In This Issue
Pediatric Depression Treatment Declines After FDA Advisory on Antidepressants
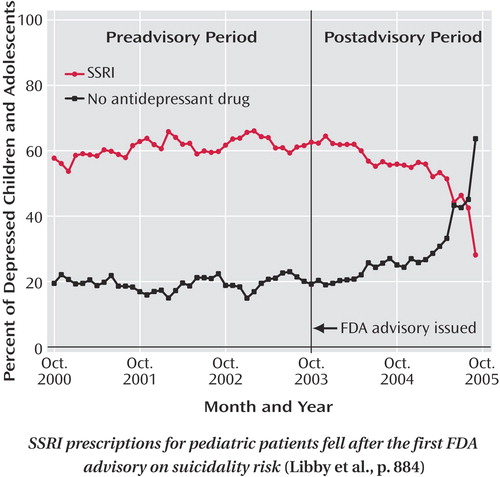
Diagnoses of new cases of major depression in children and adolescents, and their antidepressant treatment, declined sharply over the 2 years following the first Food and Drug Administration (FDA) advisory about suicidality risk for pediatric patients taking selective serotonin reuptake inhibitors (SSRIs). Decreases in SSRIs and non-SSRI antidepressants for depressed patients ages 5–18 are shown by claims in a national database of managed health care plans analyzed by Libby et al. (p. Original article: 884 ). Psychotherapy did not increase after the advisory. This comparison of the 5 years before the FDA advisory in October 2003 with the 2 years afterward encompassed more than 65,000 children and adolescents with a new diagnosis of major depressive disorder. In addition, population-level depression rates fell in 2005 after steadily increasing. Dr. Cynthia Pfeffer comments on these trends in an editorial on p. Original article: 843 .
Social and Genetic Factors in Alzheimer’s Disease
Experience with adult day care may reduce the rate of cognitive decline for people with Alzheimer’s disease who later move to nursing homes. Of 432 older Alzheimer’s disease patients evaluated by Wilson et al. (p. Original article: 910 ), 36% were placed in nursing homes over the next 3–4 years. This transition was followed by an abrupt drop in cognitive functioning, but the subsequent rate of decline was slower for those who had previously used day care services. Patients with more education had greater cognitive declines after moving to nursing homes, but prior day care attenuated this association. A possible biological marker of cognitive decline was identified by Chen et al. (p. Original article: 916 ). They found a correlation between an individual’s “dose” of the apolipoprotein E (APOE) ε4 allele, a risk factor for Alzheimer’s disease, and the rate of brain atrophy during middle age. Magnetic resonance brain images were acquired for cognitively normal people at age 47–68 years and again 2 years later. The rate of whole brain atrophy was highest for people with two ε4 alleles and lowest for those with none. Dr. James Becker et al. discuss the roles of genes and environment in an editorial on p. Original article: 849 .
Mechanisms of Change in Psychotherapy
In patients with borderline personality disorder, 10 of 12 symptom domains improved after 1 year of psychodynamic therapy focusing on transference, the patient’s transfer of feelings or conflicts to the therapist. In the comparison of interventions by Clarkin et al. (CME, p. Original article: 922 ), supportive treatment and behavior therapy were followed by improvements in six and five symptom domains, respectively. Transference-focused psychotherapy was associated with decreases in both suicidality and anger, whereas each of the other treatments decreased only one or the other. The relationship between treatment results and the therapist’s focus on emotion in short-term psychodynamic psychotherapy was explored in a meta-analysis by Diener et al. (p. Original article: 936 ). They identified 10 adequately designed studies that examined therapist activities facilitating the experience or expression of emotion by patients with a variety of diagnoses or problems. Emotional facilitation by the therapist was associated with a 30% greater likelihood of improvement, compared with other psychotherapy. Thus, this finding may help answer the question “What makes psychotherapy work? ” An editorial on these articles by Dr. Glen Gabbard appears on p. 853.
Course of Borderline Personality Disorder
A 10-year study by Zanarini et al. (p. Original article: 929 ) supports the emerging consensus that borderline personality disorder is a treatable condition with a relatively good prognosis. Among 290 hospitalized patients with borderline personality disorder, half of the assessed symptoms resolved over time and the other half showed marked improvement. The latter symptoms primarily involved aspects of temperament, e.g., chronic dysphoria, abandonment fears, or dependency. Targeting these temperamental symptoms might improve outcomes further.



