Prevalence and Correlates of Estimated DSM-IV Child and Adult Separation Anxiety Disorder in the National Comorbidity Survey Replication
Abstract
Objective: Despite its inclusion in DSM-IV, little is known about the prevalence or correlates of adult separation anxiety disorder or its relationship to the childhood disorder. Results of the first epidemiological study of adult separation anxiety disorder, to the authors’ knowledge, and its relationship to childhood separation anxiety disorder are presented. Method: Data were from the National Comorbidity Survey Replication (NCS-R), a nationally representative survey of U.S. households. A fully structured, lay-administered diagnostic interview assessed a wide range of DSM-IV disorders, including separation anxiety disorder. No independent clinical validation was obtained of the assessment. Results: Lifetime prevalence estimates of childhood and adult separation anxiety disorders were 4.1% and 6.6%, respectively. Approximately one-third of the respondents who were classified as childhood cases (36.1%) had an illness that persisted into adulthood, although the majority classified as adult cases (77.5%) had first onset in adulthood. The assessment of separation anxiety disorder in the NCS-R was comorbid with other NCS-R or DSM-IV disorders and associated with severe role impairment in roughly half of the comorbid cases and one-fourth of the pure cases. The majority of people with estimated adult separation anxiety disorder are untreated, even though many obtain treatment for comorbid conditions. Conclusions: Criteria for adult separation anxiety disorder should be refined in future editions of DSM because the disorder is likely to be much more common in adults than previously recognized. Research is needed to develop and evaluate treatments that take into consideration its high comorbidity with other DSM-IV disorders.
Although separation anxiety disorder is described in DSM-IV-TR as a childhood disorder that seldom persists into adulthood, the authors of several empirical studies have argued that adult separation anxiety disorder is more common than suggested by DSM-IV-TR (1 – 10) . This could be due to either of two possibilities. First, a higher proportion of childhood-onset cases might persist into adulthood than assumed in DSM-IV-TR. Second, at least some first onsets might occur in adulthood. Only a few short-term follow-up studies have evaluated the first possibility (11 , 12) . Although these studies showed that the vast majority of childhood cases remit before adulthood, they did not follow cases long enough to determine whether an adult form of the disorder subsequently reemerges in conjunction with the development of adult attachment relationships. A few studies of adult separation anxiety disorder evaluated the second possibility (2 , 13–15) . These studies consistently found a number of adults with separation anxiety disorder reports who never had childhood separation anxiety disorder. However, because these studies were all based on small and unrepresentative groups, no generalizations can be made about the prevalence or correlates of adult-onset separation anxiety disorder. Basic descriptive information about adult separation anxiety disorder would be of considerable interest for several reasons. Because separation anxiety disorder is only rarely diagnosed among adults in treatment, documentation of nontrivial prevalence and clinical significance would point to a problem of low recognition and treatment. This, in turn, would turn our attention to the relative importance of persistent childhood cases in relation to adult first-onset cases in accounting for adult cases. To address these issues, fully structured assessments of child and adult separation anxiety disorder were included in the recently completed National Comorbidity Survey Replication (NCS-R) (16) . Adults were assessed both for persistence of childhood separation anxiety disorder and for first onset in adulthood. This report presents basic descriptive information about the prevalence and correlates of childhood and adult separation anxiety disorder, including age-of-onset distributions, course, sociodemographic correlates, comorbidity, impairment, and treatment.
Method
Sample
As detailed elsewhere (17) , the NCS-R is a nationally representative survey of the English-speaking households in the coterminous United States. Face-to-face interviews were carried out with 9,282 respondents ages 18 and older between February 2001 and April 2003. The rate of response was 70.9%. Sample recruitment featured an advance letter and a study fact brochure followed by an in-person interviewer visit to answer questions before obtaining informed consent. Consent was obtained verbally rather than in writing to parallel the procedures used in the baseline National Comorbidity Survey (18) for the purposes of comparison. The human subjects committees of Harvard Medical School and the University of Michigan both approved these recruitment and consent procedures. The NCS-R interview was administered in two parts. Part 1 included a core diagnostic assessment administered to all respondents. Part 2 included questions about correlates and additional disorders administered to all part 1 respondents who met lifetime criteria for any core disorder plus a probability subsample of 5,692 other respondents. Separation anxiety disorder was included in part 2. The sample was weighted to be representative of the U.S. adult population. Details on NCS-R weighting are reported elsewhere (17) .
Childhood and Adult Separation Anxiety Disorder
The retrospective assessment of childhood separation anxiety disorder in the NCS-R was based on an expansion of the separation anxiety disorder module in the Diagnostic Interview Schedule for DSM-IV (19) . The respondents were classified as having had childhood separation anxiety disorder if they endorsed at least three of the eight DSM-IV criterion A symptoms for separation anxiety disorder, indicating that these symptoms were present for at least 1 month at some time before age 18, and the subjects reported clinically significant distress or role impairment. The respondents who met criteria for childhood separation anxiety disorder were asked about both age of onset and persistence into adulthood. A parallel set of symptom, age of onset, and recency questions were also asked about adult-onset separation anxiety disorder, making age-appropriate modifications to the criterion A symptom questions. The separation anxiety disorder symptom questions closely resemble those in the Structured Clinical Interview for Separation Anxiety Symptoms (2) , an instrument with good psychometric properties that was developed for use with clinical groups of adults. However, no independent clinical evaluation was made of the separation anxiety disorder section of the NCS-R interview, which means that the validity of this assessment is unknown.
Comorbid DSM-IV Disorders
Other DSM-IV disorders were assessed in the NCS-R with version 3.0 of the World Health Organization’s (WHO) Composite International Diagnostic Interview (CIDI) (20) , a fully structured, lay-administered diagnostic interview. The core lifetime CIDI disorders include other anxiety disorders (panic disorder with or without agoraphobia, generalized anxiety disorder, specific phobia, social phobia, agoraphobia without panic disorder, obsessive-compulsive disorder, and posttraumatic stress disorder), mood disorders (major depressive disorder, bipolar I or II disorder, and dysthymic disorder), impulse-control disorders (oppositional-defiant disorder, conduct disorder, attention deficit hyperactivity disorder, and intermittent explosive disorder), and substance use disorders (alcohol and illicit drug abuse and dependence). Organic exclusion rules and diagnostic hierarchy rules were used in making diagnoses. Separation anxiety disorder was not included in operationalizing the hierarchy rules. As detailed elsewhere (21) , blinded clinical reinterviews with the Structured Clinical Interview for DSM-IV (SCID) (22) with a probability subsample of NCS-R respondents revealed generally good concordance between DSM-IV diagnoses of anxiety, mood, and substance disorders based on the CIDI and the blinded SCID clinical reappraisal interviews, with areas under the curve in the range 0.65 to 0.81. Diagnoses of impulse-control disorders and separation anxiety disorder were not validated because the SCID does not include assessments of these disorders.
Other Correlates of Childhood and Adult Disorders
Three other sets of possible correlates of separation anxiety disorder were also examined: sociodemographic characteristics, role impairment, and treatment. Sociodemographic characteristics included gender, age in years (18–29, 30–44, 45–59, or 60+), race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), education in years (0–11, 12, 13–15, and 16+), marital status (married or cohabitating, previously married, or never married), and employment status (employee, student, homemaker, retiree, or other). Role impairment among 12-month cases was assessed with the Sheehan Disability Scale (23) . This scale asked respondents to focus on the 1 month in the past year when their separation anxiety disorder was most severe and to rate how much separation anxiety disorder interfered with their home management, work, social life, and personal relationships on a visual analogue scale (range=0–10) of none (0), mild (1–3), moderate (4–6), severe (7–9), and very severe (10) interference. Treatment was assessed in two places: in each diagnostic section, where the authors asked about treatment of the focal disorder, and in a separate section on overall treatment, where the authors asked about treatment of any problem with emotions, nerves, or mental health. A comparison of responses to the more and less inclusive questions allowed us to distinguish respondents with separation anxiety disorder who received mental health treatment that did not focus on separation anxiety disorder from those who received treatment for separation anxiety disorder.
Statistical Analysis
The actuarial method was used to generate age-of-onset distributions from retrospective age-of-onset reports. Associations of separation anxiety disorder assessments with sociodemographic variables and comorbid conditions were estimated with bivariate logistic regression analysis with coefficients exponentiated and reported as odds ratios for ease of interpretation. Bivariate rather than multivariate logistic regression was used because our goal was to be descriptive rather than to make causal inferences. Impairment and treatment were examined with simple cross-tabulations. Because the NCS-R data are weighted and clustered, all statistical analyses used the Taylor series linearization method (24) implemented in the SUDAAN software system (25) . Significance tests of sets of coefficients were made with Wald chi-square tests based on SUDAAN coefficient variance-covariance matrices. Statistical significance was evaluated with two-tailed tests (p<0.05).
Results
Prevalence, Age of Onset, and Persistence
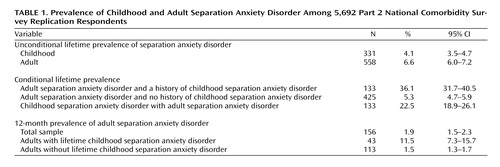
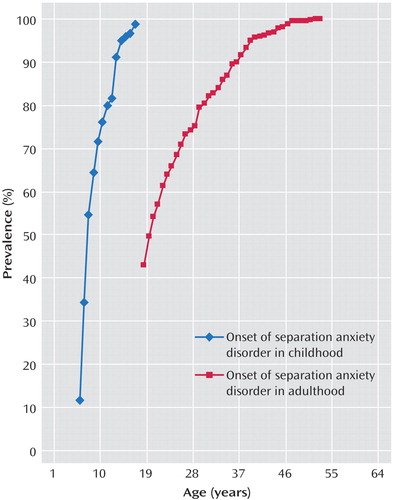
Lifetime prevalence estimates of childhood and adult separation anxiety disorder were 4.1% and 6.6%, respectively ( Table 1 ). The 12-month prevalence estimate of adult separation anxiety disorder was 1.9%. Somewhat more than one-third (36.1%) of the respondents classified in the NCS-R as childhood cases had disorders that persisted into adulthood and 11.5% into the 12 months before the interview. The respondents classified as childhood cases represented 22.5% of all those classified as lifetime cases of adult separation anxiety disorder and 24.8% (N=43) of those classified as 12-month adult cases, indicating that the majority of the NCS-R respondents classified as both lifetime (N=425, 77.5%) and 12-month (N=133, 75.2%) adult cases had first onset in adulthood. Analysis of age-of-onset curves ( Figure 1 ) shows that the majority of the respondents classified as childhood cases began their illnesses in early or middle childhood. The majority of the respondents classified as adult-onset cases, in comparison, began in the late teens or early 20s, with 80% (N=449) of the first onsets occurring by age 30.
Sociodemographic Correlates
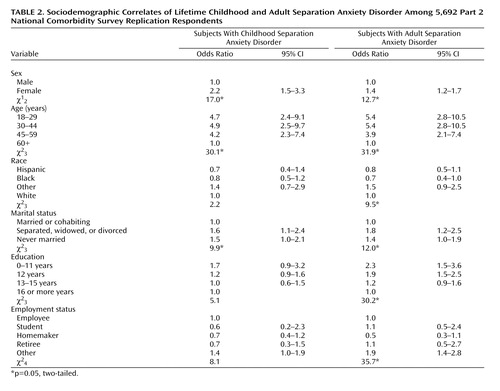
Lifetime child and adult separation anxiety disorders, as assessed by the NCS-R, were significantly more common among women than men, with odd ratios of 2.2 (children) and 1.4 (adults) ( Table 2 ). The odds of lifetime estimated separation anxiety disorder were also substantially higher among respondents in the age range of 18–59 years than in those 60+, with odds ratios in the range of 4.2–4.9 for children and 3.9–5.4 for adults with estimated separation anxiety disorder. Unmarried people (both those never married and those previously married) also had somewhat higher odds of both estimated child (odds ratios: range=1.5–1.6) and adult (odds ratios: range=1.4–1.8) separation anxiety disorder than people who were married or cohabiting. Adult, but not childhood, assessments of separation anxiety disorder were significantly related to low education (0–12 years), with odds ratios of 1.9–2.3, and to “other” employment status (a category made up mostly of unemployed and disabled individuals), with an odds ratio of 1.9.
Comorbidity With Other DSM-IV Disorders
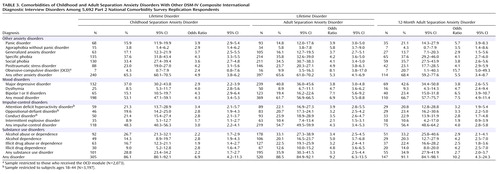
The vast majority of respondents classified in the NCS-R as having either childhood separation anxiety disorder (N=305, 86.1%) or adult separation anxiety disorder (88.5%) had a history of at least one of the other DSM-IV disorders assessed in the survey ( Table 3 ). The strength of comorbidities, as indicated by odds ratios, did not differ markedly in magnitude between estimated childhood separation anxiety disorder (with a median odds ratio of 2.9 and an interquartile range of odds ratios of 2.2–4.0) and adult separation anxiety disorder (median odds ratio of 3.9 and an interquartile range of 3.4–5.0). Moreover, the strength of comorbidity between estimated separation anxiety disorder and other anxiety disorders (odds ratios: range=4.9–5.3) was not markedly different from the strength of comorbidities with mood disorders (odds ratios: range=4.3–7.5), although they were somewhat higher than comorbidities with impulse-control disorders (odds ratios: range=3.0–4.3) and substance use disorders (odds ratios: range=2.2–3.3).
Functional Impairment
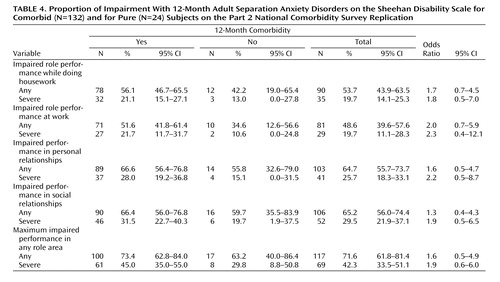
More than 40% of the respondents classified as having 12-month separation anxiety disorder (N=69) reported severe impairment in at least one of the life domains assessed by the Sheehan Disability Scale ( Table 4 ). Severe impairment was especially common in the domains of social and personal life. Not surprisingly, comorbidity was associated with impairment. Nonetheless, a meaningful proportion (29.8%) of the respondents classified as having 12-month separation anxiety disorder in the absence of any other NCS-R or DSM-IV disorder (i.e., pure 12-month separation anxiety disorder) reported severe impairment in role functioning.
Treatment
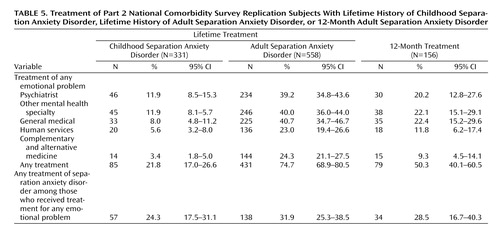
Only about one-fifth (21.8%) of the respondents with estimated childhood separation anxiety disorder reported receiving treatment for emotional problems before age 18. Most were seen by a mental health specialist ( Table 5 ). Less than one-fourth of these patients (24.3%), however, reported that separation anxiety disorder was a focus of treatment. A much higher percentage of respondents with estimated adult separation anxiety disorder (74.7%), in comparison, reported receiving treatment for emotional problems, with the highest proportions seen by a psychiatrist, some other mental health professional, or a primary care physician. Less than one-third of these adult patients (31.9%), however, reported that separation anxiety disorder was ever a focus of treatment. Approximately half (50.3%) of the respondents classified as having separation anxiety disorder in the 12 months before the interview received 12 months of treatment for emotional problems, but less than one-third of these patients (28.5%) reported that separation anxiety disorder was a focus of treatment.
Discussion
Two limitations of the study are noteworthy. First, the potentially distorting influence of retrospective recall bias cannot be ruled out in interpreting reports about childhood separation anxiety disorder. Second, diagnoses were based on unvalidated fully structured interviews administered by lay interviewers rather than by clinical interviewers. This could be an especially important limitation for a disorder such as separation anxiety disorder, in which clinical judgment may be needed to determine whether the degree of anxiety about separation from an attachment figure truly is excessive in relation to the respondent’s life situation or developmental phase or if the symptoms are better explained by another mental disorder. Because of these limitations, these results should be considered provisional. Within the context of these limitations, to our knowledge, we presented the first nationally representative data on the descriptive epidemiology of adult separation anxiety disorder. The 4.1% estimated prevalence of childhood separation anxiety disorder is similar to previously published estimates (26) . However, contrary to suggestions in DSM-IV-TR, the estimated lifetime prevalence of adult separation anxiety disorder (6.6%) was higher than the estimated lifetime prevalence of childhood separation anxiety disorder. In addition, the vast majority of respondents classified as having adult separation anxiety disorder reported first onset in adulthood rather than childhood, even though a substantial proportion of the respondents classified as childhood cases persisted into adulthood. These results call into question DSM-IV-TR representation of adult separation anxiety disorder. The NCS-R finding that estimated separation anxiety disorder is more prevalent among women than men is consistent with previous research on childhood separation anxiety disorder (11 , 12 , 26 , 27) . That the female-male odds ratio is lower for estimated adult (1.4) than childhood (2.2) cases could mean either that persistence into adulthood is higher for males than females or that males are more likely than females to have first onset in adulthood. More detailed analyses (results not shown) found that only the latter process is at work. The finding that estimated adult separation anxiety disorder is associated with roughly doubling of the odds of low (0–12 years) education, unemployment, and marital disruption is consistent with the suggestion in the clinical literature that separation anxiety disorder can be seriously impairing, although temporal and causal priority were not sorted out in the cross-sectional analyses of these sociodemographic correlates. The odds of being not married are elevated among both respondents with estimated childhood separation anxiety disorder and those with estimated adult separation anxiety disorder. This result indirectly suggests that estimated childhood separation anxiety disorder might be a risk marker for subjects remaining unmarried and, once married, for marital instability. Education and occupation, in comparison, were related to estimated adult separation anxiety disorder but not to estimated childhood separation anxiety disorder. The failure to find an association of estimated childhood separation anxiety disorder with these core indicators of socioeconomic status differs from the consistent finding in child epidemiological studies that separation anxiety disorder is strongly related to low parental socioeconomic status (26) . The finding that both estimated childhood and estimated adult separation anxiety disorder are strongly comorbid with many other DSM-IV disorders is consistent with a broader pattern of high comorbidity in the NCS-R (28) and other epidemiological surveys (29) . The finding that the odds ratios of estimated separation anxiety disorders with other anxiety disorders are no higher than with mood disorders and somewhat higher than with impulse-control and substance use disorders is consistent with the existence of a broad internalizing-externalizing distinction in the comorbidity of mental disorders (28 , 30–32) . Methodological studies are needed to investigate whether comorbidities involving separation anxiety disorder are because of overlapping symptoms, imprecision of diagnostic criteria, or other methodological confounders. To the extent that such confounders can be ruled out, studies could profitably address whether these comorbidities are causal and, if so, whether early successful treatment of separation anxiety disorder in childhood and early adulthood would lower the rates of secondary adult disorders. A related question is whether adult separation anxiety disorder has any effect on the persistence or severity of other comorbid disorders. Because high comorbidity is generally found to be significantly associated with impairment (28) , it is not surprising that nearly half of the respondents estimated to have 12-month adult separation anxiety disorder experienced severe role impairment if they have comorbid conditions. The fact that more than one-fourth of the respondents with pure 12-month estimated separation anxiety disorder also reported severe role impairment, though, suggests that separation anxiety disorder can also be impairing in itself. Because this is the case, the question arises whether comorbid separation anxiety disorder accounts for some of the impairment previously attributed to other anxiety (33 – 41) , mood (42 – 45) , or substance use (46) disorders. None of the many studies that estimated the societal costs of these conditions included separation anxiety disorder as a possible contributor to impairment. The finding that less than one-fourth of the children with estimated separation anxiety disorder receive treatment is consistent with research that documents substantial undertreatment of children with internalizing disorders (47) . Treatment of adults with estimated separation anxiety disorder is dramatically higher (74.7%). However, the vast majority of patients reported that they were treated for comorbid conditions rather than for separation anxiety disorder. These results suggest that treatment providers often fail to recognize separation anxiety disorder in the context of other comorbid conditions. The absence of research on the treatment of adult separation anxiety disorder suggests that researchers have also largely overlooked this disorder. The NCS-R profile of nontrivial prevalence and impairment in the context of low treatment raises the question of whether detection and treatment of separation anxiety disorder in usual clinical practice are adequate. However, given that there was no clinical validation of the NCS-R separation anxiety disorder interview, it is possible that these data include false positives. Thus, before drawing firm conclusions or embarking on treatment studies, it would be important to carry out phenomenological and psychometric studies to refine the criteria for adult separation anxiety disorder and to confirm its prevalence and consequences. As noted in the introduction, current DSM criteria focus on the childhood disorder. It might be that the criteria could be usefully modified for adults, especially because the authors have evidence that most lifetime cases have first onset in adulthood. In considering the possible revision of diagnostic criteria for adults, it would be useful to focus on issues of symptom overlap and differential diagnosis with a number of the disorders included in this article, as well as with several other potentially related conditions (e.g., adjustment disorder, cluster C personality disorders). This is especially important in light of the fact that the vast majority of NCS-R respondents with 12-month estimated adult separation anxiety disorder (91.1%) were classified as meeting criteria for at least one other 12-month DSM-IV disorder. In further study, it would be important to explore the boundaries between normal response to loss of an attachment figure, separation anxiety as an adjustment reaction, and syndromal separation anxiety disorder. Given that infant separation anxiety is one of the most strongly conserved behaviors in evolution (48 – 50) and given the importance of attachment relationships in adulthood, separation anxiety may be more easily elicited in adults than is commonly recognized and might be the norm under certain extreme life circumstances. Thus, it would make sense that diagnostic criteria take into consideration the possibility of expected reactions to extreme life stressors that create unusual but realistic interpersonal threats (e.g., living in a very dangerous neighborhood or a war zone, caring for a seriously ill child). In addition, as adult separation anxiety disorder becomes better understood, it would be valuable for the DSM criteria to provide assistance in distinguishing transient context-dependent separation anxiety symptoms or mild adaptive forms related to culturally accepted familial interdependence from a full-fledged pathological separation anxiety syndrome in need of treatment. The diagnosis of adjustment disorder with anxious mood is currently used in children when there are subthreshold, transient symptoms of separation anxiety. Consideration should be given as to when this should apply to adults as well. Once diagnostic criteria are clarified, it would be useful to carry out analytic epidemiological investigations to examine the many risk factors that might differ in predicting first onset in childhood versus adulthood and persistence of childhood cases into adulthood. Our superficial analysis of sociodemographic correlates already turned up potentially interesting specifications (e.g., stronger associations of socioeconomic status with adult than childhood estimated cases). A thorough investigation of similarities and differences across a wide range of risk factors would be enlightening. Comorbidity might also be a focus of risk factor analysis. For example, a growing literature documents that parental overprotection and control are risk factors for a wide range of childhood anxiety disorders (51 , 52) . It would be useful to investigate the extent to which these parenting styles account for the comorbidity of separation anxiety disorder with other anxiety and mood disorders, as well as the specific role of parental behavior in contributing to vulnerability to separation anxiety disorder. Such risk factor research could play a role in elaborating a conceptual model of separation anxiety disorder in relation to other internalizing disorders and might help elucidate factors that contribute to adult onset and/or persistence of syndromal or subthreshold separation anxiety disorder from childhood into adulthood. Such insights would inform the treatment development work needed to establish effective preventive and clinical interventions for this disorder.
Acknowledgments
Collaborating National Comorbidity Survey Replication investigators include Ronald C. Kessler (principal investigator, Harvard Medical School), Kathleen Merikangas (co-principal investigator, NIMH), James Anthony (Michigan State University), William Eaton (Johns Hopkins University), Meyer Glantz (National Institute on Drug Abuse), Doreen Koretz (Harvard University), Jane McLeod (Indiana University), Mark Olfson (Columbia University College of Physicians and Surgeons), Harold Pincus (University of Pittsburgh), Greg Simon and Michael Von Korff (Group Health Cooperative), Philip Wang (Harvard Medical School), Kenneth Wells (UCLA), Elaine Wethington (Cornell University), and Hans-Ulrich Wittchen (Max Planck Institute of Psychiatry). A complete list of National Comorbidity Survey publications and the full text of all NCS-R instruments can be found at http://www.hcp.med.harvard.edu/ncs. The NCS-R is carried out in conjunction with the WHO World Mental Health Survey Initiative. A complete list of World Mental Health publications can be found at http://www.hcp.med.harvard.edu/wmhcidi.
1. Ollendick TH, Lease CA, Cooper C: Separation anxiety in young adults: a preliminary examination. J Anxiety Disord 1993; 7:293–305Google Scholar
2. Cyranowski JM, Shear MK, Rucci P, Fagiolini A, Frank E, Grochocinski VJ, Kupfer DJ, Banti S, Armani A, Cassano G: Adult separation anxiety: psychometric properties of a new structured clinical interview. J Psychiatr Res 2002; 36:77–86Google Scholar
3. Fagiolini A, Shear MK, Cassano GB, Frank E: Is lifetime separation anxiety a manifestation of panic spectrum? CNS Spectr 1998; 3:63–72Google Scholar
4. Manicavasagar V, Silove D, Curtis J: Separation anxiety in adulthood: a phenomenological investigation. Compr Psychiatry 1997; 38:274–282Google Scholar
5. Manicavasagar V, Silove D: Is there an adult form of separation anxiety disorder? a brief clinical report. Aust NZ J Psychiatry 1997; 31:299–303Google Scholar
6. Wijeratne C, Manicavasagar V: Separation anxiety in the elderly. J Anxiety Disord 2003; 17:695–702Google Scholar
7. Hock E, McBride S, Gnezda M: Maternal separation anxiety: mother-infant separation from the maternal perspective. Child Dev 1989; 60:793–802Google Scholar
8. Diener ML, Kim D-Y: Maternal and child predictors of preschool children’s social competence. J Appl Dev Psychol 2004; 25:3–24Google Scholar
9. Mayseless O, Scher A: Mother’s attachment concerns regarding spouse and infant’s temperament as modulators of maternal separation anxiety. J Child Psychol Psychiatry 2000; 41:917–925Google Scholar
10. Scher A, Blumberg O: Night waking among 1-year-olds: a study of maternal separation anxiety. Child Care Health Dev 1999; 25:323–334Google Scholar
11. Foley DL, Pickles A, Maes HM, Silberg JL, Eaves LJ: Course and short-term outcomes of separation anxiety disorder in a community sample of twins. J Am Acad Child Adolesc Psychiatry 2004; 43:1107–1114Google Scholar
12. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A: Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003; 60:837–844Google Scholar
13. Deltito JA, Hahn R: A three-generational presentation of separation anxiety in childhood with agoraphobia in adulthood. Psychopharmacol Bull 1993; 29:189–193Google Scholar
14. Manicavasagar V, Silove D, Curtis J, Wagner R: Continuities of separation anxiety from early life into adulthood. J Anxiety Disord 2000; 14:1–18Google Scholar
15. Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M: Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 1993; 50:565–576Google Scholar
16. Kessler RC, Merikangas KR: The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res 2004; 13:60–68Google Scholar
17. Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell B-E, Walters EE, Zaslavsky A, Zheng H: The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res 2004; 13:69–92Google Scholar
18. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Google Scholar
19. Robins LN, Cottler L, Bucholtz K, Compton W: National Institute of Mental Health Diagnostic Interview Schedule, version IV (DIS-IV). St Louis, Washington University, Department of Psychiatry, 1997Google Scholar
20. Kessler RC, Ustun TB: The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004; 13:93–121Google Scholar
21. Kessler RC, Berglund PA, Demler O, Jin R, Walters EE: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry 2005; 62:593–602Google Scholar
22. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP). New York, New York State Psychiatric Institute, Biometrics Research, 2002Google Scholar
23. Leon AC, Olfson M, Portera L, Farber L, Sheehan DV: Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med 1997; 27:93–105Google Scholar
24. Wolter KM: Introduction to Variance Estimation. New York, Springer-Verlag, 1985Google Scholar
25. Research Triangle Institute: SUDAAN: Professional Software for Survey Data Analysis. Research Triangle Park, NC, Research Triangle Institute, 2002Google Scholar
26. Masi G, Mucci M, Millepiedi S: Separation anxiety disorder in children and adolescents: epidemiology, diagnosis and management. CNS Drugs 2001; 15:93–104Google Scholar
27. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA: Adolescent psychopathology, I: prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol 1993; 102:133–144Google Scholar
28. Kessler RC, Chiu WT, Demler O, Walters EE: Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry 2005; 62:617–627Google Scholar
29. Robins LN, Locke BZ, Regier DA: An overview of psychiatric disorders in America, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 328–366Google Scholar
30. Krueger RF: The structure of common mental disorders. Arch Gen Psychiatry 1999; 56:921–926Google Scholar
31. Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J: A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol 2003; 112:437–447Google Scholar
32. Kendler KS, Gallagher TJ, Abelson JM, Kessler RC: Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample: the National Comorbidity Survey. Arch Gen Psychiatry 1996; 53:1022–1031Google Scholar
33. Goodwin R, Lipsitz JD, Chapman TF, Mannuzza S, Fyer AJ: Obsessive-compulsive disorder and separation anxiety comorbidity in early-onset panic disorder. Psychol Med 2001; 31:1307–1310Google Scholar
34. Lipsitz JD, Martin LY, Mannuzza S, Chapman TF, Liebowitz MR, Klein DF, Fyer AJ: Childhood separation anxiety disorder in patients with adult anxiety disorders. Am J Psychiatry 1994; 151:927–929Google Scholar
35. Manicavasagar V, Silove D, Hadzi-Pavlovic D: Subpopulations of early separation anxiety: relevance to risk of adult anxiety disorders. J Affect Disord 1998; 48:181–190Google Scholar
36. Otto MW, Pollack MH, Maki KM, Gould RA, Worthington JJ III, Smoller JW, Rosenbaum JF: Childhood history of anxiety disorders among adults with social phobia: rates, correlates, and comparisons with patients with panic disorder. Depress Anxiety 2001; 14:209–213Google Scholar
37. Perugi G, Deltito J, Soriani A, Musetti L, Petracca A, Nisita C, Maremmani I, Cassano GB: Relationships between panic disorder and separation anxiety with school phobia. Compr Psychiatry 1988; 29:98–107Google Scholar
38. Aschenbrand SG, Kendall PC, Webb A, Safford SM, Flannery-Schroeder E: Is childhood separation anxiety disorder a predictor of adult panic disorder and agoraphobia? a seven-year longitudinal study. J Am Acad Child Adolesc Psychiatry 2003; 42:1478–1485Google Scholar
39. Hayward C, Wilson KA, Lagle K, Killen JD, Taylor CB: Parent-reported predictors of adolescent panic attacks. J Am Acad Child Adolesc Psychiatry 2004; 43:613–620Google Scholar
40. Nestadt G, Addington A, Samuels J, Liang KY, Bienvenu OJ, Riddle M, Grados M, Hoehn-Saric R, Cullen B: The identification of OCD-related subgroups based on comorbidity. Biol Psychiatry 2003; 53:914–920Google Scholar
41. Otto MW, Pollack MH, Rosenbaum JF, Sachs GS, Asher RH: Childhood history of anxiety in adults with panic disorder: association with anxiety sensitivity and comorbidity. Harv Rev Psychiatry 1994; 1:288–293Google Scholar
42. Hong JP, Samuels J, Bienvenu OJ III, Cannistraro P, Grados M, Riddle MA, Liang KY, Cullen B, Hoehn-Saric R, Nestadt G: Clinical correlates of recurrent major depression in obsessive-compulsive disorder. Depress Anxiety 2004; 20:86–91Google Scholar
43. Noyes R Jr, Lyle Stuart S, Langbehn DR, Happel RL, Longley SL, Yagla SJ: Childhood antecedents of hypochondriasis. Psychosomatics 2002; 43:282–289Google Scholar
44. Tillman R, Geller B, Bolhofner K, Craney JL, Williams M, Zimerman B: Ages of onset and rates of syndromal and subsyndromal comorbid DSM-IV diagnoses in a prepubertal and early adolescent bipolar disorder phenotype. J Am Acad Child Adolesc Psychiatry 2003; 42:1486–1493Google Scholar
45. Wilhelm K, Boyce P, Brownhill S: The relationship between interpersonal sensitivity, anxiety disorders and major depression. J Affect Disord 2004; 79:33–41Google Scholar
46. Vance A, Harris K, Boots M, Talbot J, Karamitsios M: Which anxiety disorders may differentiate attention deficit hyperactivity disorder, combined type, with dysthymic disorder from attention deficit hyperactivity disorder, combined type alone? Aust NZ J Psychiatry 2003; 37:563–569Google Scholar
47. Wang PS, Berglund PA, Olfson M, Pincus HA, Wells KB, Kessler RC: Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry 2005; 62:603–613Google Scholar
48. Polan HJ, Hofer MA: Olfactory preference for mother over home nest shavings by newborn rats. Dev Psychobiol 1998; 33:5–20Google Scholar
49. Polan HJ, Hofer MA: Maternally directed orienting behaviors of newborn rats. Dev Psychobiol 1999; 34:269–279Google Scholar
50. Polan HJ, Milano D, Eljuga L, Hofer MA: Development of rats’ maternally directed orienting behaviors from birth to day 2. Dev Psychobiol 2002; 40:81–103Google Scholar
51. Rapee RM: Potential role of childrearing practices in the development of anxiety and depression. Clin Psychol Rev 1997; 17:47–67Google Scholar
52. Wood JJ, McLeod BD, Sigman M, Hwang W-C, Chu BC: Parenting and childhood anxiety: theory, empirical findings, and future directions. J Child Psychol Psychiatry 2003; 44:134–151Google Scholar