Twelve-Month Outcome of Adolescents With Bipolar Disorder Following First Hospitalization for a Manic or Mixed Episode
Abstract
Objective: Although adolescent-onset bipolar disorder is associated with significant morbidity, there have been few prospective outcome studies of this population. The aim of this study was to examine the 12-month outcome of bipolar adolescents following an initial hospitalization for a manic or mixed episode. Method: Bipolar adolescents (N=71) were recruited during their first hospitalization for a manic or mixed episode and were evaluated using diagnostic, symptomatic, and functional assessments. Patients were also evaluated at 1, 4, 8, and 12 months after hospitalization to assess syndromic, symptomatic, and functional outcomes. Predictors of each type of outcome were identified. Results: Kaplan-Meier estimates of the cumulative probabilities of syndromal, symptomatic, and functional recovery and syndromic recurrence during the first 12 months following initial hospitalization were 0.86, 0.43, 0.41, and 0.54, respectively. Only 35% of bipolar adolescents reported full medication adherence. Individual predictors of poor syndromic recovery included co-occurring attention deficit hyperactivity disorder (ADHD), anxiety disorders, and disruptive behavior disorders as well as nonadherence to psychotropic medication and lower socioeconomic levels. Co-occurring alcohol use disorders, treatment with antidepressants, and the absence of psychotherapeutic intervention predicted syndromic recurrence. Boys were more than twice as likely as girls to experience symptomatic recovery. Conclusions: Most bipolar adolescents experienced syndromic recovery following their first hospitalization. However, rates of symptomatic and functional recoveries were much lower. Future studies examining effective pharmacological and nonpharmacological treatment strategies for bipolar youth with co-occurring disorders and investigating factors that contribute to the development of substance use disorders and treatment adherence in bipolar youth are necessary to improve outcome.
Although the onset of bipolar disorder most commonly occurs during adolescence (1 , 2) , there have been relatively few naturalistic outcome studies of children and adolescents with bipolar disorder (3 – 11) . Prospective studies of clinical cohorts of bipolar youth have reported recovery and recurrence rates that range from 14%–100% and 35%–70%, respectively, during follow-up periods of 6 months to 4 years. In general, studies of longer duration, older adolescents, and outpatient cohorts report higher recovery rates compared with those of shorter duration, prepubescent and early adolescent subjects, and inpatient cohorts.
Outcome studies of bipolar youth have not identified consistent predictors of recovery or recurrence. Some studies report that longer index affective episode (3 , 11) , index depressive or mixed episodes (11) , rapid-cycling (11) , psychosis (3 – 7) , low maternal warmth (4 – 7) , non-intact biological family (4 – 7) , and low socioeconomic status (3) are associated with poor outcome.
Methodological limitations of and differences among prior studies may have contributed to the failure to identify consistent rates of recovery and recurrence and predictors of outcome. First, previous studies have not reported information regarding medication adherence, despite the strong association between treatment adherence and high recovery rates in studies of bipolar adults (12) . Second, although most outcome studies of bipolar youth include a subset of adolescents close to their illness onset (3 – 11) , no study, to our knowledge, has examined the outcome exclusively of adolescents hospitalized for their first manic episode. Studying patients early in their illness course permits identification of factors associated with recovery that may be difficult to detect in patients who have had multiple affective episodes, where illness chronicity may become the most significant predictor of outcome (3 , 12 , 13) . Finally, prior investigations of bipolar youth have not distinguished among syndromic, symptomatic, and functional outcomes, an important step in clarifying unique factors that differentially contribute to specific aspects of recovery (12) . In fact, to our knowledge there has been only one cross-sectional study to examine functional impairment in bipolar youth (14) .
With these considerations in mind, the aim of this study was to investigate the 12-month outcome of bipolar adolescents following their initial hospitalization for a manic or mixed episode. Specifically, we examined rates of syndromic, symptomatic, and functional recoveries as well as syndromic recurrence. As a secondary aim of this study we examined whether there are distinct predictors of syndromic, symptomatic, and functional outcomes. Based on prior studies (3 – 7 , 11 , 12 , 15 , 16) , we hypothesized that psychosis, socioeconomic status, poor medication adherence, and co-occurring substance use disorders would predict worse outcome in first-hospitalization bipolar adolescents.
Method
Subjects
Adolescents admitted for their first hospitalization for bipolar disorder, type I, manic or mixed (N=71) were recruited from consecutive inpatient admissions between July 1, 1999 to Dec. 1, 2003. Potential subjects were identified by research staff who reviewed the medical records of all new admissions to the Psychiatric Units of Cincinnati Children’s Hospital Medical Center during the study period. Patients were included in the study if they were 12–18 years old, met DSM-IV criteria for a current manic or mixed episode, and had no prior treatment with anticonvulsants, antidepressants, or antipsychotics. Patients with prior psychostimulant treatment were included, since many participants had been treated for presumed preexisting attention deficit hyperactivity disorder (ADHD). Potential subjects were excluded by a diagnosis of mental retardation (IQ<70) or a manic or mixed episode resulting entirely from an unstable medical or neurological disorder or acute intoxication or withdrawal from drugs or alcohol, as determined by symptom resolution within 72 hours. Adolescents provided written assent, and their legal guardians provided written informed consent after study procedures were fully explained. This study was approved by the University of Cincinnati and the Cincinnati Children’s Hospital Medical Center Institutional Review Boards. The study cohort included all first-hospitalization manic or mixed adolescents who met other study criteria.
Index Assessments
Diagnoses were established using the Washington University at St. Louis Kiddie-Schedule for Affective Disorders and Schizophrenia (17) administered by trained child and adolescent psychiatrists with good diagnostic reliability (overall diagnostic reliability on 10 interviews between two raters: kappa=0.94). Adolescents and their primary caregivers were interviewed separately, and responses were combined in order to determine diagnoses (18) . Only adolescents who met DSM-IV criteria for a “distinct period” lasting at least 1 week (or any duration if hospitalization was necessary) for a manic (or mixed) episode were included in this study. The Young Mania Rating Scale (YMRS) (19 , 20) , the 17-item Hamilton Depression Rating Scale (HAM-D) (21 , 22) , and the Scale for the Assessment of Positive Symptoms (SAPS) (23) were performed at the time of index hospitalization by trained psychiatrists (intraclass correlation coefficient >0.8 for all ratings scales) (15) . Demographic information was obtained by interviewing the adolescent and their legal guardian. Socioeconomic status was ascertained using the 4-factor Hollingshead Scale (24) .
Premorbid psychosocial function (highest level during the year prior to index hospitalization) was assessed using the functional rating scales of the Longitudinal Interval Follow-up Examination (LIFE) (25 , 26) . Trained raters with good interrater reliability (kappa>0.75) evaluated four major areas of functioning: role performance, interpersonal relationships, recreational enjoyment, and sexual activity.
Outcome Assessments
Patients were reassessed at 1, 4, 8, and 12 months following discharge from the hospital. The outcome assessments have been described elsewhere (13 , 25–28) and are based on the National Institute of Mental Health (NIMH) Multisite Collaborative Study (29) . At each follow-up visit, the investigators reviewed affective symptoms during the prior interval, week-by-week, with the adolescent and their primary caregivers. Particular attention was given to periods of changing affective symptoms, using the methodology of the LIFE. Each follow-up interview included every item of the symptom ratings scales (YMRS, HAM-D, SAPS) at each week. For each week, an overall rating of symptom severity was made based on the scores of the rating and diagnostic instruments using a 1- to 6-point scale (kappa=0.92): 6=full syndrome, severe, meets several DSM-IV criteria more than the minimum required for an affective episode (manic, hypomanic, mixed or major depressive episode); 5=full syndrome, mild to moderate, meets minimal DSM-IV criteria required for an affective episode; 4=marked symptoms, does not meet full affective syndrome criteria, but has several DSM-IV affective syndrome criteria scored greater than mild on the HAM-D or YMRS; 3=partial remission, no DSM-IV affective syndrome criteria are rated greater than mild on the HAM-D or YMRS, but total HAM-D score >10, YMRS score >5, or any SAPS global item score >2; 2=residual symptoms, one or more mild symptoms, but YMRS score ≤5 and HAM-D score ≤10, and SAPS global item scores are all ≤2; 1=usual self, no significant symptoms.
From these ratings, syndromic and symptomatic recovery and syndromic recurrence were identified, and the percent of weeks without symptoms (1 or 2), with subsyndromal symptoms (3 or 4), and with a full syndrome (5 or 6) were calculated. Syndromic and symptomatic recoveries were defined a priori by 8 weeks with a LIFE overall score of ≤4 and by 8 weeks with a LIFE overall score of ≤2, respectively. Syndromic recurrence was defined by 1 week (2 weeks for depression) with a LIFE overall score of ≥5 any time after syndromic recovery (12 , 13 , 27) . Functional recovery was defined based on prior studies by achieving a rating equal to or better than premorbid psychosocial functioning in all four of the areas of functioning on the LIFE for at least 8 contiguous weeks (26) . To assess functional recovery, at each follow-up visit the four major areas of function (role performance, interpersonal relationships, recreational enjoyment, and sexual activity) were rated for each 4-week period. Time to each type of recovery included the 8 consecutive weeks that the patient met criteria for that type of recovery.
Treatment Assessments
This study was naturalistic and therefore the investigators were not involved in treatment decisions for the adolescents. Medications that were prescribed during each follow-up period were reviewed with the adolescents and their primary caregivers. Medical records from treating clinicians were also obtained as necessary. Treatment adherence for each medication during each interval period was assessed by reviewing weekly medication use with the adolescent and separately with their primary caregiver. Adherence for each medication was characterized as full adherence (the medication was taken >75% of the time as prescribed), nonadherence (the medication was taken <25% of the time as prescribed), or partial adherence (the medication was taken between 25% and 75% of the time as prescribed). The percent of follow-up in which each patient exhibited each category of adherence was determined for each prescribed psychotropic medication, and an average score across medications was used for analyses (12) . Medications were categorized into mood stabilizers, antipsychotics, antidepressants, or psychostimulants.
Statistical Analysis
Statistical analyses were performed using the SAS, version 8.02 (SAS Institute, Cary, North Carolina, 2003). The cumulative probabilities of syndromal, symptomatic, and functional recovery, as well as syndromic recurrence during the 12-months following initial hospitalization were estimated using the Kaplan-Meier method (30) . Based on existing literature, the individual effect of each a priori determined potential predictor on each outcome event (syndromic, symptomatic, and functional recoveries and syndromic recurrence) and time to each outcome event from index hospitalization (time to syndromic recurrence was calculated from syndromic recovery) were evaluated using Kaplan-Meier estimates and Cox proportional hazards modeling (31) , respectively. Additionally, using Cox proportional hazards modeling, predictors were entered by stepwise selection if associated with the event at a significance level of p<0.10.
Sex, ethnicity, socioeconomic status, baseline alcohol and cannabis use disorders, affective state (manic versus mixed), and psychosis, as well as co-occurring ADHD, conduct disorder, oppositional defiant disorder, anxiety disorders, and any psychotherapeutic intervention prior to the outcome event were assessed as predictors of each of the four outcome variables. The results of all analyses were unchanged by combining oppositional defiant disorder or conduct disorder into one predictor variable called disruptive behavior disorders. All independent variables were examined to ensure that they met the proportional hazards assumption, and none exhibited statistically significant deviation from this assumption. Adjusted hazard ratios and their 95% confidence intervals (CIs) were calculated for each predictor for each outcome variable.
Propensity analyses (32) were used to examine the relationships among treatment with specific medication categories and each outcome measure. Only medications that were prescribed between syndromic recovery and syndromic recurrence were included in analyses predicting syndromic recurrence. Each of the previously described predictor variables was examined as candidate explanatory variables for treatment with each medication category. Additionally, duration of mood episode prior to the index hospitalization, YMRS score at intake, HAM-D score at intake, number of medication classes prescribed at discharge from index hospitalization, and duration of index hospitalization were also examined as explanatory variables. Moreover, presence of antimanic agents and presence of psychosocial intervention at the time of syndromic recovery were examined as explanatory variables for propensity analyses of the effects of medication exposure on syndromic recurrence. Finally, having a depressive episode that preceded antidepressant treatment was examined as an explanatory variable for antidepressants; however, this was not predictive of antidepressant treatment (p=0.60). Logistic regression analyses were used to estimate the conditional probability of being prescribed each type of medication for each of the explanatory variables that significantly differed between the prescribed and nonprescribed groups; the predicted probabilities from the fitted models were then used as propensity scores. Socioeconomic status, ADHD, disruptive behavior disorders, anxiety disorders, and number of medications at the time of discharge from index hospitalization were included in the propensity scores for mood stabilizers (psychotherapy at syndromic recovery was added for syndromic recurrence analysis); baseline psychosis status and number of medications at the time of discharge from index hospitalization were included for antipsychotics; socioeconomic status, baseline psychosis status, anxiety disorders, alcohol use disorders, baseline HAM-D and YMRS scores, length of index episode, and number of medications at the time of discharge from index hospitalization were included for antidepressants (psychotherapy at syndromic recovery was added for syndromic recurrence analysis); and sex, socioeconomic status, ADHD, disruptive behavior disorders, baseline psychosis status, baseline HAM-D score, and number of medications at the time of discharge from index hospitalization were included for psychostimulants. The propensity score for each medication category was included in regression models comparing outcome measures between patients who were adherent with a specific medication category and the remainder of the cohort. Other statistical analyses were performed as necessary.
Results
Baseline Characteristics
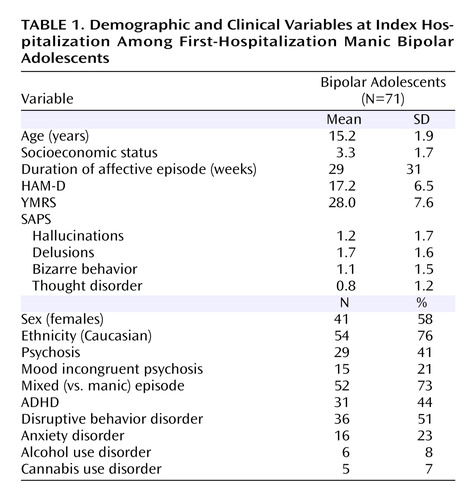
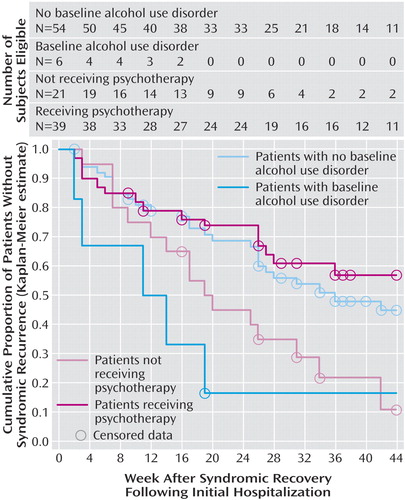
The demographic and clinical variables at initial hospitalization for all subjects (N=71) are listed in Table 1 . The index hospitalization was the result of the initial affective episode in 60 (85%) adolescents. However, 11 (15%) adolescents had a prior untreated major depressive episode. The mean length of index manic or mixed episode prior to first hospitalization was 19 (SD=20) weeks.
Sixty-two (87%) of the 71 adolescents were interviewed at all follow-up intervals. There were no statistically significant differences in demographic, clinical, or outcome variables between patients with (N=62) and without (N=9) 12 months of follow-up (p>0.10). Of the subjects who did not complete all 12 months of follow-up, most (7/9 [78%]) completed at least 8 months, and all had at least one follow-up interview.
Pharmacological Treatment Adherence
During the initial year following first hospitalization, 42 (59%) adolescents were treated with at least one mood stabilizer (40 [95%] with lithium and/or valproic acid, one [2.4%] with topiramate, and one [2.4%] with lamotrigine), 47 (66%) with an atypical antipsychotic, 17 (24%) with an antidepressant, and 19 (27%) with a psychostimulant. Twenty-five (35%) adolescents reported full adherence, 30 (42%) reported partial adherence, and 16 (23%) reported nonadherence. The results of all analyses were unchanged by combining the partially adherent and nonadherent groups into a nonadherent group (12) .
Logistic regression analyses revealed that ADHD (F=9.7, df=1, 70, p=0.003) and low socioeconomic status (F=4.5, df=1, 70, p=0.04) were associated with nonadherence. Specifically, bipolar adolescents with ADHD were less likely to be medication adherent than those without ADHD (5 [16%] versus 20 [50%], χ 2 =8.9, p=0.003). Socioeconomic status was higher in medication adherent compared with nonadherent bipolar adolescents (t=–2.1, p=0.04). None of the adolescents with an alcohol use disorder (N=6) were medication adherent compared with 25 (38%) of the adolescents without an alcohol use disorder (N=65, χ 2 =3.8, p=0.06).
Syndromic Recovery and Recurrence
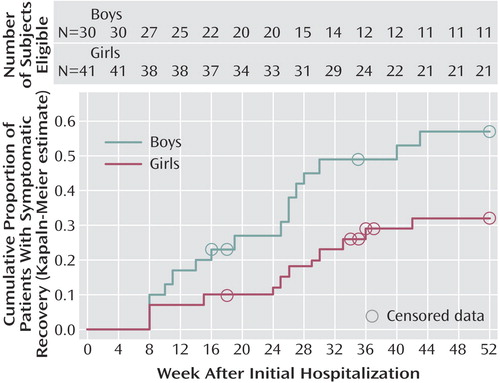
Sixty (85%) adolescents had syndromic recovery during the first year following initial hospitalization. The Kaplan-Meier estimate of cumulative probability of syndromic recovery was 0.86 (95% CI=0.78 to 0.94), with a mean time to syndromic recovery of 20 (SD=13) weeks following initial hospitalization ( Figure 1 ). Total episode duration (mean time from index episode onset to no longer having any DSM-IV mood episode) was 27 (SD=30) weeks.
a During the initial year following first hospitalization for a manic episode in adolescents with bipolar disorder (N=71), cumulative probability of syndromic recovery=0.86, 95% CI=0.78 to 0.94; cumulative probability of symptomatic recovery=0.43, 95% CI=0.31 to 0.55; cumulative probability of functional recovery=0.41, 95% CI=0.29 to 0.53.
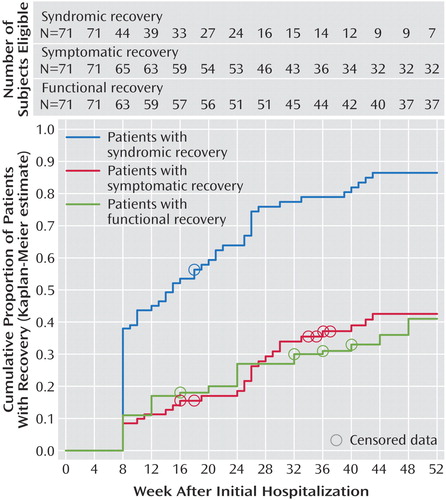
Kaplan-Meier analyses revealed that co-occurring anxiety disorders (log-rank: χ 2 =6.3, p=0.01), disruptive behavior disorders (log-rank χ 2 =7.1, p=0.007), and ADHD (log-rank: χ 2 =13, p=0.0003) as well as medication nonadherence (log-rank: χ 2 =3.8, p=0.05) were associated with lower rates of syndromic recovery ( Figure 2 ). Furthermore, Cox regression analysis revealed that ADHD (hazard ratio=2.4, 95% CI=1.4 to 4.0, p=0.002), nonadherence (hazard ratio=1.7, 95% CI=1.0 to 2.9, p=0.04), and lower socioeconomic status (hazard ratio=1.2, 95% CI=1.0 to 1.3, p=0.002) were associated with longer time to syndromic recovery following initial hospitalization. ADHD was the only predictor that remained statistically significant in the stepwise Cox regression analysis (p<0.02).
a Left: At 1 year following first hospitalization for a manic episode in bipolar adolescents with ([N=31] cumulative probability=0.75, 95% CI=0.61 to 0.91) and without ([N=40] cumulative probability=0.95, 95% CI=0.87 to 1.0) ADHD and who were ([N=25] cumulative probability=0.95, 95% CI=0.86 to 1.0) and were not ([N=46] cumulative probability=0.83, 95% CI=0.71 to 0.94) adherent with their prescribed psychotropic medications. Right: In bipolar adolescents with ([N=16] cumulative probability=0.79, 95% CI=0.57 to 1.0) and without ([N=55] cumulative probability=0.89, 95% CI=0.78 to 0.94) an anxiety disorder and with ([N=36] cumulative probability=0.85, 95% CI=0.73 to 0.97) and without ([N=35] cumulative probability=0.87, 95% CI=0.75 to 0.99) a disruptive behavior disorder.
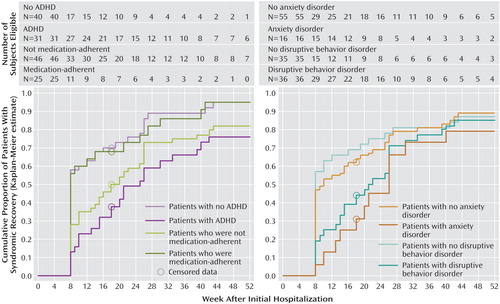
Thirty-one (52%) of the 60 adolescents who had syndromic recovery had at least one syndromic recurrence (14 [45%] mania, 12 [39%] depression, and 5 [16%] mixed episode) within the first year following initial hospitalization. The mean length of the recurrent episode was 8 (SD=8) weeks. The cumulative probability of syndromic recurrence was 0.54 (95% CI=0.41 to 0.66), with a mean time to syndromic recurrence of 17 (SD=11) weeks following syndromic recovery.
Kaplan-Meier estimates revealed that alcohol use disorders (log-rank: χ 2 =9.3, p=0.002) and no psychotherapeutic intervention following hospitalization (log-rank: χ 2 =7.4, p=0.007) were associated with syndromic recurrence ( Figure 3 ). Time to syndromic recurrence was shorter in patients with alcohol use disorders (hazard ratio=4.3, 95% CI=3.3 to 5.3, p=0.005). Moreover, time to syndromic recurrence was longer in patients who received any psychotherapeutic intervention prior to syndromic recurrence compared with those who did not (hazard ratio=2.6, 95% CI=1.3 to 3.9, p=0.009). Propensity analysis revealed that antidepressant treatment was associated with a shorter time to syndromic recurrence (hazard ratio=2.5, 95% CI=1.8 to 3.2, p=0.01).
a During the initial year following first hospitalization for a manic episode in bipolar adolescents who did ([N=6] cumulative probability=0.83, 95% CI=0.54 to 1) and did not ([N=54] cumulative probability=0.55, 95% CI=0.39 to 0.71) have a baseline alcohol use disorder and who did ([N=39] cumulative probability=0.43, 95% CI=0.26 to 0.60) and did not ([N=21] cumulative probability=0.89, 95% CI=0.71 to 1) have psychotherapy prior to recurrence.
Symptomatic Recovery
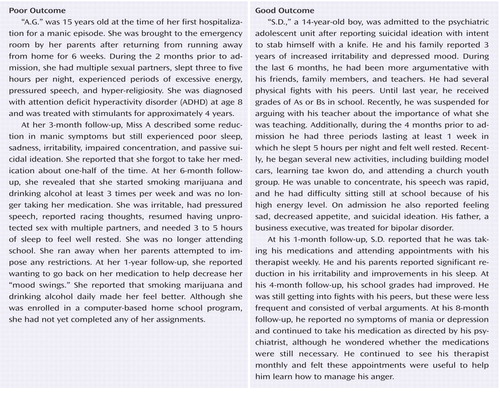
Bipolar adolescents spent 38% of the first year following their initial hospitalization with an affective episode (63% mixed episodes, 22% mania/hypomania, and 15% depression), 46% of the time with subsyndromal symptoms (90% manic/hypomanic symptoms and 10% depressive and manic/hypomanic symptoms), and 16% of the time asymptomatic. Twenty-eight (39%) adolescents achieved symptomatic recovery. The cumulative probability of symptomatic recovery was 0.43 (95% CI=0.31 to 0.55), with a mean time of 35 (SD=13) weeks following initial hospitalization ( Figure 1 ). Boys had a greater probability of symptomatic recovery compared with girls (log-rank χ 2 =4.4, p=0.03) ( Figure 4 ). Cox regression analysis revealed that boys had a shorter time to symptomatic recovery than girls (hazard ratio=2.2, 95% CI=1.1 to 4.7, p=0.04).
a During the initial year following first hospitalization for a manic episode in bipolar adolescents girls ([N=41] cumulative probability=0.32, 95% CI=0.17 to 0.47) and boys ([N=30] cumulative probability=0.57, 95% CI=0.39 to 0.75).
Functional Recovery
Twenty-eight (39%) adolescents achieved functional recovery. The cumulative probability of functional recovery was 0.41 (95% CI=0.29 to 0.53), with a mean time of 38 (SD=16) weeks following initial hospitalization ( Figure 1 ). Kaplan-Meier estimates and Cox regression analyses revealed no statistically significant predictors of functional recovery.
Examination of each of the individual subscales of functional recovery revealed that the cumulative probability of recovery was 0.97 (95% CI=0.93 to 1.0, mean=11 [SD=8] weeks following initial hospitalization) for sexual activity, 0.92 (95% CI=0.84 to 0.98, mean=17 [SD=13] weeks) for role performance, 0.80 (95% CI=0.71 to 0.89, mean=20 [SD=16] weeks) for recreational enjoyment, and 0.73 (95% CI=0.62 to 0.84, mean=24 [SD=18] weeks) for interpersonal relationships. Bipolar adolescents with ADHD (hazard ratio=2.0, 95% CI=1.2 to 3.3, p=0.01) or a disruptive behavior disorder (hazard ratio=1.8, 95% CI=1.1 to 2.9, p=0.03) were less likely to recover in the area of role performance and those who were younger (hazard ratio=1.2, 95% CI=1.0 to 1.4, p=0.04) were more likely to recover in the area of recreational enjoyment.
There were no statistically significant differences in the rate of functional recovery between adolescents who did (25/60 [42%]) and did not (3/11 [27%]) have syndromic recovery (χ 2 =0.8, p=0.37), nor in the rate of functional recovery between adolescents who did (14/28 [50%]) and did not (14/43 [33%]) have symptomatic recovery (χ 2 =2.2, p=0.14).
Discussion
To our knowledge, this is the first study to assess symptomatic, syndromic, and functional outcomes and the effect of medication adherence on outcome of bipolar adolescents following initial hospitalization for mania. Prior outcome studies of bipolar youth have used variable definitions of recovery, making it difficult to directly compare the findings from these studies. Nonetheless, consistent with the findings of most (3 , 8 , 9 , 11) , but not all (4 – 7) , studies of bipolar adolescents, the results of our study indicate that most bipolar adolescents experienced syndromic recovery. However, only 20% of bipolar adolescents experienced all three types of recovery, indicating that most bipolar adolescents continued to have impairment in at least one domain and emphasizing the importance of assessing symptomatic and functional outcomes in bipolar youth. Recently, Birmaher et al. reported that youth with bipolar I disorder spent 32% of the time with subsyndromal mood symptoms and had a symptomatic recovery rate of 68% and a syndromic recurrence rate of 58%. In comparison, we found that bipolar adolescents spent 46% of the time with subsyndromal mood symptoms and had a symptomatic recovery rate of 39% and a syndromic recurrence rate of 52%. Longer duration of follow-up (mean 95 weeks) and including outpatients (65%) may have contributed to the better outcomes reported by Birmaher et al.
Birmaher et al. (3) also compared their findings with those of a study of bipolar adults that used similar methodology (33) and concluded that bipolar youth have a more severe illness course. In contrast, we compared our findings with those of Keck et al., who reported that during the 12 months following hospitalization for a manic episode, 48%, 26%, and 24% of bipolar adults experienced syndromic, symptomatic, and functional recovery, respectively. However, Keck et al. did not exclude bipolar patients with prior affective episodes, providing additional support that longer illness duration may be a negative predictor of outcome (12) . Indeed, Birmaher et al. found that for every year of illness, bipolar youth had a 10% lower likelihood of recovery (3) .
The effects of treatment adherence on outcome of bipolar youth are largely unknown. Recently, Coletti et al. found that only 34% of bipolar adolescents reported full medication adherence during a 1-month assessment period (34) and reported that patients with optimal medication adherence were diagnosed more recently than those who had missed one or more medication doses, suggesting that early in illness course bipolar adolescents may be more treatment adherent than later in illness course (34) . However, despite using a more lenient definition of full medication adherence, we found that nonadherence rates for bipolar adolescents are high (65%), even early in illness course. Factors associated with poor medication adherence included co-occurring ADHD and alcohol use disorders and low family socioeconomic status. Although our study cannot determine the causal relationships among these factors, we speculate that patients with ADHD are more likely to forget to take their medications, and patients in families of lower socioeconomic status may have limited access to medications. However, we did not systematically collect information regarding the reasons for medication nonadherence. Additionally, our finding of higher nonadherence in first-episode manic adolescents who were diagnosed with an alcohol use disorder at baseline and then prospectively assessed for adherence suggests that alcohol use may be a risk factor for poor medication adherence (versus poor adherence leading to the development of an alcohol use disorder) in bipolar adolescents.
In general, we found that distinct predictors were associated with each of the outcome measures. However, we were unable to determine the independent effects of poor medication adherence, socioeconomic status, and ADHD on syndromic recovery because of the high colinearity among these risk factors. Post hoc exploratory analyses of the associations among these factors suggests that independent of ADHD status, medication adherence had a greater impact on time to syndromic recovery in bipolar adolescents of higher socioeconomic status than in those of lower socioeconomic status. Although additional studies are needed, these findings imply that the quality of care varies among bipolar adolescents of different socioeconomic levels. Consistent with outcome studies of bipolar adults (12 , 15 , 35 , 36) , we found that alcohol use was associated with a greater risk of recurrence, highlighting the importance of educating bipolar adolescents about the negative impact of substance use on illness outcome. Additionally, these findings stress the need for developing effective treatment strategies for adolescents with co-occurring bipolar and substance use disorders. Although treatment in this study was naturalistic, our results suggest that antidepressants may be associated with greater risk of syndromic recurrence. In contrast, prior studies indicate that, in combination with mood stabilizers, antidepressants may be useful for the treatment of bipolar youth (37) . Consistent with Birmaher et al. (3) , we found that boys were twice as likely as girls to experience symptomatic recovery. Future studies are needed to examine whether gender differences in treatments, medication adherence, and other clinical characteristics may contribute to these findings. Moreover, consistent with prior studies (38) , we identified that psychotherapeutic interventions may be effective in preventing recurrent mood episodes in bipolar adolescents. However, controlled studies of specific psychotherapeutic strategies are needed.
Inconsistent with prior studies of bipolar youth (3 , 7) , our results did not reveal that psychosis was predictive of any outcome measure. A possible explanation for this finding is that psychosis has been a marker of illness severity in prior studies that have included cohorts of both inpatients and outpatients. In contrast, our cohort was recruited exclusively from an inpatient setting, and therefore the patients may have been more severely ill than those of prior studies.
In summary, our findings indicate that adolescent-onset bipolar disorder is associated with poor medication adherence, persistent affective symptoms, and functional impairment. However, there are several limitations that should be considered when interpreting the results of our study. First, our cohort was recruited from a single inpatient site, which may limit the ability to generalize our findings. Second, although our study is a prospective study, adolescents and their family members were interviewed retrospectively at each follow-up visit, which might have limited their ability to accurately recall mood symptoms. However, in order to improve the accuracy of the information obtained, subjects and their primary caregivers were each interviewed, interviews were performed frequently (at 1, 4, 8, and 12 months), and all subjects were reminded of anchor time points (i.e., holidays, birthdays, and school events) that occurred during each follow-up period. Third, although our study is the first to assess treatment adherence as a predictor of outcome in bipolar youth, we based adherence ratings on patient reports and independent information ascertained from their family members. Measurement of serum concentrations of prescribed medications may be a more valid method for assessing medication adherence. Fourth, similar to some prior outcome studies (4 – 13) , we calculated time to recovery from initial hospitalization; however, this may not accurately reflect actual episode duration. In contrast, other studies (3) assessed time to recovery from the onset of the index mood episode, although information regarding episode duration prior to hospitalization is often based on retrospective recall from patients and their legal guardians and thus may be subject to recall bias. Nonetheless, we reported both total episode duration and time to outcomes from initial hospitalization. Despite these limitations, our findings suggest that distinct predictors are associated with specific outcome measures in bipolar adolescents. Future studies of longer duration are needed to determine whether adolescents with bipolar disorder ultimately progress into adults with bipolar disorder.
1. Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM: The National Depressive and Manic-Depressive Association (DMDA) Survey of Bipolar Members. J Affect Disord 1994; 31:281–294Google Scholar
2. Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, Bowden CL, Sachs GS, Nierenberg AA: Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2004; 55:875–881Google Scholar
3. Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M: Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry 2006; 63:175–183Google Scholar
4. Geller B, Zimmerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo CA: Six-month stability and outcome of a prepubertal and early adolescent bipolar disorder phenotype. J Child Adolesc Psychopharmacol 2000; 10:165–173Google Scholar
5. Geller B, Craney JL, Bolhofner K, DelBello MP, Williams M, Zimmerman B: One year recovery and relapse rates of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2001; 158:303–305Google Scholar
6. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimmerman B: Two year prospective follow up of children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 2002; 159:927–933Google Scholar
7. Geller B, Tillman R, Craney JL, Bolhofner K: Four year prospective outcome and natural history of mania in children with prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry 2004; 61:459–467Google Scholar
8. Jairam R, Srinath S, Girimaji SC, Seshadri SP: A prospective 4–5 year follow-up of juvenile onset bipolar disorder. Bipolar Disord 2004; 6:386–394Google Scholar
9. Rajeev J, Srinath S, Reddy YC, Shashikiran MG, Girimaji SC, Seshadri SP, Subbakrishna DK: The index manic episode in juvenile-onset bipolar disorder: the pattern of recovery. Can J Psychiatry 2003; 48:52–55Google Scholar
10. Srinath S, Janardhan Reddy YC, Girimaji SR, Seshadri SP, Subbakrishna DK: A prospective study of bipolar disorder in children and adolescents from India. Acta Psychiatr Scand 1998; 98:437–442Google Scholar
11. Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M: Recovery and relapse in adolescents with bipolar disorder affective illness: a 5-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 1995; 34:724–731Google Scholar
12. Keck PE Jr, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, Bourne ML, Haggard P: 12-Month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry 1998; 155:646–652Google Scholar
13. Strakowski SM, Keck PE Jr, McElroy SL, West SA, Sax KW, Hawkins JM, Kmetz GF, Upadhyaya VH, Tugrul KC, Bourne ML: Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry 1998; 55:49–55Google Scholar
14. Geller B, Bolhofner K, Craney JL, Williams M, DelBello MP, Gunderson K: Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry 2000; 39:1543–1548Google Scholar
15. Strakowski SM, DelBello MP, Fleck DE, Adler CM, Anthenelli RM, Keck PE Jr, Arnold LM, Amicone J: Effects of cooccurring alcohol abuse on the course of bipolar disorder following a first hospitalization for mania. Arch Gen Psychiatry 2005; 62:851–858Google Scholar
16. Tohen M, Zarate CA Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ: The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry 2003; 160:2099–2107Google Scholar
17. Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo C: Reliability of the Washington University in St. Louis, MO, Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiatry 2001; 40:450–455Google Scholar
18. DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM: Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset. Bipolar Disord 2001; 3:53–57Google Scholar
19. Young RC, Biggs JT, Ziegler VE, Meyer DA: A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 1978; 133:429–435Google Scholar
20. Fristad MA, Weller EB, Weller RA: The mania rating scale: can it be used in children? A preliminary report. J Am Acad Child Adolesc Psychiatry 1992; 31:252–257Google Scholar
21. Hamilton M: A Rating scale for depression. J Neurol Neurosurg Psychiatr 1960; 23:56–61Google Scholar
22. Patel NC, DelBello MP, Kowatch RA, Strakowski SM: Preliminary study of relationships among measures of depressive symptoms in adolescents with bipolar disorder. J Child Adolesc Psychopharmacol 2006; 16:327–335Google Scholar
23. Andreasen NC: The Scale for the Assessment of Positive Symptoms (Scale for the Assessment of Positive Symptoms). Iowa City, University of Iowa, 1984Google Scholar
24. Hollingshead AB: Four-factor Index of Social Status. New Haven, Conn: Department of Sociology, Yale University, 1975Google Scholar
25. Leon AC, Solomon DA, Mueller TI, Endicott J, Posternak M, Judd LL, Schettler PJ, Akiskal HS, Keller MB: A brief assessment of psychosocial functioning of subjects with bipolar disorder: the Longitudinal Interval Follow-up Examination-RIFT. Longitudinal Interval Follow-Up Evaluation-Range Impaired Functioning Tool. J Nerv Ment Dis 2000; 188:805–812Google Scholar
26. Strakowski SM, Williams JR, Fleck DE, DelBello MP: Eight-month functional outcome from mania following a first psychiatric hospitalization. J Psychiatr Res 2000; 34:193–200Google Scholar
27. Strakowski SM, DelBello MP, Fleck DE, Arndt S: The impact of substance abuse on the course of bipolar disorder. Biol Psychiatry 2000; 48:477–485Google Scholar
28. DelBello MP, Carlson GA, Tohen M, Bromet EJ, Schwiers M, Strakowski SM: Rates and predictors of developing a manic or hypomanic episode 1 to 2 years following a first hospitalization for major depression with psychotic features. J Child Adolesc Psychopharmacol 2003; 13:173–185Google Scholar
29. Keller MB, Lavon PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Google Scholar
30. Kaplan EL, Meier P: Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53:457–481Google Scholar
31. Cox DR: Regression models and life tables. J R Stat Soc [Ser A] 1972; B34:187–220Google Scholar
32. D’Agostino RB: Tutorial in biostatistics: propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998; 1:2265–2281Google Scholar
33. Judd LL, Akiksal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB: The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002; 59:530–537Google Scholar
34. Coletti DJ, Leigh E, Gallelli KA, Kafantaris V: Patterns of adherence to treatment in adolescents with bipolar disorder. J Child Adolesc Psychopharmacol 2005; 15:913–917Google Scholar
35. Salloum IM, Cornelius JR, Mezzich JE, Kirisci L: Impact of concurrent alcohol misuse on symptom presentation of acute mania at initial evaluation. Bipolar Disord 2002; 4:418–421Google Scholar
36. Weiss RD, Ostacher MJ, Otto MW, Calabrese JR, Fossey M, Wisniewski SR, Bowden CL, Nierenberg AA, Pollack MH, Salloum IM, Simon NM, Thase ME, Sachs GS; for STEP-BD Investigators: Does recovery from substance use disorder matter in patients with bipolar disorder? J Clin Psychiatry 2005; 66:730–735Google Scholar
37. Biederman J, Mick E, Spencer TJ, Wilens TE, Faraone SV: Therapeutic dilemmas in the pharmacotherapy of bipolar depression in the young. J Child Adolesc Psychopharmacol 2000; 10:185–192Google Scholar
38. Lofthouse N, Fristad MA: Psychosocial interventions for children with early onset bipolar spectrum disorder. Clin Child Fam Psychol Rev 2004; 7:71–88Google Scholar