovery, the computed time to 50% probability of recovery for all subjects was 6.1 weeks (95% CI=5.3–6.9). Computed proportions of patients recovering by 3, 6, 12, and 24 months, respectively, were 65.1% (N=142 of 218; 95% CI=58.5%–71.7%), 83.7% (N=170 of 203; 95% CI=79.2%–89.8%), 91.1% (N=184 of 202; 95% CI=87.1%–95.3%), and 97.5% (N=194 of 199; 95% CI=94.9%–99.9%).
Factors associated with time to syndromal recovery were tested by comparing survival functions in subgroups of interest (table 2). Syndromal recovery time was shorter with 1) relatively low initial depression severity, 2) functional recovery by 6 months, 3) age 30 or older at illness onset, and 4) relatively brief hospitalization. Syndromal recovery of 50% of subjects was also 17.5 days shorter in bipolar versus psychotic depression subjects (38.0 versus 55.5 days). Women recovered only slightly earlier than men.
Two-Year Recovery Rates
Although almost all subjects achieved syndromal recovery (97.5% [N=194 of 199] within 24 months or less after hospitalization), only 37.6% (N=68 of 181) achieved functional recovery in that time (table 2). Functional recovery based on residential and occupational status was achieved by only 30.4% (N=62 of 204), 32.5% (N=64 of 197), and 37.6% (N=68 of 181) of subjects at 6, 12, and 24 months, respectively. Among men and women, rates of syndromal (N=111 of 113; 98.3% and N=83 of 86; 96.5%) and functional recovery (N=37 of 103; 35.9% and N=31 of 78; 39.7%) by 2-year follow-up were nearly identical (χ2=0.10, df=1, both n.s.) (table 2). Recovery rates were also very similar among diagnostic subtypes (syndromal versus functional recovery rates, in rank order): 99.1% versus 42.1% for patients presenting with bipolar disorder, manic; 97.4% versus 37.8% for patients with bipolar disorder, mixed (98.6% versus 40.4% for all patients with bipolar disorders); and 94.3% versus 28.9% for nonbipolar, depressed patients (χ2=3.24 and χ2=1.94 for the recovery categories, df=2, both n.s.).
Among the 97.5% (N=194 of 199) of subjects achieving syndromal recovery for whom data on functional recovery were available, 63.1% (N=111 of 176) failed to reach functional recovery by 2 years. Few (N=65 of 176; 36.9%) achieved both types of recovery. Only 1.5% (N=3 of 199) recovered functionally while continuing to meet DSM-IV criteria for an ongoing episode of illness. Functional recovery rates were much lower than syndromal rates at 6 and 24 months (figure 1).
Correlates of Syndromal and Functional Recovery
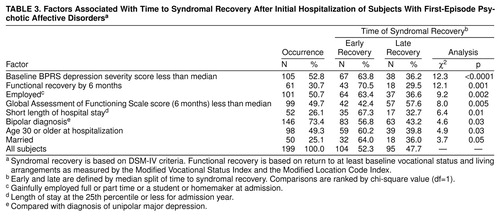
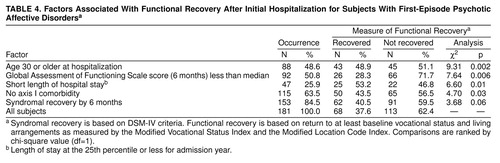
Several clinical descriptors were associated with recovery types in preliminary bivariate analyses (table 3 and table 4). Syndromal recovery was strongly predicted by low initial BPRS depression scores. Only short hospitalization and older age at onset (age 30 or older) were significantly associated with both syndromal and functional recovery. Potential but nonsignificant correlates with recovery included male sex, gradual onset, greater initial illness severity (baseline CGI score), and comorbid psychiatric, substance abuse, or medical illness.
Hospital length of stay declined progressively across study years by 3.63-fold, from a mean of 45.4 days (SD=21.8) in 1989 to 12.5 days (SD=6.16) in 1996 (rs=0.57, p<0.0001, N=219). However, neither individual times to recovery (r=0.01, n.s., N=194) nor computed time to 50% syndromal recovery varied significantly with hospitalization year (r=0.09, n.s., N=194) or the corresponding annual average length of stay (data not shown). Across all subjects, syndromal recovery time increased with longer initial hospitalization (rs=0.32, p<0.0001, N=194), and computed time to 50% recovery was shorter after relatively short hospitalizations (table 2). Hence, as expected, clinically determined shorter hospital length of stay was associated with more favorable early prognosis. Proportions of patients attaining both syndromal and functional recovery within 2 years of initial hospitalization remained quite stable across years of study entry despite marked, progressive shortening in length of stay (figure 2).
Multivariate Analyses of Factors Associated With Recovery
Multivariate regression modeling examined the relative strength of association with recovery outcomes of the factors identified in bivariate analyses to be preliminarily associated with time to syndromal recovery (table 3) or attainment of functional recovery (table 4). Cox multivariate regression analysis (table 5) associated four factors with time to syndromal recovery in a highly significant model (χ2=30.7, df=4, p<0.001). The factors, in rank order by odds ratio, were 1) relatively low initial depression severity, 2) functional recovery by 6 months, 3) relatively short length of stay, and 4) age 30 years or older at onset. Multivariate logistic regression (table 5) associated two factors with functional recovery in a highly significant model (χ2=14.6, df=2, p<0.001). The two factors, in rank order of hazard ratio, were age 30 years or older at onset and relatively short length of stay.
Pharmacological Treatment
Psychotropic agents were taken by 95% of patients with bipolar disorders (N=151 of 159 patients) and 92% of patients with major depressive disorder (N=55 of 60 patients) at hospital discharge, and by 51% (N=74 of 146) and 42% (N=22 of 53), respectively, at 2-year follow-up. Among the 159 psychotic bipolar patients, predictably, mood-stabilizing agents were the most commonly prescribed agents at discharge (N=142; 89% of cases), including lithium (N=114; 72%) or an anticonvulsant (N=38; 24%); 81% (N=129) received an antipsychotic; and 10% (N=16) an antidepressant. All of those who received an antipsychotic also received a mood stabilizer. By 2-year follow-up, 51% (N=74 of 146) received mood stabilizers; 19% (N=28), antidepressants; 16% (N=23), antipsychotics; and 14% (N=20), anxiolytic-sedatives. Several patients received two or more drugs, usually a mood stabilizer and an antipsychotic (N=23 of 146; 16%), a mood stabilizer and an antidepressant (N=22 of 146; 15%), or two mood stabilizers (N=20 of 146; 14%).
Most of the 60 depressive subjects were discharged with an antidepressant (N=42; 70%) or antipsychotic (N=43; 72%), and 22% (N=13) received a mood stabilizer. By 2-year follow-up, 36% (N=19 of 53) received antidepressants; 25% (N=13), antipsychotics; 13% (N=7), anxiolytic-sedatives; and 4% (N=2), mood stabilizers. At 24 months, 11% (N=6 of 53) received more than one drug, usually an antidepressant with an antipsychotic (N=5; 9%).
Time to syndromal recovery and functional recovery by 2 years were not associated with drug treatment types at discharge or 2-year follow-up, nor with lack of medication at follow-up, in either bipolar or depressive patients. However, functionally recovered patients tended to receive fewer medicines (mean=3.15, SD=2.41 versus mean=3.94, SD=2.8) (F=3.2, df=1, 178, p=0.05). The average number of medicines taken at 2 years was greater in subjects requiring longer time to syndromal recovery (rs=0.18, p=0.02, N=194). Moreover, multiple-drug treatment at 2 years was associated with longer time to syndromal recovery: taking one, two to four, or five or more psychotropics was associated, respectively, with 50% recovery times of 6.66 weeks (95% CI=0–16.6), 14.5 weeks (95% CI=0–58.6), and 30.5 weeks (95% CI=0–80.1) (χ2=7.01, df=2, p=0.03). However, recovery time was significantly longer with more intensive polypharmacy in depressive patients (χ2=9.47, df=2, p=0.009) but not in bipolar patients (χ2=4.20, df=2, p=0.12).
DISCUSSION
Major affective syndromes with psychotic features, although the most common idiopathic psychotic disorders, have rarely been studied in prolonged, systematic follow-up to clarify their course and outcome, and very rarely has a large sample of such patients been followed from illness onset. This report involves 219 patients with bipolar (72.6%) or major depressive (27.4%) syndromes presenting initially with psychotic features and given standard contemporary treatment, with follow-up at regular intervals for up to 2 years from a first lifetime psychiatric hospitalization. Limitations of the study include the lack of control of treatment, which may not have been optimal but reflected current community standards. In addition, not all subjects were available for face-to-face examinations at all follow-up times, and 20 were lost to follow-up or died before 24 months. Hospitalization-based sampling may also limit generalizability by omitting persons with illnesses not considered sufficiently severe or dangerous to require hospitalization. Despite these limitations, several interesting findings emerged.
First, proportions of subjects attaining syndromal recovery from the presenting illness episode at 3, 6, 12, and 24 months after first lifetime psychiatric hospitalization were 65.1%, 83.7%, 91.1%, and 97.5%, respectively. Recovery was similarly high in all diagnostic subtypes. These high rates are consistent with the 74% rate of syndromal recovery at 6 months previously reported for 102 subjects with first episodes of affective and nonaffective psychotic disorders at McLean Hospital (23) and with results of two other recent studies (in Cincinnati and Vancouver) reporting 12-month follow-up of first episode psychotic affective disorder patients (17, 42).
A second important finding was a remarkably low probability of functional recovery within 2 years, in contrast with the nearly universal syndromal recovery. By 6, 12, and 24 months of follow-up, only 30.4%, 32.5%, and 37.6% of subjects, respectively, attained living situations and occupational levels even equaling their premorbid levels. A similarly low rate of functional recovery (35% at 12 months) was recently found in the Cincinnati study (17), but comparable data were not reported for the Vancouver sample (42). Evidently, even supposedly “good prognosis” major affective disorders carry a high risk of long-term disability when psychotic features are present and hospitalization is required at illness onset. Moreover, when functional recovery was not achieved early, it was rarely attained later; only 2.94% of subjects (N=6 of 204) not functionally recovered at 6 months attained such recovery by 24 months.
Third, syndromal and functional recovery rates did not change substantially during the study, even as the average hospital length of stay dropped sharply and continuously, by 72.5%, from 45.4 days in 1989 to 12.5 days in 1996 figure 2). Neither time to syndromal recovery nor the proportion of patients achieving functional recovery by 2-year follow-up differed significantly across this era. Apparently, shorter length of stay had neither an unfavorable nor a favorable effect on time to syndromal recovery or chances of functional recovery for most patients. It seems unlikely that shorter inpatient stays reflect major improvements in psychiatric therapeutics in recent years. More plausibly, patients probably continue to recover after hospitalizations shortened by largely economic considerations. Increasingly, recovery occurs in alternative settings, including partial hospital, transitional care, or other ambulatory programs, or even at home. These less intensive settings aim to protect recovering psychotic patients and facilitate syndromal recovery and clinical stability while avoiding expensive hospitalization. However, the short- and long-term clinical impact and the financial and social costs of increased reliance on such alternatives to hospitalization have not been examined empirically. These are important issues urgently requiring scientific investigation.
Some prudent conclusions are suggested by this study. Most patients presenting for the first time with a psychotic affective illness required several months even to recover to the point of no longer meeting DSM-IV diagnostic criteria for a current episode. The great majority remained functionally impaired for at least 2 years from illness onset, and full symptomatic and functional recovery may not occur for some patients. Substantial difficulties with independent living, interpersonal relations, and ability to work productively may continue for prolonged periods or result in sustained disability with high indirect costs to society. The low rates of functional recovery found within 2-year follow-up suggest that functional as well as symptomatic assessments should be included in comprehensive evaluations of even newly psychotic patients and that treatment programs should be designed accordingly. Slowly progressing or poorer prognosis patients with psychotic affective illnesses are likely to require more intensive or structured aftercare, early consideration of innovative and improved medicines, or strengthened psychosocial and rehabilitative interventions aimed at modifying specific disabilities. Since very few patients reached functional recovery after the first 6 months of follow-up, the need for such interventions evidently should be identified early in the recovery process, and required resources allocated appropriately and promptly.
The findings strongly suggest that timely identification and vigorous and sustained therapeutic interventions are required even in supposedly “good prognosis” patients with major affective disorders who present with psychotic features and require early hospitalization. Early risk for substantial disability in the reported sample was surprisingly high. This finding encourages further evaluation of psychotic patients with affective disorder in broader samples including nonhospitalized patients. Effects of markedly shortened hospitalization on long-term syndromal and functional outcomes of patients with psychotic affective disorders, as well as on the process of recovery in the initial months after hospital discharge, also need to be evaluated. Finally, responsiveness of early functional disability in psychotic affective disorders to specific therapeutic interventions and their cost/benefit relationships remain to be evaluated.
Received Feb. 12, 1999; revision received July 15, 1999; accepted Sept. 2, 1999. From the International Consortium for Bipolar Disorder Research and the Harvard–McLean First Psychosis Project; Consolidated Department of Psychiatry and Neuroscience Program, Harvard Medical School; Department of Epidemiology, Harvard School of Public Health, Boston; and the Bipolar and Psychotic Disorders Program, McLean Hospital, Belmont, Mass. Address reprint requests to Dr. Tohen, Lilly Research Laboratories, Indianapolis, IN 46285; [email protected] (e-mail). Supported by NIH grants MH-01948, MH-04844, MH-47370; awards from the National Alliance for Research on Schizophrenia and Depression, the Atlas Foundation, and the Bruce J. Anderson Foundation; the McLean Private Donors Neuropsychopharmacology Research Fund; the Ruane Family Fund; and the Andrew P. Merrill Memorial Fund. Ms. Hari Mandir Kaur Khalsa provided valuable assistance with data analysis.
 |
 |
 |
 |
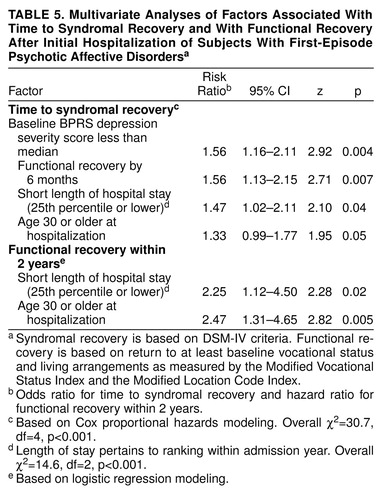 |
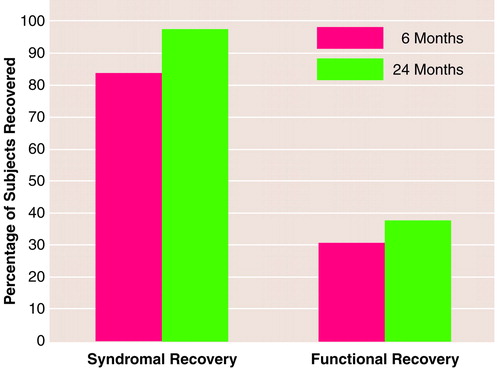
FIGURE 1. Percentage of Patients With First-Episode Psychotic Affective Disorders Who Reached Syndromal (N=199) and Functional (N=181) Recovery Within 6 and 24 Months After First Lifetime Hospitalization
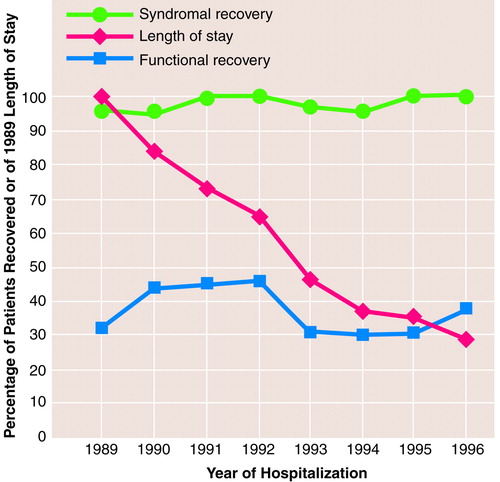
FIGURE 2. Relation of Mean Length of Hospital Stay in 1989-1996 to Rates of Syndromal (N=199) and Functional (N=181) Recovery Within 24 Months After First Lifetime Hospitalization for Patients With Psychotic Affective Disordersa
aCurve for length of stay represents percentage of the 1989 mean of 45.4 days. Decrease in length of stay is highly significant (rs=–0.59, p<0.001), but rates of syndromal and functional recovery are uncorrelated with admission year (rs≤0.06, both n.s.).
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
2. Tohen M, Waternaux CM, Tsuang MT: Outcome in mania: a 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry 1990; 47:1106–1111Google Scholar
3. Johnson J, Horwath E, Weissman MM: The validity of major depression with psychotic features based on a community study. Arch Gen Psychiatry 1991; 48:1075–1081Google Scholar
4. Harrow M, Goldberg JF, Grossman LS, Meltzer HY: Outcome in manic disorders: a naturalistic follow-up study. Arch Gen Psychiatry 1990; 47:665–671Crossref, Medline, Google Scholar
5. Coryell W, Endicott J, Keller M: Outcome of patients with chronic affective disorder: a five-year follow-up. Am J Psychiatry 1990; 147:1627–1633Google Scholar
6. Coryell W, Endicott J, Maser JD, Mueller T, Lavori P, Keller M: The likelihood of recurrence in bipolar affective disorder: the importance of episode recency. J Affect Disord 1995; 33:201–206Crossref, Medline, Google Scholar
7. Gitlin MJ, Swendsen J, Heller TL, Hammen C: Relapse and impairment in bipolar disorder. Am J Psychiatry 1995; 152:1635–1640Google Scholar
8. Goldberg JF, Harrow M, Grossman LS: Course and outcome in bipolar affective disorder: a longitudinal follow-up study. Am J Psychiatry 1995; 152:379–384Link, Google Scholar
9. Keck PE Jr, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, Bourne ML, Haggard P:12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry 1998; 155:646–652Google Scholar
10. Keller MB, Lavori PW, Coryell W, Andreasen NC, Endicott J, Clayton PJ, Klerman GL, Hirschfeld RM: Differential outcome of pure manic, mixed/cycling, and pure depressive episodes in patients with bipolar illness. JAMA 1986; 255:3138–3142Google Scholar
11. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Crossref, Medline, Google Scholar
12. Lundquist G: Prognosis and course in manic-depressive psychoses: a follow-up study of 319 first admissions. Acta Psychiatr Neurol Scand 1945; 20(suppl 35):1–96Google Scholar
13. Tohen M, Waternaux CM, Tsuang MT, Hunt AT: Four-year follow-up of twenty-four first-episode manic patients. J Affect Disord 1990; 19:79–86Crossref, Medline, Google Scholar
14. Baldessarini RJ, Tondo L: Thirty years of lithium treatment. Arch Gen Psychiatry (in press)Google Scholar
15. Husted JA, Beiser M, Iacono WG: Negative symptoms in the course of first-episode affective psychosis. Psychiatry Res 1995; 56:145–154Crossref, Medline, Google Scholar
16. Fennig S, Bromet EJ, Karant MT, Ram R, Jandorf L: Mood-congruent versus mood-incongruent psychotic symptoms in first-admission patients with affective disorder. J Affect Disord 1996; 37:23–29Crossref, Medline, Google Scholar
17. Strakowski SM, Keck PE Jr, McElroy SL, West SA, Sax KW, Hawkins JM, Kmetz GF, Upadhyaha VH, Tugrul KC, Bourne ML: Twelve-month outcome following a first hospitalization for affective psychosis. Arch Gen Psychiatry 1998; 55:49–55Crossref, Medline, Google Scholar
18. Tsuang MT, Woolson RF, Winokur G, Crowe RR: Stability of psychiatric diagnosis: schizophrenia and affective disorders followed up over a 30- to 40-year period. Arch Gen Psychiatry 1981; 38:535–539Crossref, Medline, Google Scholar
19. Black DW, Winokur G, Bell S, Nasrallah A, Hulbert J: Complicated mania: comorbidity and immediate outcome in the treatment of mania. Arch Gen Psychiatry 1988; 45:232–236Crossref, Medline, Google Scholar
20. Winokur G, Kadrmas A: A polyepisodic course in bipolar illness: possible clinical relationships. Compr Psychiatry 1989; 30:121–127Crossref, Medline, Google Scholar
21. Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL: The enduring psychosocial consequences of mania and depression. Am J Psychiatry 1993; 150:720–727Link, Google Scholar
22. Winokur G, Coryell W, Akiskal HS, Endicott J, Keller M, Mueller T: Manic-depressive (bipolar) disorder: the course in light of a prospective ten-year follow-up of 131 patients. Acta Psychiatr Scand 1994; 89:102–110Crossref, Medline, Google Scholar
23. Tohen M, Stoll AL, Strakowski SM, Faedda GL, Mayer PV, Goodwin DC, Kolbrener ML, Madigan AM: The McLean First-Episode Psychosis Project: six-month recovery and recurrence outcome. Schizophr Bull 1992; 18:273–282Crossref, Medline, Google Scholar
24. Tohen M, Goodwin FK: Epidemiology of bipolar disorder, in Textbook in Psychiatric Epidemiology. Edited by Tsuang MT, Tohen M, Zahner M. New York, John Wiley & Sons, 1995, pp 301–315Google Scholar
25. Dion GL, Tohen M, Anthony WA, Waternaux CS: Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hosp Community Psychiatry 1988; 39:652–657Abstract, Google Scholar
26. Strakowski SM, Tohen M, Stoll AL, Faedda GL, Goodwin DC: Comorbidity in mania at first hospitalization. Am J Psychiatry 1992; 149:554–556Link, Google Scholar
27. Strakowski SM, Tohen M, Stoll AL, Faedda GL, Mayer PV, Kolbrener ML, Goodwin DC: Comorbidity in psychosis at first hospitalization. Am J Psychiatry 1993; 150:752–757Link, Google Scholar
28. Tohen M, Zarate CA Jr, Zarate SB, Gebre-Medhin P, Pike S: The McLean/Harvard first-episode mania project: pharmacologic treatment and outcome. Psychiatr Annals 1996; 26(July suppl):S444–S448Google Scholar
29. Zarate CA, Tohen M, Zarate SB: Thyroid function tests in first-episode bipolar disorder manic and mixed types. Biol Psychiatry 1997; 42:302–304Crossref, Medline, Google Scholar
30. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1988Google Scholar
31. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982; 39:879–883Crossref, Medline, Google Scholar
32. Lukoff D, Neuchterlein KH, Ventura J: Manual for the expanded Brief Psychiatric Rating Scale. Schizophr Bull 1986; 12:594–602Google Scholar
33. Tohen M: Course and treatment outcome in patients with mania, in Psychiatric Treatment Advances in Outcome Research. Edited by Mirin SM, Gossett JT, Grob MT. Washington, DC, American Psychiatric Press, 1991, pp 127–142Google Scholar
34. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 218–222Google Scholar
35. Revicki DA, Tohen M, Gyulai L, Thompson C, Pike S, Davis-Vogel A, Zarate C: Telephone versus in-person clinical and health status assessment interviews in patients with bipolar disorder. Harv Rev Psychiatry 1997; 5:75–81Crossref, Medline, Google Scholar
36. Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM: Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Arch Gen Psychiatry 1991; 48:851–855Crossref, Medline, Google Scholar
37. Prien RF, Carpenter LL, Kupfer DJ: The definition and operational criteria for treatment outcome of depressive disorder: a review of the current research literature. Arch Gen Psychiatry 1991; 48:796–800Crossref, Medline, Google Scholar
38. Zarate CA Jr, Weinstock L, Cukor P, Morabito C, Leahy L, Burns C, Baer L: Applicability of telemedicine for assessing patients with schizophrenia: acceptance and reliability. J Clin Psychiatry 1997; 58:22–25Crossref, Medline, Google Scholar
39. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, John Wiley & Sons, 1989Google Scholar
40. Lee ET: Statistical Methods for Survival Analysis. New York, John Wiley & Sons, 1992Google Scholar
41. Lin DY, Wei LJ: The robust inference for the Cox proportional hazards model. J Am Statistical Assoc 1989; 84:1074–1078Google Scholar
42. Iacono WG, Beiser M: Age of onset, temporal stability, and eighteen-month course of first-episode psychoses, in The Emergence of a New Discipline: Rochester Symposium on Developmental Psychopathology, vol 1. Edited by Cicchetti D. Hillsdale, NJ, Lawrence Erlbaum Associates, 1989, pp 221–260Google Scholar



