In This Issue
Omega-3 Fatty Acids, Mood, and Suicide
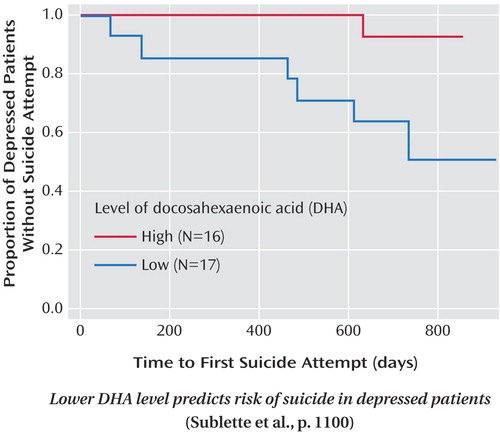
Research on links between dietary omega-3 polyunsaturated fatty acids and depression continues to show promise. Numerous epidemiological, cross-sectional, and treatment studies support the association between depression and low omega-3 levels, either absolute concentrations or a higher ratio of omega-6 to omega-3 fatty acids. It is now time, conclude Parker et al. (p. Original article: 969 ), for more specific investigations. Two examples appear in this issue. Treatment of depressed children ages 8–12 was tested in a double-blind study by Nemets et al. (p. Original article: 1098 ). A 50% reduction in depressive symptoms occurred in seven of 10 children receiving omega-3 fatty acids but none of 10 receiving placebo. The difference in response became apparent at week 8. The omega-3 fatty acids were a combination of EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) that is commonly available without a prescription. No side effects were reported. Sublette et al. (p. Original article: 1100 ) measured baseline fatty acids in depressed adults and tracked suicide attempts over 2 years. Suicide attempts were more likely among those with a low baseline DHA level and a high ratio of omega-6 to omega-3 fatty acids. EPA and arachidonic acid were not related to outcome. Changes in serotonin and corticotropin levels are among the possible mechanisms for DHA's effect.
Sticks, Stones, and Hurtful Words
Verbal aggression by parents is underestimated as a source of psychiatric symptoms, according to findings by Teicher et al. (p. Original article: 993 ). Among 554 young adults, parental verbal abuse during childhood was related to current anxiety, depression, anger/hostility, mental dissociation, and seizure-like events, such as brief hallucinations. Extraordinarily large effects were seen in subjects who had been verbally abused and had also witnessed domestic violence. The criteria for posttraumatic stress disorder currently include childhood physical maltreatment, sexual abuse, and witnessing of domestic violence but not verbal abuse. This large study indicates that parental verbal abuse during childhood is an equally potent risk factor.
Middle-Aged Children of Depressed Parents
A 20-year follow-up of 101 children of depressed parents by Weissman et al. (p. Original article: 1001 ) confirms high rates and early onset of major depression, anxiety disorders, and substance dependence. It also reveals a second, slight increase in new anxiety disorders between ages 28 and 32, primarily panic disorder among women. The offspring of depressed parents functioned more poorly at work and in their extended families than offspring of nondepressed subjects. At a mean age of 35 years, they also reported more medical problems. Fewer than half had obtained treatment for psychiatric disorders.
Pregnancy and Antidepressants: 4 Years Later
Taking a selective serotonin reuptake inhibitor (SSRI) during pregnancy may not affect offspring over the long term as much as the depression or anxiety for which the SSRI is prescribed. Misri et al. (p. Original article: 1026 ) discovered that at age 4, children of women who took SSRIs during pregnancy did not differ from children of nondepressed, nonmedicated mothers in internalizing behaviors, such as irritability and withdrawal. However, reports of their children's internalizing behaviors by mothers who had taken SSRIs were related to the mothers' own mood and anxiety levels. Despite treatment, over half of these women still had substantial depression or anxiety.
The Youngest Burn Victims
Preschoolers account for over 40% of the burns received by children and adolescents, but assessment of posttraumatic stress disorder (PTSD) is difficult when the patients have limited verbal ability. Among 30 children hospitalized for severe burns 1 month earlier, Stoddard et al. (p. Original article: 1084 ) found that a low frequency of spontaneous smiles correlated with high parental ratings of posttraumatic and other psychological symptoms and with a high heart rate during hospitalization. A low number of vocalizations correlated with the child's reaction to reminders of the burn and with the pain rating during hospitalization. These associations could guide development of a reliable tool for diagnosing PTSD in preverbal children.



