Posttraumatic Stress Disorder and Depression in Battle-Injured Soldiers
Abstract
Objective: This study examined rates, predictors, and course of probable posttraumatic stress disorder (PTSD) and depression among seriously injured soldiers during and following hospitalization. Method: The patients were 613 U.S. soldiers hospitalized following serious combat injury. Standardized screening instruments were administered 1, 4, and 7 months following injury; 243 soldiers completed all three assessments. Cross-sectional and longitudinal analyses of risk factors were performed. PTSD was assessed with the PTSD Checklist; depression was assessed with the Patient Health Questionnaire. Combat exposure, deployment length, and severity of physical problems were also assessed. Results: At 1 month, 4.2% of the soldiers had probable PTSD and 4.4% had depression; at 4 months, 12.2% had PTSD and 8.9% had depression; at 7 months, 12.0% had PTSD and 9.3% had depression. In the longitudinal cohort, 78.8% of those positive for PTSD or depression at 7 months screened negative for both conditions at 1 month. High levels of physical problems at 1 month were significantly predictive of PTSD (odds ratio=9.1) and depression at 7 months (odds ratio=5.7) when the analysis controlled for demographic variables, combat exposure, and duration of deployment. Physical problem severity at 1 month was also associated with PTSD and depression severity at 7 months after control for 1-month PTSD and depression severity, demographic variables, combat exposure, and deployment length. Conclusions: Early severity of physical problems was strongly associated with later PTSD or depression. The majority of soldiers with PTSD or depression at 7 months did not meet criteria for either condition at 1 month.
Many soldiers wounded in Afghanistan or Iraq who would have died in prior wars now survive (1 , 2) . However, they may sustain lasting injuries resulting in disfigurement or loss of function. A recent study of combat troops following return from deployment to Afghanistan or Iraq found postwar rates of posttraumatic stress disorder (PTSD) ranging from 12.2% to 12.9% and rates of depression from 7.1% to 7.9%. Higher rates of PTSD were associated with higher levels of direct combat exposure and minor wounds or injury (3) . In comparison, one study of reserve and National Guard veterans from the Gulf War era found rates of PTSD ranging from 7.0% to 22.6% (4) . Rates of PTSD among soldiers returning from that war increased with the passage of time following return from deployment (5) .
Injured soldiers and those with higher levels of combat exposure have generally had higher rates of PTSD following previous wars (4 , 6 , 7) . However, rarely have these soldiers been studied shortly following injury (8 , 9) . A small study of Israeli soldiers found that 16.7% of injured soldiers had PTSD approximately 15 months following injury, compared to 2.5% of noninjured soldiers with similar combat experiences (9) .
Injury and PTSD have been studied in other populations, particularly patients admitted to trauma centers. Rates of PTSD in trauma center patients 12 months after injury have ranged from 2% to 30% (10 – 13) . The course of PTSD in trauma center patients is highly variable. As many as one-half of patients who have depression or PTSD at 3 months may no longer have a diagnosis of either condition at 12 months (10) . Of trauma center patients diagnosed with PTSD at 12 months, nearly one-half may not have had the diagnosis when assessed closer to the time of injury (13) .
Objective measures of physical injury are often not related to PTSD outcome (11 , 12) . High levels of physical problems, chronic pain, and seeking of medical care are often seen in patients diagnosed with PTSD (14 – 18) . However, the relationship of pain and other physical problems shortly after injury to PTSD outcome has not been well studied.
To better understand the frequency, course, and predictors of PTSD and depression in war-injured soldiers, consecutive soldiers wounded in Iraq and Afghanistan and admitted to one tertiary care hospital in the United States were examined. The soldiers were assessed at 1, 4, and 7 months following injury. In this study we examined the rates and risk factors for probable PTSD and depression at 1 month, 4 months, and 7 months.
Method
Subjects
During the period from March 2003 to September 2004, 7,609 U.S. soldiers were injured in combat. Of these, 3,674 received minor injuries and were returned to duty; 3,935 personnel required further care that prevented their return to duty. The exact distribution of injured troops among military hospitals has not been published. However, the most severely injured among Army personnel were evacuated to Walter Reed Army Medical Center. Soldiers evacuated from combat in Iraq and Afghanistan to Walter Reed Army Medical Center were psychiatrically assessed within 48 hours of admission and were provided psychiatric treatment as indicated throughout the course of hospitalization (19) . Approximately 1 month after the injury, standardized screening instruments were administered. The screening instruments were not administered to soldiers with severe cognitive injury and those who remained in intensive care settings (approximately 5% of the total). Soldiers were reassessed 4 and 7 months after the injury, either by telephone interview or upon return to the hospital for outpatient treatment.
Clinical records were examined from the first 613 soldiers who were admitted to Walter Reed Army Medical Center, required extended treatment, and were capable of completing the screening battery. All of these soldiers had life-threatening or seriously disfiguring injuries requiring high-acuity inpatient medical care lasting from weeks to months and resulting in persistent loss of function. The injuries were multiple and serious: amputations, fractures, closed-head trauma, open cranial trauma, chest trauma, ocular injury, spinal cord injury, and muscle, nerve, and vascular injuries caused by shrapnel or gunshot wounds. Permission to analyze data from these patients with identifying information removed was provided by the Department of Clinical Investigation at Walter Reed Army Medical Center.
Assessments
The presence or absence of probable PTSD was assessed with the 17-item National Center for PTSD Checklist of the Department of Veterans Affairs (20 – 24) . The PTSD Checklist lists all symptoms of PTSD in DSM-IV-TR. Soldiers rated “how much you have been bothered by each problem in the past month.” The ratings for the possible responses were 1 (“not at all”), 2 (“a little bit”), 3 (“moderately”), 4 (“quite a bit”), and 5 (“extremely”). The responses were summed to create a severity scale (range=17–85). Subjects were categorized as positive for PTSD if they reported at least one intrusion symptom, three avoidance symptoms, and two hyperarousal symptoms, each present at the level of moderate or higher during the past month, and if they received a PTSD Checklist symptom severity score of 50 or higher (3 , 20) .
Probable depression was assessed by using the nine-item Patient Health Questionnaire depression scale (25 , 26) . Probable depression was defined as the presence of five or more of the nine symptoms “more than half the days” or “nearly every day” in the past 2 weeks and the presence of depressed mood or anhedonia among those symptoms. When compared against structured clinical evaluations in primary care settings, the Patient Health Questionnaire depression scale demonstrated 73% sensitivity and 94% specificity and a test-retest reliability correlation (r) of 0.84 (25 , 26) .
Two measures of war exposure were used. One measure was duration of deployment (range=0–18 months, median=5.0, mean=5.00, SD=3.10, skewness=0.87, upper quartile=7 or more months). In addition, the soldiers were asked about specific traumatic exposures during deployment (3) . The positive responses were summed to create a combat exposure severity score (range=0–11, median=7.00, mean=6.14, SD=2.75, skewness=–0.48).
The injuries were serious and chronic. The 15-item Patient Health Questionnaire somatic symptom severity scale was used as a measure of severity of physical problems arising from the injuries (27) . The scale includes seven questions about regional pain and eight questions about general physical discomfort (e.g., nausea and dizziness). The usual scoring method was used—patients rate the severity of each symptom as 0 (“not bothered at all”), 1 (“bothered a little”), or 2 (“bothered a lot”). Two symptoms normally included, “feeling tired or having little energy” and “trouble sleeping,” were excluded from the scale because they are also represented in the depression scale. The responses were summed to create a physical problem severity scale (range=0–26, median=5.00, mean=5.53, SD=3.85, skewness=0.98, upper quartile=8 or more).
Statistical Analysis
Rates of PTSD and depression at 1 month, 4 months, and 7 months are reported for the cross-sectional sample. All predictive analyses were performed by using Statistical Software for the Social Sciences, version 12.02 (Chicago, SPSS). Predictors of PTSD and depression at each evaluation point were examined by using hierarchical multivariable logistic regression models.
Age (25 years and above versus less than 25), marital status, and gender were first examined together in the multivariable logistic regression to determine the relative effects of each when all others were controlled. Combat exposure (upper half) and duration of deployment (upper quartile) were then added to the logistic regression model. In the third step, physical problem severity (upper quartile) was added to the logistic regression model along with all prior variables.
A longitudinal cohort including soldiers who had been evaluated at all three times (1, 4, and 7 months) was also examined. Rates of PTSD and depression at each evaluation point as well as the time of illness onset were examined. To assess early predictors of later-onset PTSD and depression, the hierarchical multivariable logistic regression models just described were used. The soldiers who did not meet the criteria for PTSD or depression at 1 month but who did meet the criteria at 7 months were compared to those who remained below the diagnostic thresholds at 7 months.
To understand early predictors of the severity of PTSD and depression at 7 months, the severity scores for PTSD (PTSD Checklist) and depression (Patient Health Questionnaire) at 7 months were then examined in relation to age, gender, marital status, 1-month PTSD severity score, 1-month depression severity score, 1-month physical problem severity score, total combat exposure, and deployment length, by using bivariate correlations (Pearson). Predictive models of PTSD and depression severity at 7 months were examined by using multivariable linear regression including age, gender, marital status, 1-month PTSD severity score, 1-month depression severity score, 1-month physical problem severity score, combat exposure, and deployment length. The predictive value of the model and beta values and p values for the significant predictive variables are reported.
Results
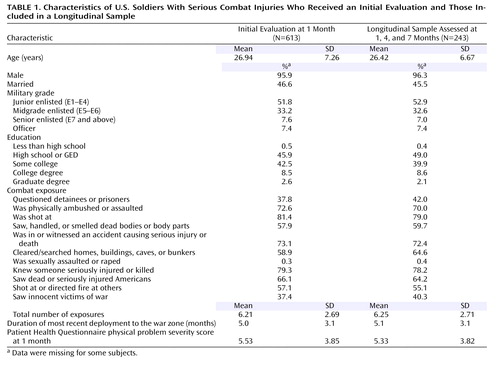
At 1 month after their injuries, 613 soldiers received an initial assessment. At 4 months 395 (72.3% of those eligible) were reassessed, and at 7 months 301 (61.1% of those eligible) were reassessed. All three assessments were completed by 243 soldiers (49.9% of those eligible). Of the soldiers who were contacted, fewer than 0.5% refused to participate in the follow-up. The remainder could not be contacted for follow-up assessment. There were no differences in the rates of probable depression, probable PTSD, or the presence of either condition at 1 month between the soldiers who completed all three assessments and those who could not be contacted for follow-up assessment. Demographic data, combat exposure, duration of deployment, and physical problem severity for the initial assessment group and the longitudinal cohort (evaluated at all three times) were similar and are provided in Table 1 .
Assessments at 1, 4, and 7 Months
At 1 month, 26 of the 613 soldiers (4.2%) met the criteria for PTSD and 27 (4.4%) met the criteria for depression. Forty-one soldiers (6.7%) met the criteria for either PTSD or depression, and 12 (2.0%) met the criteria for both PTSD and depression. At 4 months, 48 of 395 soldiers (12.2%) met the criteria for PTSD and 35 (8.9%) met the criteria for depression. Fifty-three soldiers (13.4%) met the criteria for either PTSD or depression, and 30 (7.6%) met the criteria for both PTSD and depression. At 7 months, 36 of 301 soldiers (12.0%) met the criteria for PTSD and 28 (9.3%) met the criteria for depression. Forty-five soldiers (15.0%) met the criteria for either PTSD or depression, and 19 (6.3%) met the criteria for both conditions.
At the 1-month assessment, when age, sex, and marital status were examined together in a single logistic regression model, soldiers under the age of 25 were more likely to meet the PTSD criteria than were soldiers age 25 or older; the odds ratio was 3.4, and the 95% confidence interval (CI) was 1.4–8.4 (Wald χ 2 =7.23, df=1, p=0.02). The younger soldiers were also 2.9 times as likely to meet the depression criteria (95% CI=1.2–6.9, Wald χ 2 =5.66, df=1, p=0.02). Married soldiers were 3.1 times as likely to meet the PTSD criteria (95% CI=1.3–7.4, Wald χ 2 =6.17, df=1, p=0.02) and 2.7 times as likely to meet the depression criteria (95% CI=1.2–6.5, Wald χ 2 =5.16, df=1, p=0.03) as were unmarried soldiers. At the 4- and 7-month assessments, no demographic factors were associated with probable PTSD or depression.
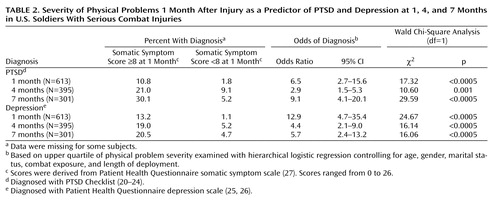
When high combat exposure and long deployment were added to the logistic regression model, the soldiers with high combat exposure were 4.8 times as likely to meet the PTSD criteria at 1 month (95% CI=1.6–14.4, Wald χ 2 =7.74, df=1, p=0.005) as were those with lower combat exposure. However, they were not more likely to have depression at 1 month. Combat exposure was not significantly associated with risk for PTSD or depression at 4 months or 7 months. Long deployment was not associated with PTSD or depression at any of the three time points. Severity of physical problems was then entered into the logistic regression model. High severity of physical problems at 1 month was significantly associated with PTSD and depression at all time points: 1, 4, and 7 months ( Table 2 ).
Longitudinal Cohort
In the longitudinal cohort (N=243), eight soldiers (3.3%) met the criteria for PTSD and 11 (4.5%) met the criteria for depression at 1 month. Fifteen soldiers (6.2%) met the criteria for PTSD or depression and four (1.6%) met the criteria for both PTSD and depression. At 4 months, 23 soldiers (9.5%) met the criteria for PTSD and 18 (7.4%) met the criteria for depression. Twenty-five soldiers (10.3%) met the criteria for PTSD or depression, and 16 (6.6%) met the criteria for both PTSD and depression. At 7 months, 25 soldiers (10.3%) met the criteria for PTSD and 21 (8.6%) met the criteria for depression. Thirty-three soldiers (13.6%) met the criteria for PTSD or depression, and 13 (5.4%) met the criteria for both PTSD and depression. The rates of probable PTSD and depression at each assessment and the time of onset are depicted in Figure 1 .
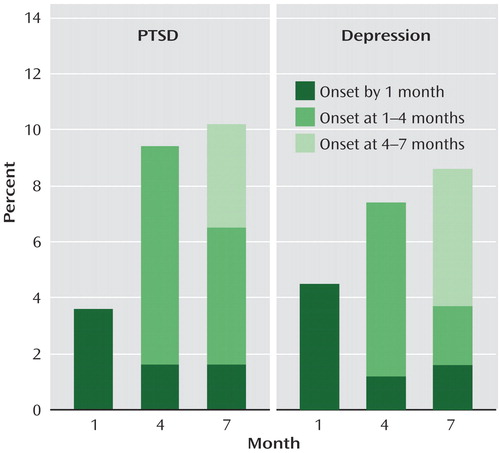
Eight of the 15 soldiers who met the criteria for PTSD or depression at 1 month (53.3%) no longer met the criteria for either condition at 7 months. Of the 228 soldiers who were negative for both PTSD and depression at 1 month, 26 (11.4%) had positive screening results for either PTSD or depression at 7 months. As a result, 78.8% of those with a positive result for either PTSD or depression at 7 months (26 of 33) had had a negative result for both conditions at the initial assessment.
Predictors of Later Onset of PTSD or Depression
To better understand which soldiers had later onset of PTSD or depression, we next examined those who did not meet the diagnostic criteria at 1 month. Using the logistic regression analysis already described, we found similar predictors in this group. Those with a high severity of physical problems at 1 month were at 7.0 times greater risk of PTSD at 7 months (95% CI=3.1–16.0, Wald χ 2 =21.29, df=1, p<0.0005) and 4.8 times greater risk of depression at 7 months (95% CI=2.0–11.8, Wald χ 2 =11.75, df=1, p=0.001) than those with lower physical problem severity. Age, gender, and marital status were not associated with later onset of PTSD or depression. Similarly, neither combat exposure nor long deployment was associated with later onset of PTSD or depression.
Predictors of Symptom Severity at 7 Months
The severity of PTSD at 7 months was significantly related to the severity of PTSD at 1 month (r=0.52, N=243, p<0.0005), depression severity at 1 month (r=0.37, N=243, p<0.005), and physical problem severity at 1 month (r=0.44, N=243, p<0.0005), but not age, gender, marital status, combat exposure, or deployment length. The multiple linear regression model to predict PTSD severity at 7 months included age, gender, marital status, combat exposure, deployment length, 1-month PTSD severity, 1-month depression severity, and 1-month physical problem severity. The model was significant (R 2 =0.31, F=13.15, df=8, p<0.0005). PTSD severity at 1 month (β=0.48, p<0.0005) and physical problem severity at 1 month (β=0.26, p<0.0005) significantly predicted PTSD severity at 7 months.
The severity of depression at 7 months was significantly associated with depression severity at 1 month (r=0.34, N=243, p<0.0005), PTSD severity at 1 month (r=0.44, N=243, p<0.0005), and physical problem severity at 1 month (r=0.40, N=243, p<0.0005), but not age, gender, marital status, combat exposure, or deployment length. The multiple linear regression model to predict depression severity at 7 months included age, gender, marital status, combat exposure, deployment length, 1-month PTSD severity, 1-month depression severity, and 1-month physical problem severity. The regression model was significant (R 2 =0.24, F=9.19, df=8, p<0.0005). PTSD severity at 1 month (β=0.34, p<0.0005) and physical problem severity at 1 month (β=0.26, p=0.0005) predicted depression severity at 7 months.
Discussion
Physical wounds sustained during combat contribute to both physical and psychological burdens. Physical wounds of war are preceded by multiple combat exposures such as being shot at, having friends seriously injured or killed, seeing dead comrades, and directing violent force toward the enemy. The interaction across time of injury, combat exposure, pain, general somatic complaints, success of physical recovery, concern over long-term dysfunction, medical care, and social supports results in a complex course of illness and recovery.
To our knowledge, this is the first report of rates of PTSD and depression among soldiers seriously wounded or injured during combat duty in Iraq or Afghanistan. The prevalence of a positive screening result for either PTSD or depression was about 7% soon after arrival at the U.S. tertiary care hospital, a rate similar to baseline rates in nonexposed soldiers or in the general population. At 4 and 7 months the rates of PTSD (12%) and depression (9%) were similar to those found in returning combat soldiers who were not seriously wounded (3) . The majority of soldiers with PTSD or depression at 7 months had not met the criteria for either condition 1 month following injury. These findings highlight the clinical challenges of providing early psychiatric care for war-wounded military personnel.
It is unclear what factors contribute to low initial rates of PTSD and depression. High levels of social and medical support, pain or sleep medications routinely administered during the immediate postinjury period, and focus on recovery may all be factors. Unlike survivors of motor vehicle accidents (28) , these soldiers did not have a predictable trend of recovery from PTSD across time. As in prior studies (5 , 10 , 13) , we found significant changes in psychiatric diagnoses across the 7 months of follow-up. Later onset of symptoms was found in a substantial number of soldiers. Persisting physical problems, anticipation of returning home and starting work, concern over health care, and pending disability determinations may also have affected the reporting of symptoms at follow-up (29) .
The rates of PTSD and depression in this sample at 4 and 7 months were lower than the 20%–33% lifetime risk for PTSD previously reported among injured Vietnam veterans (6 , 30) . The rates are comparable to those found in accident victims admitted to trauma centers (15% for PTSD and 12% for depression at 12 months) (10) , higher than those in other studies of accident victims (2% at 12 months) (12) , and lower than in other studies that included a high percentage of physical assault survivors (30% at 12 months) (11) . Studies of veterans of the first Gulf War (5) suggest that these rates may rise with time. Further study is needed to assess the long-term mental health needs of these soldiers.
To our knowledge, this is the first study to report that early physical problems predict subsequent PTSD. Greater severity of physical problems as early as 1 month after injury was strongly associated with the presence of both early (1 month) and later (7 months) PTSD and depression. Physical problem severity at 1 month was also predictive of PTSD and depression severity at 7 months even when the analysis controlled for PTSD and depression severity at 1 month. Our measure of physical problem severity was a self-report and reflected the soldier’s experience of his or her injury, pain, and discomfort. Some studies of civilian trauma survivors found that objective measures of injury severity were not predictive of later PTSD. In those studies, personality factors, subjective experiences of the event, and high levels of physical problems at 1 year were strongly associated with PTSD at 1 year (11 , 12 , 18) . Our findings support the importance of self-reported measures of injury severity in understanding the longitudinal course of PTSD.
Our study is limited by the use of self-reported measures of PTSD and depression, although these instruments are well validated. The low percentage of female soldiers, the severity of the injuries in this sample, and the exclusion of soldiers with severe cognitive impairments limit the ability to generalize the findings to other populations. An important aspect of this study is the absence of an objective measure of injury severity or measures of other life stressors or social supports that may also have contributed to the resolution or worsening of symptoms after discharge from the hospital. This is an area for further study. Our analysis showed no demographic differences or differences in combat exposure, initial physical problems, or rates of initial PTSD or depression between the initial and longitudinal groups. Although there were no apparent differences in initial health status between the two groups, the loss of 35% to 50% of the soldiers between 1 month and the 4- and 7-month follow-ups may have resulted in bias in the findings.
Despite these limitations, we believe that this study is the first to demonstrate the early course of posttrauma PTSD and depression in soldiers seriously injured in combat and the first to show associations of the severity of early physical problems with later PTSD and depression. The course of illness in battle-injured soldiers is complex, and the initial assessments in this study were not predictive of the health or the life impact of such injuries 6 months later. In groups with extremely high levels of trauma exposure that includes serious physical injury, long-term prognosis may not be easily predicted by variation in measures of trauma exposure alone. In contrast, the findings of this study suggest that severity of physical problems shortly after the injury may be of value in predicting persistence or later onset of PTSD and depression in severely injured patients. Further study of the early course of PTSD in injured soldiers is needed.
1. Patel TH, Wenner KA, Price SA, Weber MA, Leveridge A, McAtee SJ: A US Army Forward Surgical Team’s experience in Operation Iraqi Freedom. J Trauma 2004; 57:201–207Google Scholar
2. Gawande A: Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med 2004; 351:2471–2475Google Scholar
3. Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL: Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351:13–22Google Scholar
4. Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM: Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol 2003; 157:141–148Google Scholar
5. Southwick SM, Morgan CA 3rd, Darnell A, Bremner D, Nicolaou AL, Nagy LM, Charney DS: Trauma-related symptoms in veterans of Operation Desert Storm: a 2-year follow-up. Am J Psychiatry 1995; 152:1150–1155Google Scholar
6. Kulka RA, Schlenger WE, Fairbank J, Hough RL, Jordan BK, Marmar CR, Weiss DS: Evidence of post-traumatic stress disorder, in Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990, pp 50–72Google Scholar
7. Ikin JF, Sim MR, Creamer MC, Forbes AB, McKenzie DP, Kelsall HL, Glass DC, McFarlane AC, Abramson MJ, Ittak P, Dwyer T, Blizzard L, Delaney KR, Horsley KW, Harrex WK, Schwarz H: War-related psychological stressors and risk of psychological disorders in Australian veterans of the 1991 Gulf War. Br J Psychiatry 2004; 185:116–126Google Scholar
8. Brandt GT, Norwood AE, Ursano RJ, Wain H, Jaccard JT, Fullerton CS, Wright K: Psychiatric morbidity in medical and surgical patients evacuated from the Persian Gulf War. Psychiatr Serv 1997; 48:102–104Google Scholar
9. Koren D, Norman D, Cohen A, Berman J, Klein EM: Increased PTSD risk with combat-related injury: a matched comparison study of injured and uninjured soldiers experiencing the same combat events. Am J Psychiatry 2005; 162:276–282Google Scholar
10. O’Donnell ML, Creamer M, Pattison P: Posttraumatic stress disorder and depression following trauma: understanding comorbidity. Am J Psychiatry 2004; 161:1390–1396Google Scholar
11. Zatzick DF, Kang S-M, Müller H-G, Russo JE, Rivara FP, Katon W, Jurkovich GJ, Roy-Byrne P: Predicting posttraumatic distress in hospitalized trauma survivors with acute injuries. Am J Psychiatry 2002; 159:941–946Google Scholar
12. Schnyder U, Moergeli H, Klaghofer R, Buddeberg C: Incidence and prediction of posttraumatic stress disorder symptoms in severely injured accident victims. Am J Psychiatry 2001; 158:594–599Google Scholar
13. Carty J, O’Donnell ML, Creamer M: Delayed-onset PTSD: A prospective study of injury survivors. J Affect Disord 2006; 90:257–261; Epub, Dec 27, 2005Google Scholar
14. Beckham JC, Crawford AL, Feldman ME, Kirby AC, Hertzberg MA, Davidson JR, Moore SD: Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. J Psychosom Res 1997; 43:379–389Google Scholar
15. Andreski P, Chilcoat H, Breslau N: Post-traumatic stress disorder and somatization symptoms: a prospective study. Psychiatry Res 1998; 79:131–138Google Scholar
16. Engel CC Jr, Liu X, McCarthy BD, Miller RF, Ursano R: Relationship of physical symptoms to posttraumatic stress disorder among veterans seeking care for Gulf War-related health concerns. Psychosom Med 2000; 62:739–745Google Scholar
17. Katon W, Sullivan M, Walker E: Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med 2001; 134(9 pt 2):917–925Google Scholar
18. Zatzick DF, Russo JE, Katon W: Somatic, posttraumatic stress, and depressive symptoms among injured patients treated in trauma surgery. Psychosomatics 2003; 44:479–484Google Scholar
19. Lamberg L: Military psychiatrists strive to quell soldiers’ nightmares of war. JAMA 2004; 292:1539–1540Google Scholar
20. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA: Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996; 34:669–673Google Scholar
21. Dobie DJ, Kivlahan DR, Maynard C, Bush KR, McFall M, Epler AJ, Bradley KA: Screening for post-traumatic stress disorder in female Veteran’s Affairs patients: validation of the PTSD Checklist. Gen Hosp Psychiatry 2002; 24:367–374Google Scholar
22. Forbes D, Creamer M, Biddle D: The validity of the PTSD Checklist as a measure of symptomatic change in combat-related PTSD. Behav Res Ther 2001; 39:977–986Google Scholar
23. Lang AJ, Laffaye C, Satz LE, Dresselhaus TR, Stein MB: Sensitivity and specificity of the PTSD Checklist in detecting PTSD in female veterans in primary care. J Trauma Stress 2003; 16:257–264Google Scholar
24. Walker EA, Newman E, Dobie DJ, Ciechanowski P, Katon W: Validation of the PTSD Checklist in an HMO sample of women. Gen Hosp Psychiatry 2002; 24:375–380Google Scholar
25. Spitzer RL, Kroenke K, Williams JBW, Patient Health Questionnaire Primary Care Study Group: Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 1999; 282:1737–1744Google Scholar
26. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613Google Scholar
27. Kroenke K, Spitzer RL, Williams JB: The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 2002; 64:258–266Google Scholar
28. Ursano RJ, Fullerton CS, Epstein RS, Crowley B, Kao TC, Vance K, Craig KJ, Dougall AL, Baum A: Acute and chronic posttraumatic stress disorder in motor vehicle accident victims. Am J Psychiatry 1999; 156:589–595Google Scholar
29. Frueh BC, Elhai JD, Gold PB, Monnier J, Magruder KM, Keane TM, Arana GW: Disability compensation seeking among veterans evaluated for posttraumatic stress disorder. Psychiatr Serv 2003; 54:84–91Google Scholar
30. Helzer JE, Robins LN, McEvoy L: Post-traumatic stress disorder in the general population: findings of the Epidemiologic Catchment Area Survey. N Engl J Med 1987; 317:1630–1634Google Scholar