Trauma, PTSD, and Substance Use Disorders: Findings From the Australian National Survey of Mental Health and Well-Being
Abstract
Objective: The aim of the present study was to examine the association between trauma and posttraumatic stress disorder (PTSD) and substance use disorders and to examine the correlates of substance use disorder plus PTSD comorbidity in the Australian general population. Method: Data were collected from a stratified sample of 10,641 participants as part of the Australian National Survey of Mental Health and Well-Being. A modified version of the Composite International Diagnostic Interview was used to determine the presence of DSM-IV anxiety, affective, and substance use disorders and ICD-10 personality disorders. Results: Substance use disorder plus PTSD was experienced by a significant minority of the Australian general population (0.5%). Among those with PTSD, the most common substance use disorder was an alcohol use disorder (24.1%), whereas among those with a substance use disorder, PTSD was most common among individuals with an opioid use disorder (33.2%). Consistent with U.S. clinical literature, individuals with substance use disorder plus PTSD experience significantly poorer physical and mental health and greater disability than those with substance use disorder alone. In contrast, individuals with PTSD alone and those with substance use disorder plus PTSD shared a remarkably similar clinical profile. Conclusions: It is important that individuals entering treatment for substance use disorder or PTSD be assessed for this comorbidity. The addition of either disorder may present complications that need to be considered for the provision of appropriate treatment. Further research is necessary to ascertain which treatments are most effective in treating comorbid substance use disorder plus PTSD.
There is a growing epidemiological and clinical literature documenting the frequent co-occurrence of substance use disorders and posttraumatic stress disorder (PTSD). For example, the National Comorbidity Survey (1) found that men with an alcohol or other drug use disorder were 2.06 and 2.97 times more likely than those without an alcohol or another drug use disorder to have co-occurring PTSD, respectively. Among women, the odds of having co-occurring PTSD in the presence of an alcohol or other drug use disorder were 2.48 and 4.46, respectively (1) . The likelihood of these two disorders co-occurring in the Australian population were found to be even higher (2) . Analysis of the National Survey of Mental Health and Well-Being found that men with an alcohol use disorder were 6.6 times more likely to have co-occurring PTSD than men without an alcohol use disorder, and men with a drug use disorder were 7.2 times more likely than men without a drug use disorder to have co-occurring PTSD. These odds for women were 4.5 and 12.4, respectively (2) .
Despite the frequent co-occurrence, much remains to be understood about this comorbidity. Specifically, although existing analyses have identified the association between alcohol and other drug use disorders and PTSD (1 , 2) , there is little epidemiological information regarding the association between PTSD and particular substances. The analysis of the Epidemiological Catchment Area (ECA) data by Cottler et al. (3) found that individuals who had ever used cocaine or opiates were at particular risk of trauma exposure (odds ratio=5.06) and PTSD (odds ratio=3.62) compared to those who had never used cocaine or opiates (3) . It is likely that these associations would be even stronger among those who use substances at problematic levels; however, this has not yet been examined.
There is also a notable lack of epidemiological research focusing explicitly on the interrelationships between these two disorders (4) , the demographic correlates of this comorbidity, or its impact on physical and mental health and disability. Existing clinical evidence indicates that substance use disorder plus PTSD may be associated with poorer physical and psychological health and poorer functioning (5 – 8) compared to those with either disorder alone. However, because these studies have been limited to clinical groups of those in treatment for either disorder, they may be subject to self-selection or referral bias (9) . Epidemiological examination of the factors associated with substance use disorder plus PTSD would add considerably to understanding this comorbidity. Achieving a better understanding of this comorbidity is particularly important given its association with poorer treatment outcomes (10) .
With data collected from the Australian general population, the present study aimed to
Examine the prevalence of trauma and PTSD among individuals with alcohol, cannabis, sedative, amphetamine, and opioid use disorders;
Examine the strength of the association among trauma, PTSD, alcohol, cannabis, sedative, amphetamine, and opioid use disorders;
Examine the demographic, physical, and mental health correlates of substance use disorder plus PTSD and the disability associated with this comorbidity.
Method
Procedure
The present study used data collected as part of the Australian National Survey of Mental Health and Well-Being conducted in 1997 by the Australian Bureau of Statistics. Participants were recruited from private dwellings (e.g., houses, home units, trailers, tents) in all states and territories of Australia and selected by using random stratified multistage sampling. Of the 13,600 private dwellings approached, 10,641 people agreed to participate, representing a 78% response rate. After a complete description of the study was given to the subjects, written informed consent was obtained. The study was weighted according to the inverse probability of an individual being selected for an interview. A more detailed account of the sampling design used has been reported elsewhere (11) . Interviews were conducted in person, and responses were recorded on a laptop computer.
Structured Questionnaire
A structured questionnaire was administered with sections addressing demographic characteristics, neuroticism, the presence of chronic health conditions, psychiatric disorders, suicidal ideation, disability, days out of role, and general psychological morbidity (11) .
Neuroticism was measured by using the Eysenck Personality Questionnaire (12) . General physical and mental health were measured by using the 12-Item Short-Form Health Survey Questionnaire, in which lower scores indicate poorer health (population mean=50, SD=10) (13) . Chronic health conditions included self-reported asthma, bronchitis, anemia, high blood pressure, heart trouble, arthritis, kidney disease, diabetes, cancer, stomach or duodenal ulcer, liver or gallbladder trouble, and hernia or rupture. The participants were assessed for 12-month DSM-IV diagnoses of anxiety (panic disorder, agoraphobia, social phobia, generalized anxiety disorder, obsessive-compulsive disorder, and posttraumatic stress disorder PTSD), affective disorder (depression, dysthymia, mania, hypomania, and bipolar disorder), and substance use disorders (abuse and dependence) by using a modified version of the Composite International Diagnostic Interview, version 2.1 (14) , and screened for ICD-10 personality disorders (paranoid, schizoid, impulsive, borderline, histrionic, narcissistic, anxious, and dependent).
The PTSD module began by eliciting events that may have occurred during the participants’ lifetimes. The participants were asked to indicate whether or not they had experienced combat, natural disasters, or life-threatening accidents; witnessed serious injury or death; had been raped, sexually molested, threatened with a weapon, tortured, or the victim of terrorists; or experienced any other extremely stressful or upsetting event or a great shock because one of the aforementioned events happened to someone close. If the response to either of those questions was “yes,” a description of the event was obtained. Responses to the latter two events were coded according to DSM-IV guidelines as to whether these events qualified under criterion A1. If a participant endorsed multiple events, he or she was asked to specify the event that he or she considered to be most traumatic. The remainder of the PTSD module was administered with reference to that event to determine a current diagnosis.
Analyses
Prevalence estimates were weighted to conform to independent population estimates by state, part of the state, age, and sex. In addition, balanced repeated replicate weights were used to account for the complex survey sampling design. Prevalence estimates and their standard errors were calculated by using SUDAAN version 8.0 (Research Triangle Institute, Research Triangle Park, N.C.). Inferential tests were conducted on unweighted data by using SAS version 8.02 (SAS Institute, Cary, N.C.).
A series of logistic, linear, and Poisson regressions were performed to examine the association between trauma, PTSD, and particular substance use disorders and the correlates of substance use disorder plus PTSD comorbidity. Analyses of the association between trauma, PTSD, and substance use disorders were controlled for age and sex. Analyses of the physical and mental health correlates and disability associated with substance use disorder plus PTSD were controlled for potentially confounding factors, including demographic characteristics (i.e., age, sex, marital status, schooling, and main source of income) and neuroticism. These variables were found to be associated with substance use disorder/PTSD status in univariate analysis and have been shown to be associated with the outcome variables in a previous analysis of the National Survey of Mental Health and Well-Being (15) . Results of logistic regressions were reported as odds ratios with 95% confidence intervals (CIs). Results of Poisson regressions are reported as risk ratios (i.e., the exponent of the regression coefficient) with 95% CIs. All tests conducted were two-tailed with a predetermined alpha level of 0.05. All regression models reported reached significance at p<0.001.
Results
Prior analysis of the survey has shown that in the preceding 12 months, 1.3% of the population met DSM-IV criteria for PTSD (weighted N=180,802), and 7.9% met criteria for a substance use disorder (weighted N=1,061,081) (11) . Six percent had an alcohol use disorder (weighted N=813,637), 2.2% had a cannabis use disorder (weighted N=302,246), 0.5% had a sedative use disorder (weighted N=64,976), 0.4% had an amphetamine use disorder (weighted N=46,917), and 0.3% had an opioid use disorder (weighted N=38,922). It is important to note that 85% of the people with a substance use disorder had only one substance use disorder, and at best, the association between any substance use disorders was fair (kappas ranged from 0.03 to 0.31) (16) .
Substance Use Disorder and Trauma
High rates of trauma exposure were reported across all substance use disorders (more data are available online). After we controlled for age and sex, logistic regression analysis revealed that the greatest likelihood of trauma exposure was associated with sedatives (92.8% versus 56.7%) (odds ratio=7.94, 95% CI=3.16–19.97), amphetamines (91.0% versus 56.8%) (odds ratio=7.47, 95% CI=2.36–25.84), and opioid use disorders (87.8% versus 56.8%) (odds ratio=5.58, 95% CI=1.96–15.95). Poisson regression showed that individuals with these disorders experienced a greater number of traumatic events than those who did not have these disorders. After we adjusted for age and sex in Poisson regression, those who had been exposed to trauma experienced an average of 2.38 more substance use disorders compared to those who were not exposed to trauma (0.12 versus 0.05) (risk ratio=2.38, 95% CI=2.05–2.78). The most common trauma types experienced by individuals with substance use disorders were having witnessed serious injury or death (40.5%), having been involved in a life-threatening accident (33.1%), and having been threatened with a weapon, having been held captive, or having been kidnapped (25.7%).
Prevalence of Substance Use Disorder Plus PTSD
Overall, 34.4% of those with PTSD also had a substance use disorder, most commonly an alcohol use disorder (24.1%). After we adjusted for age and sex in logistic regression, individuals with PTSD were 5.19 times more likely to have an alcohol use disorder (95% CI=3.51–7.67) ( Figure 1 ). After we adjusted for age and sex in Poisson regression, those with PTSD had an average 5.47 more substance use disorders than those without PTSD (1.6 versus 1.2) (risk ratio=5.47, 95% CI=4.39–6.82).
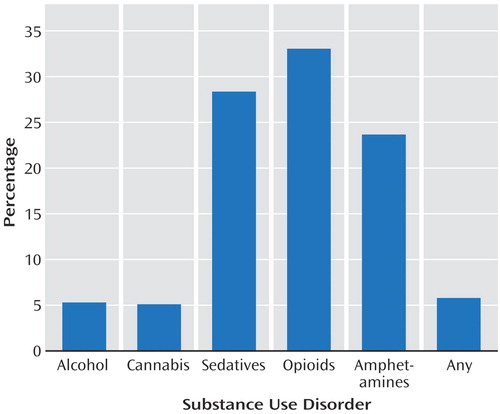
Of those with a substance use disorder, 5.9% had comorbid PTSD, making them 6.53 (95% CI=4.55–9.36) times more likely to receive a diagnosis of PTSD compared to those without a substance use disorder after we adjusted for age and sex in logistic regression. The highest prevalence of PTSD was found among those with an opioid use disorder (33.2%), followed by those with a sedative use disorder (28.5%). After we controlled for age and sex in logistic regression, the likelihood of having PTSD was highest among those with sedative (odds ratio=24.06, 95% CI=12.93–44.76) and opioid use disorders (odds ratio=23.54, 95% CI=10.49–52.81).
For 57.5% of those with both a substance use disorder and PTSD, their most traumatic event occurred before the onset of substance use disorder symptoms. In 8.7% of the cases, the event occurred simultaneous to the onset of substance use disorder symptoms, and for 33.8%, the symptoms of substance use disorder preceded the most traumatic event. Those with both a substance use disorder and PTSD were equally as likely to have chronic PTSD (i.e., PTSD lasting for more than 1 year) compared to those with PTSD alone (78.4% versus 75.1%).
Correlates of Substance Use Disorder Plus PTSD
To examine the relationship between substance use disorder and PTSD, the sample was divided into four groups:
Substance use disorder plus PTSD: participants diagnosed with both a substance use disorder and PTSD.
Substance use disorder alone: participants diagnosed with a substance use disorder who did not have PTSD.
PTSD alone: participants diagnosed with PTSD who did not have a substance use disorder.
Neither: participants who were not diagnosed with either a substance use disorder or PTSD.
Only a small proportion of the group had substance use disorder plus PTSD (0.5%), representing an estimated 62,183 Australian adults (more data are available online). An estimated 7.4% had a substance use disorder alone, 0.9% had PTSD alone, and 91.2% had neither a substance use disorder nor PTSD. The remaining analyses were based on comparisons between these groups.
Demographics
We present prevalence estimates for demographic correlates in each of the four groups (more data are available online). Those with substance use disorder plus PTSD were more likely to be men than those with PTSD alone (odds ratio=2.52, 95% CI=1.29–4.94) and were more likely to be between 18 and 34 years than those with neither disorder (odds ratio=2.93, 95% CI=1.73–4.97). The group with substance use disorder plus PTSD was less likely than all other groups to be in a married/de facto relationship (substance use disorder alone: odds ratio=0.50, 95% CI=0.26–0.94; PTSD alone: odds ratio=0.33, 95% CI=0.16–0.68; neither: odds ratio=0.19, 95% CI=0.10–0.35). There were no differences in level of educational attainment among the four groups. Those in the group with substance use disorder plus PTSD were more likely than those in the group with substance use disorder alone (odds ratio=4.63, 95% CI=2.61–8.23) and the group with neither (odds ratio=4.44, 95% CI=2.55–7.73) to derive their main source of income from a government allowance and less likely than all other groups to derive their main source of income from a wage or salary (substance use disorder alone: odds ratio=0.23, 95% CI=0.12–0.45; PTSD alone: odds ratio=0.41, 95% CI=0.19–0.86; neither: odds ratio=0.33, 95% CI=0.17–0.63).
Physical Health
After we adjusted for demographic characteristics and neuroticism in linear regression, substance use disorder/PTSD status was not associated with level of general physical health as measured by the 12-Item Short-Form Health Survey Questionnaire (substance use disorder plus PTSD: 44.0; substance use disorder alone: 49.3; PTSD alone: 45.1; neither: 48.9; t=1.85, df=3, p>0.05).
Sixty-one percent of those with substance use disorder plus PTSD reported at least one chronic health condition compared with 35% of those with substance use disorder alone, 41% of those with PTSD alone, and 39% of those with neither disorder. After we controlled for demographic characteristics and neuroticism in logistic regression, those with substance use disorder plus PTSD were more likely to report having a physical health condition than all other groups (substance use disorder alone: odds ratio=2.13, 95% CI=1.15–3.94; PTSD alone: odds ratio=2.38, 95% CI=1.15–4.92; neither: odds ratio=2.53, 95% CI=1.39–4.62). With a Poisson regression to control for demographic characteristics and neuroticism, those with substance use disorder plus PTSD were found to have a greater number of physical health conditions than those with substance use disorder alone (risk ratio=0.68, 95% CI=0.53–0.88), PTSD alone (risk ratio=0.71, 95% CI=0.52–0.98), or neither disorder (risk ratio=0.65, 95% CI=0.51–0.83).
Mental Health
General mental health
PTSD status was significantly associated with level of general mental health as measured by the 12-Item Short-Form Health Survey Questionnaire (substance use disorder plus PTSD: 35.1; substance use disorder alone: 46.9; PTSD alone: 37.4; neither: 52.4; t=12.59, df=3, p<0.001). After we adjusted for demographic characteristics and neuroticism, linear regression revealed that those with substance use disorder plus PTSD had significantly poorer general mental health than those with substance use disorder alone (mean difference=–7.86, 95% CI=–9.40 to –6.31), PTSD alone (mean difference=–1.91, 95% CI=–2.51 to –1.30), or neither disorder (mean difference=–7.89, 95% CI=–9.98 to –5.81).
Comorbid affective, anxiety, and personality disorders
Almost two-thirds of those in the group with substance use disorder plus PTSD and the group with PTSD alone had a comorbid affective disorder, and approximately half in both groups had a comorbid anxiety disorder (excluding PTSD) (Table 4). Personality disorders were also highly prevalent among those with substance use disorder plus PTSD (62.3%).
After we controlled for demographic characteristics and neuroticism in logistic regression, those with substance use disorder plus PTSD were significantly more likely to have a comorbid affective, anxiety, or personality disorder than those with substance use disorder alone or neither disorder. Those with substance use disorder plus PTSD were equally likely to have each of those comorbidities as those with PTSD alone.
Suicidal ideation and attempted suicide
More than half of those with substance use disorder plus PTSD had ever thought about suicide, and 17.3% had a lifetime history of attempted suicide (more data are available online). After we controlled for demographic characteristics and neuroticism in logistic regression, those with substance use disorder plus PTSD were no more or less likely to have ever considered or attempted suicide than those with substance use disorder or PTSD alone. Although those with substance use disorder plus PTSD were no more likely to have considered suicide than those with neither disorder, they were more likely to have a lifetime history of attempted suicide.
Disability
After we controlled for demographic characteristics and neuroticism in logistic regression, those with substance use disorder plus PTSD were more likely to have had at least 1 day out of role in the last month than those with substance use disorder alone (53.7% versus 24.4%) (odds ratio=2.79, 95% CI=1.60–4.85) and neither disorder (53.7% versus 17.1%) (odds ratio=4.03, 95% CI=2.36–6.87). There was no difference in the likelihood of having had at least 1 day out of role in the last month between those with substance use disorder plus PTSD and those with PTSD alone (53.7% versus 40.3%) (odds ratio=1.39, 95% CI=0.72–2.69).
Discussion
Consistent with previous epidemiological and clinical investigations conducted in the United States (1 , 5) , the present study found that substance use disorder and PTSD were highly comorbid conditions experienced by over 62,000 Australians. This represents a significant minority of the general population. Approximately one-third of those with PTSD also had a substance use disorder, and 5.9% of those with a substance use disorder also had PTSD. The presence of either disorder significantly increased the likelihood of having the other (odds ratio=6.53). These findings provide further evidence that there is a significant association between substance use disorder and PTSD and that their co-occurrence in clinical samples is not merely due to selection bias. Previous research has demonstrated that traumas leading to PTSD are experienced at similar rates in both Australia and the United States (2) .
Trauma exposure and PTSD were highly prevalent across all substance use disorders. Notably, the highest rates of PTSD were among those with opioid, sedative, or amphetamine use disorders. It should be noted, however, that substances used are likely to be influenced by the drug markets of particular countries. Cocaine use disorders were not measured in the National Survey of Mental Health and Well-Being because of the low prevalence of use among the Australian population. However, Cottler et al. (3) found a strong association between cocaine use and PTSD in the ECA study. Nonetheless, findings from the present study and studies from the United States have demonstrated a clear association between PTSD and hard-core drug use across cultures.
The elevated prevalence of PTSD among hard-core substance abusers may be due in part to the high-risk lifestyle associated with this kind of drug use. This lifestyle increases the risk of exposure to trauma, indirectly increasing the likelihood of subsequent PTSD (17) . However, for two-thirds of those diagnosed with both a substance use disorder and PTSD, symptoms of substance use disorder followed or developed at the same time as their most traumatic event, suggesting that the majority of those with this comorbidity may be self-medicating their PTSD symptoms (18) . The cross-sectional nature of this study does not allow for strong causal inferences to be made; however, it seems important that treatments for this comorbid substance use disorder plus PTSD focus on the interconnectedness of the two disorders.
As found in the clinical literature (8) , individuals with lifetime trauma exposure were also found to abuse or be dependent on multiple substances. It may be that individuals with substance use disorder plus PTSD require the use of multiple substances to alleviate different symptoms of PTSD or to overcome tolerance to one drug. The high rate of polydrug use among those with PTSD is of concern because of the harms associated with polydrug use, including overdose (19) , poor physical and mental health (20) , and HIV risk-taking behavior (21) . Because substance use disorder categories in the present study were not mutually exclusive and no measure was taken of primary drug of concern, associations between different substances and particular trauma types, the chronicity of PTSD, and PTSD symptom clusters could not be examined. It is recommended that future research examine these associations by participants’ primary drug of concern.
Individuals with substance use disorder plus PTSD were typically young, unmarried, or not in a de facto relationship and derived their main source of income from a government allowance. Together, these findings indicate that individuals with substance use disorder plus PTSD have poorer social and occupational functioning, particularly when compared with those with substance use disorder alone. Similar findings have been noted in both Australian and American studies of individuals with comorbid substance use disorder plus PTSD (8 , 22) . These associations are of clinical concern because it has been suggested that the lack of support from an intimate partner and financial constraints may create practical and emotional barriers to accessing treatment and may be potential risk factors for relapse after treatment (23) .
In keeping with studies of people seeking treatment for a substance use disorder in both the United States and Australia (6 , 8) , those with substance use disorder plus PTSD were found to be in poorer general physical and mental health compared to those with substance use disorder alone, with 12-Item Short-Form Health Survey Questionnaire scores between and 1 standard deviations below the population mean, respectively (13) . Affective, anxiety, and personality disorders were also more prevalent among those with this comorbidity; however, they were no more likely to have considered or attempted suicide. Nonetheless, it should be noted that approximately one in five people with either substance use disorder plus PTSD or substance use disorder alone had a lifetime history of attempted suicide. Given their poorer physical and mental health, it is not surprising that those with substance use disorder plus PTSD were more likely to have had a day out of role in the preceding month. These findings are of relevance to treatment providers because many of these psychological correlates have been shown to have a negative impact on substance use disorder treatment outcomes (24) . These findings also reveal that individuals with comorbid substance use disorder plus PTSD demonstrate a significant challenge to treatment providers and are likely to require substantial clinical resources.
Although those with substance use disorder plus PTSD were more likely to have a chronic health condition and had a greater number of health conditions than those with PTSD alone, the two groups shared a remarkably similar clinical profile. This finding indicates that the additional morbidity seen among individuals with substance use disorder plus PTSD may be attributed largely to PTSD. Thus, treating substance use disorder alone in such circumstances is unlikely to remedy the other problems experienced by individuals with this comorbidity (7) . This is not to say that by treating PTSD the substance use disorder will resolve but rather that both disorders should be treated concurrently.
Findings from the present study must be considered in light of a number of limitations. Despite the sophisticated sampling design used in the National Survey of Mental Health and Well-Being, it is unlikely that the sample is representative of all those with a substance use disorder or PTSD because of the hidden nature of this population and the difficulties inherent in accessing these individuals. For example, a small but significant proportion of those with substance use disorder and PTSD are homeless. Because participants were recruited from private dwellings, these individuals would not be represented in the present study. Furthermore, underreporting of drug use by patients with mental illness has been reported in studies that compared self-report measures with observer reports and laboratory tests (25) . Two studies, however, have examined self-reported substance use among those with PTSD and found their responses to be highly valid (26 , 27) .
In spite of these limitations, the present study has provided important information regarding the clinical profile of individuals with substance use disorder plus PTSD. The similarity in findings from studies conducted in the United States and Australia also demonstrates that these associations occur in spite of differences in culture, drug use, and the provision of substance abuse treatment. It is important that individuals are assessed for substance use disorder plus PTSD upon entry into treatment for either disorder so that they may receive appropriate referral and treatment. It is also important that future research examine the impact of this comorbidity on treatment outcomes because current studies of this association are limited. Additionally, further research is necessary to determine which treatments are most effective in treating comorbid substance use disorder plus PTSD (28) .
1. Kessler RC, Sonnega A, Bromet E, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
2. Creamer M, Burgess P, McFarlane AC: Post-traumatic stress disorder: findings from the Australian National Survey of Mental Health and Well-Being. Psychol Med 2001; 31:1237–1247Google Scholar
3. Cottler LB, Compton WM III, Mager D, Spitznagel EL, Janca A: Posttraumatic stress disorder among substance users from the general population. Am J Psychiatry 1992; 149:664–670Google Scholar
4. Chilcoat HD, Menard C: Epidemiological investigations: comorbidity of posttraumatic stress disorder and substance use disorder, in Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Edited by Ouimette PC, Brown PJ. Washington, DC, American Psychological Association, 2003Google Scholar
5. Bonin MF, Norton G, Asmundson GJ, Dicurzio S, Pidlubney S: Drinking away the hurt: the nature and prevalence of PTSD in substance abuse patients attending a community-based treatment program. J Behav Ther Exp Psychiatry 2000; 31:55–66Google Scholar
6. Brown PJ, Stout RL, Mueller T: Substance use disorder and posttraumatic stress disorder comorbidity: addiction and psychiatric treatment rates. Psychol Addict Behav 1999; 13:115–122Google Scholar
7. Najavits LM, Weiss RD, Shaw SR: A clinical profile of women with PTSD and substance dependence. Psychol Addict Behav 1999; 13:98–104Google Scholar
8. Mills KL, Lynskey M, Teesson M, Ross J, Darke S: Post-traumatic stress disorder among people with heroin dependence in the Australian Treatment Outcome Study (ATOS): prevalence and correlates. Drug Alcohol Depend 2005; 77:243–249Google Scholar
9. Meisler AW: Trauma, PTSD, and substance abuse. PTSD Res Quarterly 1996; 7:1–8Google Scholar
10. Ouimette PC, Brown PJ, Najavits LM: Course and treatment of patients with both substance use and posttraumatic stress disorders. Addict Behav 1998; 23:785–795Google Scholar
11. Andrews G, Henderson S, Hall W: Prevalence, comorbidity, disability and service utilisation. Br J Psychiatry 2001; 178:145–153Google Scholar
12. Eysenck SB, Eysenck HJ, Barrett P: A revised version of the Psychoticism Scale. Pers Individ Dif 1985; 6:21–29Google Scholar
13. Ware J Jr, Kosinski M, Keller SD: A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233Google Scholar
14. World Health Organization: Composite International Diagnostic Interview (CIDI), Version 2.1. Geneva, WHO, 1997Google Scholar
15. Degenhardt LJ, Hall W, Lynskey M: Alcohol, cannabis and tobacco use among Australians: a comparison of their associations with other drug use and use disorders, affective and anxiety disorders, and psychosis. Addiction 2001; 96:1603–1614Google Scholar
16. Landis R, Koch G: The measurement of observer agreement for categorical data. Biometrics 1977; 33:159–174Google Scholar
17. Chilcoat HD, Breslau N: Investigations of causal pathways between PTSD and drug use disorders. Addict Behav 1998; 23:827–840Google Scholar
18. Khantzian EJ: The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry 1997; 4:231–244Google Scholar
19. Darke S, Ross J, Zador D, Sunjic S: Heroin-related deaths in New South Wales, Australia, 1992–1996. Drug Alcohol Depend 2000; 60:141–150Google Scholar
20. Leri F, Bruneau J, Stewart J: Understanding polydrug use: review of heroin and cocaine co-use. Addiction 2003; 98:7–22Google Scholar
21. Darke S, Swift W, Hall W, Ross M: Drug use, HIV risk-taking and psychosocial correlates of benzodiazepine use among methadone maintenance clients. Drug Alcohol Depend 1994; 34:67–70Google Scholar
22. Ouimette PC, Finney JW, Moos RH: Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychol Addict Behav 1999; 13:105–114Google Scholar
23. Riggs DS, Rukstalis M, Volpicelli JR, Kalmanson D, Foa EB: Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: potential pitfalls to PTSD treatment. Addict Behav 2003; 28:1717–1730Google Scholar
24. Darke S, Ross J: Polydrug dependence and psychiatric comorbidity among heroin injectors. Drug Alcohol Depend 1997; 48:135–141Google Scholar
25. Goldfinger SM, Schutt RK, Seidman LJ, Turner WM, Penk WE, Tolomiczenko GS: Self-report and observer measures of substance abuse among homeless mentally ill persons in the cross-section and over time. J Nerv Ment Dis 1996; 184:667–672Google Scholar
26. Calhoun PS, Sampson WS, Bosworth HB, Feldman ME, Kirby AC, Hertzberg MA, Wampler TP, Tate-Williams F, Moore SD, Beckham JC: Drug use and validity of substance use self-reports in veterans seeking help for posttraumatic stress disorder. J Consult Clin Psychol 2000; 68:923–927Google Scholar
27. Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D: Validity of substance use self-reports in dually diagnosed outpatients. Am J Psychiatry 1998; 155:127–128Google Scholar
28. Ouimette PC, Moos RH, Brown PJ: Substance use disorder-posttraumatic stress disorder comorbidity: a survey of treatments and proposed practice guidelines, in Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Edited by Ouimette PC, Brown PJ. Washington, DC, American Psychological Association, 2003, pp 91–110Google Scholar



