Chronic Restlessness With Antipsychotics
Mr. B is a 34-year-old man with a 13-year history of schizophrenia. His early treatment consisted of brief trials of first-generation antipsychotics, which he refused to take for any significant period of time. He was then started on risperidone at an average of 5 mg/day. Within a few months, he and his mother noticed that he had upper and lower extremity tremor and profound motor restlessness, especially of the legs. These symptoms worsened until Mr. B was taken off risperidone and started on olanzapine, after which the tremor resolved, but the restlessness persisted. Mr. B’s discomfort was so severe that he was unable to sit through a 15-minute medication management appointment without getting up and pacing the room. His mother noted that the restlessness lasted throughout the day, relenting only when he slept. Mr. B stated that he could not stay still for more than a few minutes at a time and that he had an irresistible urge to move, which led him to pace the house and neighborhood until the soles of his feet were bleeding. Mr. B’s mother also reported that when the restlessness was at its worst, he was extremely irritable, easily agitated, and sometimes violent.
Acute and Tardive Akathisia
Akathisia is one of the most common acute movement disorders (1) , but it also exists in chronic and tardive forms. These akathisia variants are less well recognized but are equally—and sometime more—debilitating to patients. The word “akathisia” (derived from Greek, literally meaning “not to sit”) was first used in 1901 by Haskovec (2) to describe two patients who experienced restlessness and an inability to sit still. In contemporary usage, akathisia refers to a drug-induced movement disorder. Akathisia presents as a syndrome of motor restlessness, usually in the lower extremities, that is often (but not always) accompanied by a subjective sense of inner restlessness, an urge to move, and anxiety or dysphoria (3) .
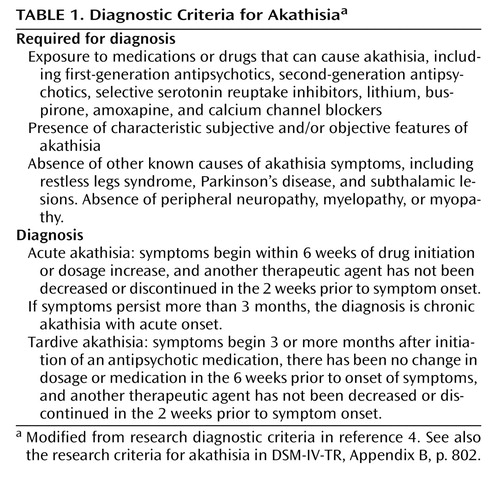
Most cases of akathisia are acute and are dose related ( Table 1 ). Chronic akathisia is defined as akathisia persisting more than 3 months after the last antipsychotic dosage change; it does not address acuity of onset (4) . Tardive akathisia has a delayed onset, with symptoms beginning 3 months or more after medication initiation or dosage increase (4) . Some patients, such as the patient presented in the clinical vignette, demonstrate an “unmasking” or worsening of symptoms with drug withdrawal and an improvement with dosage increase. This is often referred to as “withdrawal akathisia” (4) . Tardive akathisia often persists even in the absence of antipsychotic medication. Burke et al. (5) reported akathisia persisting for an average of 2.7 years in 26 patients whom they followed after discontinuation of antipsychotic medications.
Epidemiology of Akathisia
The published epidemiological data for akathisia are largely limited to treatment periods that preceded the widespread use of second-generation antipsychotics. Sachdev (6) reported an incidence rate of acute akathisia of 31% for 100 patients treated for 2 weeks with antipsychotic medications. He suggested that “a conservative estimate of incidence of [acute] akathisia with classical neuroleptics at clinical dosage levels is … 20%–30%” (6, 7). In a review of the literature on chronic akathisia, Sachdev (8) reported a prevalence rate ranging from 0.1% to 41%. Barnes and Braude (3) reported a prevalence rate of about 33% for chronic akathisia in a group of outpatients with schizophrenia. Presumably the rates are lower in the current treatment climate because of the lower risk of akathisia with second-generation antipsychotics.
Pathophysiology of Akathisia in Schizophrenia
The pathophysiology of akathisia is poorly understood, but it appears to differ from that of extrapyramidal symptoms. The prevailing hypothesis for both is that the symptoms are due to antipsychotic-induced dopamine D 2 receptor occupancy above a threshold of 80% (9) . However, in individual patients there is not a clear relationship between the severity of akathisia and other extrapyramidal symptoms, such as rigidity and tremor. This suggests that the striatonigral dopamine pathway involved in the pathophysiology of extrapyramidal symptoms is unlikely to be the main pathway in akathisia (10) . Cholinergic and adrenergic pathways may play a mediating role (10) ; in both cases, the majority of available evidence for their involvement comes from the clinical utility of anticholinergic and antiadrenergic (b 2 antagonists) medications in improving akathisia (10) . Similarly, second-generation antipsychotics with high cholinergic receptor affinities carry a lower risk of akathisia (9) . Investigators have hypothesized that serotonergic pathways may be implicated, because serotonergic medications, such as selective serotonin reuptake inhibitors, can induce akathisia, and antagonism of serotonin (especially 5-HT 2A ) by some second-generation antipsychotics can reduce akathisia symptoms (10) .
Risk Factors for Akathisia
Various risk factors have been associated with akathisia. Some treatment risk factors include higher drug dosages, rapid increment of dosage, and higher-potency antipsychotic medications (10) . Individual risk factors include higher age, female sex, negative symptoms, iron deficiency, cognitive dysfunction, and affective disorder diagnoses (8) .
Diagnosis
Table 1 lists the diagnostic criteria for akathisia, and Table 2 presents the features and differential diagnoses of various movement syndromes.
The diagnosis of akathisia can be difficult (16) , particularly since the medications most often implicated in akathisia are those most likely to have been prescribed for treatment of psychotic agitation. Akathisia is often mistaken for anxiety or worsening of psychotic agitation, and anxiety and agitation often accompany akathisia and further complicate the differential diagnosis. Another factor complicating diagnosis is that akathisia symptoms can vary in severity over time, particularly in mild cases. The assessment of akathisia in clinical trials usually involves rating scales that may include measures of both subjective and objective components. The most widely used scale today is the Barnes Akathisia Rating Scale (17) . Although akathisia scales have demonstrated reliability and validity, investigators are rarely well trained in their use, and interrater reliability is seldom established in large multicenter trials, making it difficult to develop accurate estimates of incidence, prevalence, and risk factors. Furthermore, akathisia can often be suppressed with distraction; if clinicians are monitoring for akathisia only under brief and formal examinations, the diagnosis may be overlooked (1) .
Restless legs syndrome and akathisia have many symptoms in common (15 , 18) , and direct-to-consumer marketing of medications for restless legs syndrome may lead to confusion of this disorder with akathisia. Making the distinction is critical, because the treatment for restless legs syndrome (dopamine agonists such as ropinirole and pramipexole [19] ) may worsen psychosis, necessitating higher dosages of antipsychotic medication and ultimately worsening the akathisia. We have included a column on restless legs syndrome in Table 2 to aid in making the diagnostic distinction. The important distinguishing features of restless legs syndrome are that symptoms usually occur only during periods of rest, relaxation, or sleep and that the symptoms follow a circadian pattern and are typically worse in the evening or at night (15) .
Differentiating tardive akathitic movements from tardive dyskinetic movements can also be difficult, especially in circumstances where both conditions may be present. Tardive akathisia can share features with tardive dyskinesia. A study of akathisia in patients taking first-generation antipsychotics found that one-third to two-thirds of those with tardive akathisia had either orofacial or choreoathetoid limb dyskinesias suggestive of tardive dyskinesia (3). It is unclear whether tardive akathisia is a separate disorder or a variation of the manifestations of tardive dyskinesia (6). The choreic movements of tardive dyskinesia should be distinguished from some of the more complex and rare manifestations of akathisia, including face and thigh rubbing, scratching, and trunk rocking (1). There are several important distinguishing features. The first is that tardive akathitic movements can be voluntarily suppressed, at least briefly. The second is that akathitic movements are complex and demonstrate an intact motor control (4) .
Contribution of Akathisia to Psychopathology
Akathisia is an uncomfortable and distressing side effect, so much so that the diagnostic criteria include subjective discomfort. The presence of akathisia is correlated with medication noncompliance and has been associated with a worsening of psychotic symptoms, impulsive, aggressive, and self-injurious behavior, and even suicidality (1 , 20 – 22 ). The agitation and restlessness typical of akathisia, especially the acute variant, can be mistaken for psychotic agitation. This can lead to increases in antipsychotic dosages and further worsening of the akathisia. On the other hand, lowering the antipsychotic dosage to find the lowest effective dosage can lead to symptoms such as agitation, aggression, anxiety, and hyperactivity. These may be interpreted as a reemergence of the targeted psychiatric condition, but they may also be an unmasking of tardive akathisia (22) .
First-Generation Versus Second-Generation Antipsychotics
When chlorpromazine, the first widely used antipsychotic, was introduced in 1954, the potential for a variety of extrapyramidal side effects quickly became apparent. (In fact, some observers [23] suggested that parkinsonian side effects, specifically micrography, could be used to detect the dosage threshold for antipsychotic efficacy.) The assumption that antipsychotic drug treatment had to come with a high risk of movement disorder was challenged with the introduction of clozapine, the first antipsychotic medication that had a qualitatively lower risk of inducing extrapyramidal side effects (24) .
Between the 1960s and the 1980s, much was learned about the incidence, prevalence, and risk factors for neuroleptic-induced movement disorders—acute dystonic reactions, akinesia, motor rigidity, tremor, akathisia, and tardive (or late-occurring) syndromes such as tardive dyskinesia, tardive dystonia, and tardive akathisia. Throughout these decades, however, a number of investigators continued to voice concern that these disorders were often missed completely, falsely attributed to psychopathology and undertreated, even when diagnosed (20 , 25 , 26) . The consequences of these disorders were often significant in terms of personal distress, functional impairment, stigmatization, and nonadherence (21) .
The introduction of clozapine served as an impetus to develop other compounds with the “atypical” characteristic of a lower propensity to cause movement disorders. In general, the second-generation antipsychotics are less likely than first-generation antipsychotics to produce extrapyramidal symptoms (27 , 28) . Although low dosages (less than 600 mg chlorpromazine-equivalents) of the low-potency conventional antipsychotics are an exception to this generalization, the second-generation medications have been shown to have superior efficacy to low-dose, low-potency conventional antipsychotics (8) . In the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study (29) , no significant differences between antipsychotics were observed in rating scale scores for extrapyramidal symptoms, yet the rate of discontinuation because of extrapyramidal side effects was significantly higher among patients taking perphenazine, the only first-generation medication in the study, than among those taking second-generation medications. This finding suggests a notable disconnect between rating scale measures for movement disorders and the clinical impact of such disorders. Patients in the CATIE study who had a prior diagnosis of tardive dyskinesia were also excluded from the perphenazine arm, diluting the impact of movement side effects from first-generation antipsychotics in the study. Furthermore, it is likely that CATIE raters were not sensitive to milder manifestations of akathisia and other movement disorder syndromes (30) , which would also have reduced measured differences among medications in extrapyramidal side effects.
In general, the second-generation antipsychotics produce lower rates of akathisia compared with haloperidol even when low dosages of haloperidol are used (31 – 37) . Differences among the second-generation medications, however, are neither clear nor consistent. The CATIE investigators (29) reported similar rates of akathisia in phase 1 among the second-generation antipsychotics (ranging from 5% to 9%). Aside from the CATIE trial, there is a paucity of data regarding the relative risk of akathisia among the second-generation antipsychotics.
Tardive dyskinesia was first observed shortly after the introduction of chlorpromazine. With conventional antipsychotics, the incidence of tardive dyskinesia is generally reported to be 5% per year, at least for the first 5 years of treatment (38) . The incidence with second-generation antipsychotics appears to be significantly lower, approximately 1% per year on average (39) ; however, the available studies are limited by methodological problems and relatively brief follow-up periods.
Tardive akathisia, unlike tardive dyskinesia, has not been widely studied or universally accepted. Second-generation antipsychotics are probably less likely than the first-generation antipsychotics to produce tardive akathisia, but no systematic data are currently available.
Assessment of Akathisia and Other Movement Disorders
Although the introduction of the second-generation antipsychotics has decreased the prevalence and severity of neurological side effects in patients treated with antipsychotics, acute and chronic extrapyramidal side effects remain relatively common. For some individuals, these symptoms can constitute a substantial symptom burden that can be difficult to detect. This is particularly true for restlessness, which, as mentioned above, can be difficult to discriminate from agitation or anxiety. We recommend examining patients for acute, chronic, and tardive akathisia as a component of a regular evaluation of extrapyramidal symptoms. The Mount Sinai guidelines on the pharmacotherapy of schizophrenia (40) recommend a relatively complete examination for extrapyramidal symptoms and tardive dyskinesia before a patient is started on a new medication, and then every 6 months for patients who receive a first-generation antipsychotic and every 12 months for those receiving a second-generation antipsychotic. The guidelines recommend more frequent monitoring for individuals at high risk, such as elderly patients.
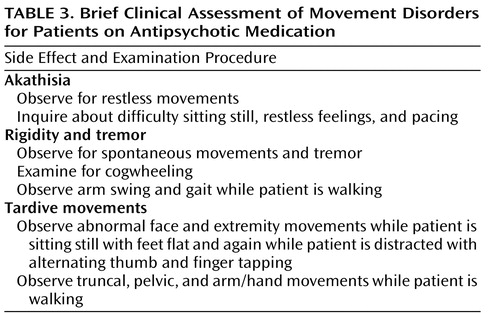
The Mount Sinai guidelines represent a minimal level of monitoring. More frequent monitoring that focuses on the most common side effects may be appropriate during acute treatment, during periods of dosage adjustment, and when there is concern about specific side effects. In many clinical settings, heavy case loads may make it difficult for clinicians to administer a complete examination for extrapyramidal symptoms and abnormal involuntary movements. In such circumstances, we recommend a relatively brief examination that can be administered in less than 3 minutes ( Table 3 ). Since the goal of this examination is to detect mild movements, we are not recommending any system for rating. If abnormal movements are detected, we recommend systematic rating with descriptions of the symptoms.
Management of Akathisia
Relatively little information is available to guide clinicians in treating chronic or tardive akathisia (41 – 43) . Case reports (reviewed in reference 14) and small randomized studies (44 – 54) suggest that benzodiazepines, propranolol, and anticholinergics may be of some help in treating acute akathisia. We recommend trials of propranolol, anticholinergics, or benzodiazepines for reducing the immediate distress that patients experience from restlessness. In our experience, these treatments, which are already often inadequate for treating acute akathisia (41 – 43) , are even less effective in chronic akathisia.
If it is feasible to reduce the antipsychotic dosage, this should be done gradually. Changing the patient to an antipsychotic with a lower liability for extrapyramidal side effects—particularly clozapine—is supported by our clinical experience and by small randomized trials (55 , 56) and case series (57 , 58) . It is important to inform patients that there may be a delay of weeks or months from the time the antipsychotic regimen is changed until the patient experiences substantial relief.
Summary and Recommendations
Restlessness is a relatively common complaint in patients receiving antipsychotic medications. Possible causes include agitation, anxiety, and akathisia. It is important to bear in mind that the subjective experience of restlessness will not always lead to obvious increases in motor behavior. We recommend that clinicians regularly assess both subjective and objective restlessness. If restlessness is a result of akathisia, clinicians should assess whether it is acute or chronic. The differentiation can be made by considering the time of onset of the symptom as well as the response of the akathisia to changes in antipsychotic dosage.
If the diagnosis is chronic or tardive akathisia, we recommend trials of an anticholinergic, a central-acting beta-blocker, or a benzodiazepine to relieve the patient’s distress. At the same time, clinicians should consider changing the patient’s antipsychotic pharmacotherapy. Alternatives to be considered are lowering the dosage of antipsychotic, changing to a less potent second-generation antipsychotic, or changing to clozapine.
When Mr. B, from the clinical vignette, was transferred to the schizophrenia clinic, he was on a combination of 10 mg of olanzapine at bedtime, 2.5 mg of clonazepam three times a day, 0.5 mg of lorazepam once a day, 5 mg of trihexyphenidyl once a day, 2 mg of benztropine once a day, 20 mg of propranolol three times a day, and 25 mg of atenolol once a day. Akathisia was his primary complaint, despite the multiple medications aimed at ameliorating the restlessness. He denied active psychotic symptoms. The goal of treatment with Mr. B was to find a regimen that would allow adequate treatment of his schizophrenia while minimizing his movement disorder side effect.
Over the next 8 years, Mr. B had trials of up to 850 mg/day quetiapine, up to 60 mg of ziprasidone twice a day, up to 15 mg/day of aripiprazole, and combination treatments (usually due to prolonged cross-titration schedules) of olanzapine with quetiapine, ziprasidone with quetiapine, and aripiprazole with quetiapine. With each initial medication change or dosage increase, Mr. B would report an improvement in his akathisia, but the restlessness quickly returned; the symptoms were at their worst when he was on aripiprazole and ziprasidone. He was also restarted several times on lorazepam and propranolol, but improvements on benzodiazepines and beta-blockers were equally short-lived, and typically these medications were discontinued after several weeks or months. The medication regimen was changed fairly frequently in an effort to balance worsening akathisia at higher dosages of antipsychotic medication and emerging psychotic symptoms of paranoia, thought disorder, and anxiety at lower dosages. Although the presumptive diagnosis was tardive akathisia, based on the chronicity and the noted improvement on increasing antipsychotic dosage or switching medications, Mr. B was never off antipsychotic medications.
For many such patients, clozapine is the only effective strategy. In 2005, Mr. B was started on clozapine specifically to target the tardive akathisia. His dosage was titrated to 100 mg in the morning and 200 mg at bedtime, and it has remained stable since. Mr. B has not needed adjunctive antipsychotic medications, benzodiazepines, or beta-blockers for akathisia symptoms while on this regimen. He does still have symptoms of restlessness, but the symptoms are markedly better than they were prior to treatment with clozapine. Both Mr. B and his mother report that the akathisia, while still bothersome, is tolerable and manageable at this level.
1. Barnes TR: The Barnes Akathisia Rating Scale—revisited. J Psychopharmacol 2003; 17:365–370Google Scholar
2. Haskovec L: Akathisie. Bohemes Med Clin 1902; 17:704–708Google Scholar
3. Barnes TR, Braude WM: Akathisia variants and tardive dyskinesia. Arch Gen Psychiatry 1985; 42:874–878Google Scholar
4. Sachdev P: Research diagnostic criteria for drug-induced akathisia: conceptualization, rationale, and proposal. Psychopharmacology (Berl) 1994; 114:181–186Google Scholar
5. Burke RE, Kang UJ, Jankovic J, Miller LG, Fahn S: Tardive akathisia: an analysis of clinical features and response to open therapeutic trials. Mov Disord 1989; 4:157–175Google Scholar
6. Sachdev P: Akathisia and Restless Legs. New York, Cambridge University Press, 1995Google Scholar
7. Sachdev P: The epidemiology of drug-induced akathisia, I: acute akathisia. Schizophr Bull 1995; 21:431–449Google Scholar
8. Sachdev P: The epidemiology of drug-induced akathisia, II: chronic, tardive, and withdrawal akathisias. Schizophr Bull 1995; 21:451–461Google Scholar
9. Mattay VS, Casey DE: Neuroleptic-induced acute extrapyramidal syndromes and tardive dyskinesia, in Schizophrenia. Edited by Hirsch SR, Weinberger DR. Blackwell Scientific Science, 2003, pp 552–572Google Scholar
10. Sachdev PS, Brune M: Animal models of acute drug-induced akathisia: a review. Neurosci Biobehav Rev 2000; 24:269–277Google Scholar
11. Adler LA, Angrist B, Reiter S, Rotrosen J: Neuroleptic-induced akathisia: a review. Psychopharmacology (Berl) 1989; 97:1–11Google Scholar
12. Ayd FJ Jr: A survey of drug-induced extrapyramidal reactions. JAMA 1961; 175:1054–1060Google Scholar
13. Rodnitzky RL: Drug-induced movement disorders. Clin Neuropharmacol 2002; 25:142–152Google Scholar
14. Miller CH, Fleischhacker WW: Managing antipsychotic-induced acute and chronic akathisia. Drug Saf 2000; 22:73–81Google Scholar
15. Kushida CA: Clinical presentation, diagnosis, and quality of life issues in restless legs syndrome. Am J Med 2007; 120(suppl 1):S4–S12Google Scholar
16. Hirose S: The causes of underdiagnosing akathisia. Schizophr Bull 2003; 29:547–558Google Scholar
17. Barnes TR: A rating scale for drug-induced akathisia. Br J Psychiatry 1989; 154:672–676Google Scholar
18. Ekbom KA: Restless legs. JAMA 1946; 131:481–486Google Scholar
19. Hening WA: Current guidelines and standards of practice for restless legs syndrome. Am J Med 2007; 120(suppl 1):S22–S27Google Scholar
20. Van Putten T, Mutalipassi LR, Malkin MD: Phenothiazine-induced decompensation. Arch Gen Psychiatry 1974; 30:13–19Google Scholar
21. Van Putten T: Why do schizophrenic patients refuse to take their drugs? Arch Gen Psychiatry 1975; 31:67–72Google Scholar
22. Gualtieri CT: The problem of tardive akathisia. Brain Cogn 1993; 23:102–109Google Scholar
23. Haase JH: Uber Vorkommen und Deutung des psychomotorischen Parkinsonsyndroms bei Megaphen-bzw Largactil-Dauerbehandlung (Occurrence and interpretation of psychomotor parkinsonism in megaphen or largactil prolonged therapy). Der Nervenarzi 1954; 25:486–492Google Scholar
24. Kane J, Honigfeld G, Singer J, Meltzer H: Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988; 45:789–796Google Scholar
25. Rifkin A, Quitkin F, Klein DF: Akinesia: a poorly recognized drug-induced extrapyramidal behavioral disorder. Arch Gen Psychiatry 1975; 32:672–674Google Scholar
26. Van Putten T: The many faces of akathisia. Compr Psychiatry 1975; 16:43–47Google Scholar
27. Leucht S, Pitschel-Walz G, Abraham D, Kissling W: Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo: a meta-analysis of randomized controlled trials. Schizophr Res 1999; 35:51–68Google Scholar
28. Leucht S, Wahlbeck K, Hamann J, Kissling W: New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet 2003; 361:1581–1589Google Scholar
29. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators: Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353:1209–1223Google Scholar
30. Marder SR: Lessons from each drug trial (editorial). Am J Psychiatry 2007; 164:375–376Google Scholar
31. Arvanitis LA, Miller BG: Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo: the Seroquel Trial 13 Study Group. Biol Psychiatry 1997; 42:233–246Google Scholar
32. Hirsch SR, Kissling W, Bäuml J, Power A, O’Connor R: A 28-week comparison of ziprasidone and haloperidol in outpatients with stable schizophrenia. J Clin Psychiatry 2002; 63:516–523Google Scholar
33. Marder SR, Glynn SM, Wirshing WC, Wirshing DA, Ross D, Widmark C, Mintz J, Liberman RP, Blair KE: Maintenance treatment of schizophrenia with risperidone or haloperidol: 2-year outcomes. Am J Psychiatry 2003; 160:1405–1412Google Scholar
34. Marder SR, McQuade RD, Stock E, Kaplita S, Marcus R, Safferman AZ, Saha A, Ali M, Iwamoto T: Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res 2003; 61:123–136Google Scholar
35. Zimbroff DL, Kane JM, Tamminga CA, Daniel DG, Mack RJ, Wozniak PJ, Sebree TB, Wallin BA, Kashkin KB (Sertindole Study Group): Controlled, dose-response study of sertindole and haloperidol in the treatment of schizophrenia. Am J Psychiatry 1997; 154:782–791Google Scholar
36. Carlson CD, Cavazzoni PA, Berg PH, Wei H, Beasley CM, Kane JM: An integrated analysis of acute treatment-emergent extrapyramidal syndrome in patients with schizophrenia during olanzapine clinical trials: comparisons with placebo, haloperidol, risperidone, or clozapine. J Clin Psychiatry 2003; 64:898–906Google Scholar
37. Lieberman JA, Tollefson G, Tohen M, Green AI, Gur RE, Kahn R, McEvoy J, Perkins D, Sharma T, Zipursky R, Wei H, Hamer MM (HGDH Study Group): Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry 2003; 160:1396–1404Google Scholar
38. Kane JM, Woerner M, Weinhold P, Wegner J, Kinon B: A prospective study of tardive dyskinesia development: preliminary results. J Clin Psychopharmacol 1982; 2:345–349Google Scholar
39. Correll CU, Leucht S, Kane JM: Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry 2004; 161:414–425Google Scholar
40. Marder SR, Essock SM, Miller AL, Buchanan RW, Davis JM, Kane JM, Lieberman J, Schooler NR: The Mount Sinai conference on the pharmacotherapy of schizophrenia. Schizophr Bull 2002; 28:5–16Google Scholar
41. Lima AR, Bacaltchuk J, Barnes TR, Soares-Weiser K: Central action beta-blockers versus placebo for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev 2004; 4:CD001946Google Scholar
42. Lima AR, Soares-Weiser K, Bacaltchuk J, Barnes TR: Benzodiazepines for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev 2002; 1:CD001950Google Scholar
43. Rathbone J, Soares-Weiser K: Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev 2006; 4:CD003727Google Scholar
44. Parlak I, Erdur B, Parlak M, Ergin A, Ayrik C, Tomruk O, Turkcuer I, Ergin N: Midazolam vs diphenhydramine for the treatment of metoclopramide-induced akathisia: a randomized controlled trial. Acad Emerg Med 2007; 14:715–721Google Scholar
45. Dorevitch A, Durst R, Ginath Y: Propranolol in the treatment of akathisia caused by antipsychotic drugs. South Med J 1991; 84:1505–1506Google Scholar
46. Duncan EJ, Adler LA, Stephanides M, Sanfilipo M, Angrist B: Akathisia and exacerbation of psychopathology: a preliminary report. Clin Neuropharmacol 2000; 23:169–173Google Scholar
47. Hermesh H, Manor I, Munitz H: Propranolol: a treatment for pseudoakathisia. J Nerv Ment Dis 1994; 182:241–243Google Scholar
48. Kim A, Adler L, Angrist B, Rotrosen J: Efficacy of low-dose metoprolol in neuroleptic-induced akathisia. J Clin Psychopharmacol 1989; 9:294–296Google Scholar
49. Lipinski JF, Zubenko GS, Barreira P, Cohen BM: Propranolol in the treatment of neuroleptic-induced akathisia. Lancet 1983; 2:685–686Google Scholar
50. Lipinski JF Jr, Zubenko GS, Cohen BM, Barreira PJ: Propranolol in the treatment of neuroleptic-induced akathisia. Am J Psychiatry 1984; 141:412–415Google Scholar
51. Poyurovsky M, Pashinian A, Weizman R, Fuchs C, Weizman A: Low-dose mirtazapine: a new option in the treatment of antipsychotic-induced akathisia: a randomized, double-blind, placebo- and propranolol-controlled trial. Biol Psychiatry 2006; 59:1071–1077Google Scholar
52. Ratey JJ, Salzman C: Recognizing and managing akathisia. Hosp Community Psychiatry 1984; 35:975–977Google Scholar
53. Vinson DR, Drotts DL: Diphenhydramine for the prevention of akathisia induced by prochlorperazine: a randomized, controlled trial. Ann Emerg Med 2001; 37:125–131Google Scholar
54. Wells BG, Cold JA, Marken PA, Brown CS, Chu CC, Johnson RP, Nasdahl CS, Ayubi MA, Knott DH, Arheart KL: A placebo-controlled trial of nadolol in the treatment of neuroleptic-induced akathisia. J Clin Psychiatry 1991; 52:255–260Google Scholar
55. Spivak B, Mester R, Abesgaus J, Wittenberg N, Adlersberg S, Gonen N, Weizman A: Clozapine treatment for neuroleptic-induced tardive dyskinesia, parkinsonism, and chronic akathisia in schizophrenic patients. J Clin Psychiatry 1997; 58:318–322Google Scholar
56. Peacock L, Solgaard T, Lublin H, Gerlach J: Clozapine versus typical antipsychotics: a retro- and prospective study of extrapyramidal side effects. Psychopharmacology (Berl) 1996; 124:188–196Google Scholar
57. Chengappa KN, Shelton MD, Baker RW, Schooler NR, Baird J, Delaney J: The prevalence of akathisia in patients receiving stable doses of clozapine. J Clin Psychiatry 1994; 55:142–145Google Scholar
58. Levin H, Chengappa KN, Kambhampati RK, Mahdavi N, Ganguli R: Should chronic treatment-refractory akathisia be an indication for the use of clozapine in schizophrenic patients? J Clin Psychiatry 1992; 53:248–251Google Scholar