In This Issue
Costs of Mental Health Care for Adolescents
The true cost of treating mental illness in U.S. adolescents is $10–12 billion annually, according to estimates by Costello et al. (p. Original article: 36 ). Previous calculations did not include services in nonmedical settings, such as schools, juvenile justice settings, and social service agencies. Schools were the most common providers but accounted for only 13% of the costs. Based on a representative sample of 4,500 adolescents, the findings reinforce the need to integrate mental health care. They also underscore the lack of treatment—only one-third of adolescents with major psychiatric problems received mental health services from any agency. Dr. Philip Wang et al. discuss these findings in an editorial on p. Original article: 1 .
The Disinhibited Brain and Uninhibited Behavior
Evidence for the failure of inhibitory mechanisms in psychiatric illness ranges from the simple to the complex. Patients with schizophrenia typically are unable to suppress physiological reactions to predictable auditory clicks and tones. Hong et al. (p. Original article: 61 ) report that this lack of normal inhibition may reflect more than one dysfunctional process. Among 59 patients, abnormalities in two common measures of inhibition, the startle response and the P50 component of the EEG, often did not occur in the same patient. Leibenluft et al. (p. Original article: 52 ) demonstrated that failed attempts to inhibit motor responses elicited greater activation of the right ventral prefrontal cortex and bilateral striatum in comparison subjects than in children with bipolar disorder. Underactivation in patients could indicate an inability to engage these regions. Immature brain circuitry is one proposed factor in the risk-taking behaviors characteristic of adolescents. Pat-Horenczyk et al. (p. Original article: 66 ) found high levels of risky behavior by Israeli adolescents exposed to frequent threats of terrorist attacks. Boys reported taking more risks than girls, and the association between posttraumatic symptoms and risk taking was stronger for boys. Goldstein et al. (p. Original article: 43 ) found that monetary rewards of varying value elicited a complex pattern of brain responses in healthy subjects but not subjects addicted to cocaine. Further, objective and subjective measures of motivation in the addicted subjects were not correlated, suggesting disrupted perception of their own drive. In an editorial on p. Original article: 4 , Dr. Marc Potenza outlines the implications of research on impulsivity.
Targeted Cognitive Behavior Therapy
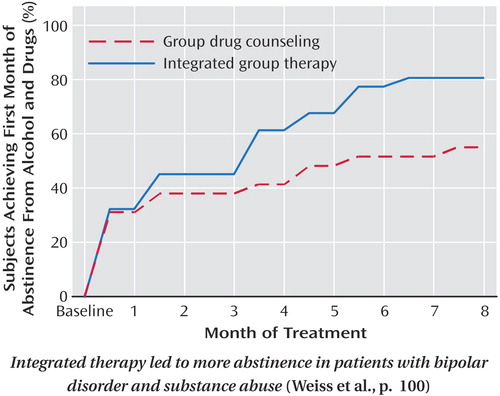
Cognitive behavior therapy (CBT) can target specific problems in a number of illnesses. For patients with co-occurring bipolar disorder and substance dependence, Weiss et al. (p. Original article: 100 ) found that CBT-based integrated group therapy reduced substance use more than group drug counseling did. Patients receiving integrated group treatment had fewer days of alcohol use but not less bipolar illness. Greeven et al. (p. Original article: 91 ) report a head-to-head comparison of CBT, paroxetine, and placebo for hypochondriasis. The rates of response after 16 weeks were higher for CBT (45%) and paroxetine (30%) than for placebo (14%). Sijbrandij et al. (p. Original article: 82 ) administered brief CBT to patients experiencing posttraumatic stress disorder (PTSD) within 3 months of a traumatic event. Four weekly sessions of CBT accelerated recovery from acute PTSD symptoms but did not affect outcome 4 months later. Randomized, controlled trials of psychotherapy, such as these, are the subject of an editorial by Dr. Arthur Rifkin (p. Original article: 7 ).
Perceived Need for Hospitalization in Patients With Eating Disorders
People with severe eating disorders sometimes accept inpatient treatment only under pressure. Guarda et al. (p. Original article: 108 ) found that 46 of 139 patients hospitalized for eating disorders disagreed with their admission but that 20 of the 46 agreed with the decision 2 weeks later. Patients with anorexia nervosa perceived greater coercion, greater pressure to be admitted, and less procedural justice than patients with bulimia nervosa. Adolescents were less likely to change their minds and perceived greater coercion. This difficult issue is discussed in an editorial by Dr. Arnold Andersen on p. Original article: 9 .



