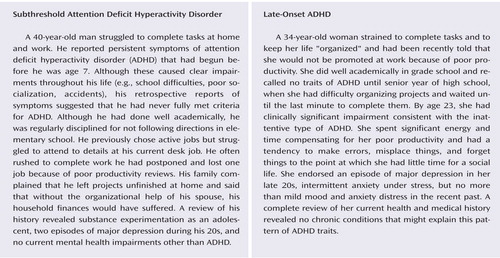
Diagnosing Adult Attention Deficit Hyperactivity Disorder: Are Late Onset and Subthreshold Diagnoses Valid?
Abstract
Objective: Diagnosing attention deficit hyperactivity disorder (ADHD) in adults is difficult when diagnosticians cannot establish an onset before the DSM-IV criterion of age 7 or if the number of symptoms recalled does not achieve DSM’s diagnosis threshold. Method: The authors addressed the validity of DSM-IV’s age-at-onset and symptom threshold criteria by comparing four groups of adults: 127 subjects with full ADHD who met all DSM-IV criteria for childhood-onset ADHD, 79 subjects with late-onset ADHD who met all criteria except the age-at-onset criterion, 41 subjects with subthreshold ADHD who did not meet full symptom criteria for ADHD, and 123 subjects without ADHD who did not meet any criteria. The authors hypothesized that subjects with late-onset and subthreshold ADHD would show patterns of psychiatric comorbidity, functional impairment, and familial transmission similar to those seen in subjects with full ADHD. Results: Subjects with late-onset and full ADHD had similar patterns of psychiatric comorbidity, functional impairment, and familial transmission. Most children with late onset of ADHD (83%) were younger than 12. Subthreshold ADHD was milder and showed a different pattern of familial transmission than the other forms of ADHD. Conclusions: The data about the clinical features of probands and the pattern of transmission of ADHD among relatives found little evidence for the validity of subthreshold ADHD among such subjects, who reported a lifetime history of some symptoms that never met DSM-IV’s threshold for diagnosis. In contrast, the results suggested that late-onset adult ADHD is valid and that DSM-IV’s age-at-onset criterion is too stringent.
Pediatricians, child psychiatrists, and psychologists regularly diagnose and treat attention deficit hyperactivity disorder (ADHD) in children, but recognition of ADHD in adulthood has faced many obstacles. Diagnosing ADHD in adults requires clinicians to obtain an accurate retrospective diagnosis of childhood-onset ADHD (1) and, although many studies suggest that these retrospective diagnoses are valid (2 – 4) , diagnostic issues remain. As McGough and Barkley (5) discussed, current DSM diagnostic criteria for ADHD have never been validated in adults, do not include developmentally appropriate symptoms and diagnostic thresholds, and do not identify some significantly impaired adults as having ADHD who are likely to benefit from treatment. Two particularly vexing diagnostic questions remain:
Should the age at onset criterion of ADHD be modified when making the adult diagnosis?
Should changes be made to symptom thresholds when making retrospective diagnoses of ADHD in adults?
Several studies of youth have challenged DSM-IV’s requirement that ADHD onset before age 7. The scant empirical data available question the validity of the age-at-onset criterion. One study comparing teenagers with onset before or after age 13 found no link between age at onset and severity of symptoms, types of adjustment difficulties, or the persistence of the disorder (6) . Rohde et al. (7) compared clinical features between adolescents meeting full criteria for ADHD and those meeting all criteria except age at onset. Because these two groups had similar profiles of clinical features, the authors concluded that DSM-IV’s age-at-onset criterion should be revised. In an epidemiologically ascertained sample of adolescents, Willoughby et al. (8) found that adolescents meeting full criteria for the combined type of ADHD had worse clinical outcomes than those failing to meet the age at onset criterion but found no differences attributable to the age at onset for the inattentive subtype of ADHD. In DSM-IV field trials, the requirement of an age at onset of 7 reduced the accuracy of identifying currently impaired cases of ADHD and reduced agreement with clinician judgments (9) .
When making the diagnosis of ADHD in adults, clinicians must establish that diagnostic criteria for the disorder were met in childhood. Because the passage of time may make symptoms difficult to recall, it is possible that the threshold for “caseness” should be lowered when one makes such retrospective diagnoses. But because lowering symptom thresholds would likely increase the risk for false positive diagnoses, systematic research is needed to address this issue.
In the present report, we address the validity of DSM-IV’s age at onset and symptom threshold criteria by comparing four groups of adults: 1) full ADHD subjects met all DSM-IV criteria for childhood-onset ADHD, 2) late-onset ADHD subjects met all criteria except the age-at-onset criterion, 3) subthreshold ADHD subjects had subthreshold symptoms, and d) non-ADHD subjects did not meet any of the above criteria. If late-onset and subthreshold ADHD are valid forms of ADHD, we hypothesized that 1) they would show patterns of psychiatric comorbidity, functional impairment, and neuropsychological dysfunction that are similar to those seen for full ADHD; 2) relatives of late-onset and subthreshold ADHD patients should be at increased risk for full ADHD compared with subjects without ADHD; and c) relatives of subjects with full ADHD should be at increased risk for late-onset and subthreshold ADHD compared with relatives of subjects without ADHD. Our two-family hypotheses are of particular importance. Because Robins and Guze (10) lay out in their framework for establishing the validity of psychiatric diagnoses, demonstrating familial transmission is a key validation criterion for heritable disorders. For our study of subthreshold and late-onset ADHD, this criterion is particularly important because demonstrating a familial link between a gold standard diagnosis (i.e., full ADHD) and a controversial diagnosis (i.e., subthreshold and late-onset ADHD) provides strong evidence for the validity of the latter.
Method
Subjects
Men and women between the ages of 18 and 55 were eligible to become probands for the study. Exclusion criteria were deafness, blindness, psychosis, inadequate command of the English language, or a full-scale IQ less than 80 as measured by the IQ estimated from the block design and vocabulary subtests of the Wechsler Adult Intelligence Scales—Revised. No ethnic or racial group was excluded. We used two ascertainment sources to recruit ADHD probands: referrals to psychiatric clinics at Massachusetts General Hospital and advertisements in the greater Boston area. We recruited potential probands without ADHD through advertisements in the greater Boston area. We ascertained and assessed the probands and all available biological children, parents, and siblings. The study was approved by the institutional review board at Massachusetts General Hospital. Every subject 18 and older provided signed informed consent. Younger relatives of the probands provided signed assent, and the parents provided signed informed consent. The confidentiality of the subjects was protected throughout the study.
Assessment Measures
Trained lay interviewers, blind to ascertainment status, interviewed all adults with the Structured Clinical Interview for DSM-IV (11) and modules from the Schedule for Affective Disorders and Schizophrenia for School-Age Children Epidemiologic Version (K-SADS-E) (12) . When we asked questions about childhood disorders, the subjects were first queried about childhood symptoms, and if they were present, they were asked about continuation of these symptoms into adulthood and the emergence of others. Age at onset was defined as the first emergence of impairing symptoms. Interviewers collected information for psychiatric diagnoses in child relatives (ages 6 to 18) with the K-SADS-E. Before interviewing for the study, interviewers completed a 4-month training program that included mastery of the instruments, learning about DSM-IV criteria, watching training tapes, observing interviews performed by experienced raters, rating several subjects under the supervision of the project coordinator and completing practice interviews. Throughout the study, they were supervised by board-certified child and adolescent psychiatrists or licensed psychologists. This supervision included weekly meetings and additional consultations, as needed. During the study, all interviews were audiotaped for random quality control assessments.
For all child relatives, psychiatric data were collected from the mother when available. In addition, child relatives 12 and older were directly evaluated. Final diagnostic assignment was based on the structured psychiatric interview. Initial diagnoses were prepared by the study interviewers and were then reviewed by a diagnostic committee of board-certified child and adolescent psychiatrists or licensed psychologists. The diagnostic committee was blind to each subject’s ascertainment group, all data collected from other family members, and all nondiagnostic data (e.g., cognitive functioning). Diagnoses were made for two points in time: lifetime and current (past month).
The interviewers had been instructed to take extensive notes about the symptoms for each disorder. These notes and the structured interview data were reviewed by the diagnostic committee so that the Committee could make a best-estimate diagnosis, as described by Leckman et al. (13) . Definite diagnoses were assigned to subjects who met all diagnostic criteria. Diagnoses were considered definite only if a consensus was achieved that criteria were met to a degree that would be considered clinically meaningful. By “clinically meaningful,” we mean that the data collected from the structured interview indicated that the diagnosis should be a clinical concern because of the nature of the symptoms, the associated impairment, and the coherence of the clinical picture.
The interviewers were blind to the subject’s baseline ascertainment group, the ascertainment site, and all prior assessments. The interviewers had undergraduate degrees in psychology and were extensively trained. First they underwent several weeks of classroom-style training, learning interview mechanics, diagnostic criteria, and coding algorithms. Then they observed interviews by experienced raters and clinicians. They subsequently conducted at least six practice (nonstudy) interviews and at least three study interviews while being observed by senior interviewers. Trainees were not permitted to conduct interviews independently until they executed at least three interviews that achieved perfect diagnostic agreement with an observing senior interviewer. A senior investigator (J.B.) supervised the interviewers throughout the study. We computed kappa coefficients of agreement by having experienced board-certified child and adult psychiatrists and licensed clinical psychologists diagnose subjects from audiotaped interviews. On the basis of 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98. Kappa coefficients for individual diagnoses were ADHD (0.88), conduct disorder (1.00), major depression (1.00), mania (0.95), separation anxiety (1.00), agoraphobia (1.00), panic (0.95), substance use disorder (1.00), and tics/Tourette’s disorder (0.89).
Statistical Analyses
Our analyses used logistic regression for binary outcomes, ordinal logistic regression for ordinal outcomes, Poisson regression for count data, multinomial logistic regression for categorical outcomes, and Gaussian regression for continuous outcomes. For each psychiatric disorder in Table 1 , we used Cox proportional hazard models to predict age of onset and proportion at risk. We then permuted group membership across subjects and recalculated our omnibus and pairwise statistics for permutation tests. Permutation testing calculates the probability of achieving a result through random assignment of subjects into groups by measuring the number of recalculated results greater than the observed statistic during a prescribed number of iterations. Using permutation tests allowed us to reinforce our results with low frequencies of psychiatric disorders in our groups without ADHD and subthreshold ADHD. For the same reasons, we used Fisher’s exact test to analyze differences in the frequency of subjects receiving different treatment options, numbers of relatives with full ADHD, and subthreshold ADHD across ADHD diagnosis groups.
Because multiple members of a single family cannot be considered independent of one another because they share genetic, cultural, and social risk factors, we used Huber-White robust estimates of variance in analyses of relatives so that p values would be accurately estimated. We used the following strategy to balance our risk for type I and type II errors when we adjusted for multiple comparisons. For each domain of analysis (as defined by the tables), we applied Bonferroni correction to the omnibus test for each variable in the domain. If that was significant, we used the 0.05 alpha level to assert significance for pairwise comparisons.
Results
Based on the retrospective reports of ADHD symptoms, we classified our probands into lifetime diagnostic categories. Full ADHD was defined as meeting full DSM-IV criteria for ADHD, with onset of some symptoms before age 7 (N=127). Late-onset ADHD was defined as meeting full DSM-IV criteria for ADHD except for the age-at-onset criterion (N=79). Because we did not place any restrictions on the age at onset for the late-onset group, the range of age at onset was wide (ages 7 to 45); 63% had an age at onset of 7, 8, or 9; and 83% had an age of onset in the 7-to-12-year range. Subthreshold ADHD was defined as never having met DSM-IV criteria for ADHD and reporting a chronic history of three or more inattentive symptoms or three or more hyperactive-impulsive symptoms (N=41). We defined the symptom cutoff for the subthreshold diagnosis based on our previous work (14) .
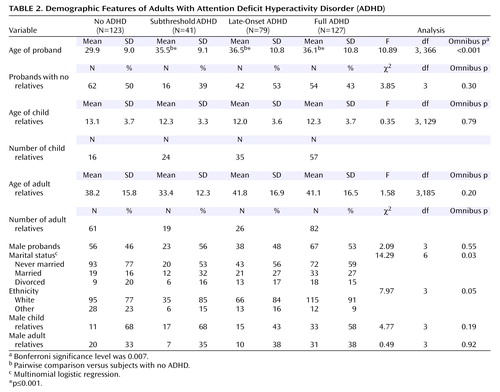
The remaining subjects were defined as not having ADHD (N=123). Of these 370 probands, 196 had 418 relatives; the remaining 174 probands had no relatives participating in the study. Table 2 shows that the four comparison groups did not differ in gender, marital status, the gender of their child relatives, the gender of their adult relatives, the age of their child relatives, and the age of their adult relatives. Because probands without ADHD were significantly younger and less likely to be Caucasian, subsequent analyses corrected for age. We also performed all analyses correcting for binary ethnicity (Caucasian versus other ethnicity) and all results remained significant.
Clinical Features
By definition, the group without ADHD and the subthreshold ADHD group could not meet full threshold criteria for ADHD at the time of their assessment in adulthood. Seventy percent of the subjects with a lifetime history of full ADHD met full symptom criteria for ADHD based on symptoms reported within the 6-month period before their interviews. For the late-onset group with ADHD, the prevalence was 68%, which was not significantly different (p=0.76).
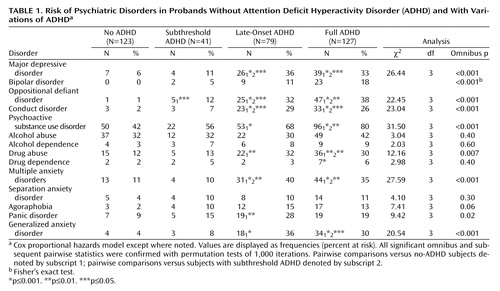
Table 1 shows the proportion of subjects at risk of comorbid psychiatric disorders in each proband. Compared with the probands without ADHD, the full ADHD and late-onset ADHD probands had an increased risk of mood, disruptive behavior, substance use, and anxiety disorders. In contrast, the subthreshold ADHD probands only showed an increased risk of oppositional defiant disorders. We found no significant differences in the risk of comorbidity between the full ADHD and late-onset ADHD probands but compared with subthreshold ADHD probands, both groups were more likely to have lifetime histories of mood disorders, disruptive behavior disorders, substance abuse, and multiple anxiety disorders (i.e., a history of two or more anxiety disorders).
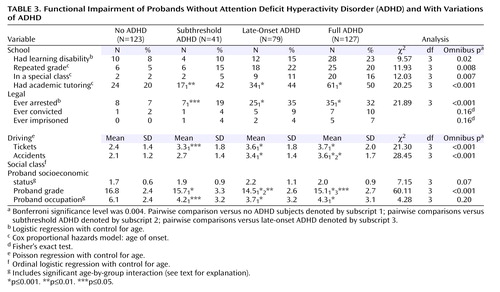
Table 3 describes evidence of functional impairments. Each ADHD group was significantly more likely to have required academic tutoring in school compared with the subjects without ADHD. The full ADHD and late-onset ADHD groups had the highest rates of learning disability, repeated grades, and placement in special classes, but these differences did not attain our Bonferroni-corrected level of statistical significance.
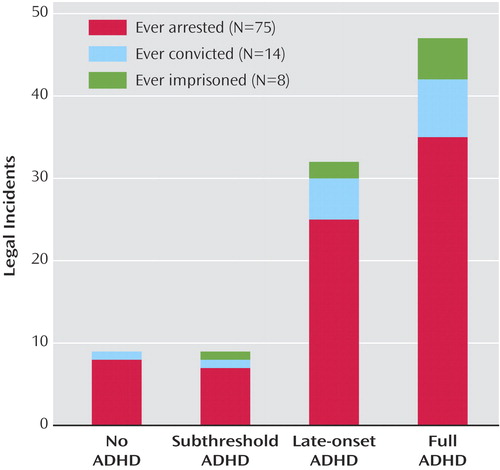
The ADHD cases were significantly more likely to have been arrested compared with the group without ADHD ( Figure 1 ). Both the late-onset and the full ADHD groups were about five times more likely to have been arrested than the group without ADHD. These results were marginally significant when we included the effect of conduct disorder (omnibus test: χ 2 =8.28, df=3, p=0.04; conduct disorder: odds ratio=7.7, 95% CI=3.9–15.1, p<0.001) but did not achieve our Bonferroni-corrected significance level of p=0.007. The ADHD groups were similar to one another in the number of traffic tickets received, and all had significantly more tickets than the group without ADHD. We saw a significantly increased risk for traffic accidents in the full- and late-onset ADHD groups but not in the subthreshold group, which did not differ significantly from the group without ADHD. The ADHD groups reported elevated rates of conviction and imprisonment, but the differences did not attain statistical significance ( Table 3 ).
We found no differences between the four groups in Hollingshead-Redlich socioeconomic status when we controlled for the group-specific effects of age. Subsequent analyses of each group showed that age had the strongest effect on the subjects without ADHD (ordinal logistic regression: χ 2 =6.40, df=1, p=0.01), with older subjects having significantly higher socioeconomic status. Similarly, we found no differences in proband occupation, a component of the socioeconomic status score, when we included the group-specific effects of age. Subsequent regression showed that within the group of subjects without ADHD (ordinal logistic regression: χ 2 =5.30, df=1, p=0.02) and subthreshold subjects (ordinal logistic regression: χ 2 =6.03, df=1, p=0.01), age had a positive effect on occupation. We found that the four groups differed in highest completed grade level, with no significant age-by-group interactions: the three groups with ADHD had completed lower grade levels than the group without ADHD. Pairwise tests showed that subjects with late-onset ADHD completed lower grades than the subjects with subthreshold or full ADHD. To determine if these differences in socioeconomic status might account for the other significant findings in Table 3 or Table 4 , we reanalyzed the data with control for socioeconomic status; all significant findings remained significant.
Familial Transmission of ADHD
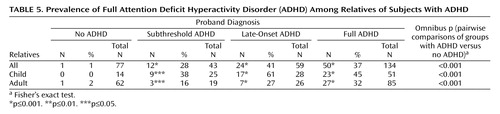
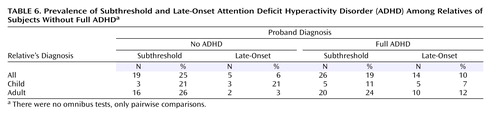
Our first familial transmission hypothesis predicted that the relatives of late-onset and subthreshold ADHD patients would be at increased risk for full ADHD compared with subjects without ADHD. Table 5 shows this is true when either all relatives or child and adult relatives are considered separately. Our second familial transmission hypothesis predicted that, when limiting the study group to relatives without full ADHD, the relatives of full ADHD subjects should be at increased risk for late onset and subthreshold ADHD compared with relatives of subjects without ADHD. Table 6 shows this hypothesis was not true for subthreshold ADHD. In contrast, we found an increased prevalence of late-onset ADHD among adult relatives of full ADHD probands compared with adult relatives of probands without ADHD. This differential transmission of late-onset ADHD was not seen for child relatives.
Treatment of ADHD
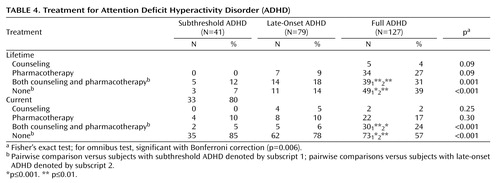
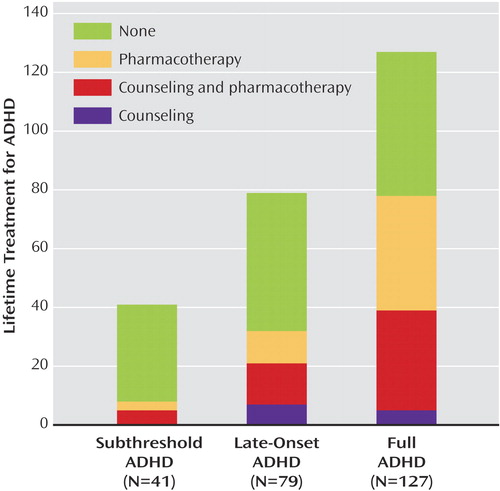
The data in Table 1 , Table 3 , Table 5 , and Table 6 documenting similarities and differences among the four subgroups provide information about the validity of subthreshold and late-onset ADHD. We also collected naturalistic treatment data to document how these disorders were treated in the community. As Table 4 shows, we found higher rates of both past and current multimodal treatment among patients with full ADHD compared with the other ADHD groups. The late-onset cases were more likely to receive treatment than the subthreshold cases, but the difference was significant only for lifetime history of no treatment, which was lower for the subjects with late-onset ADHD ( Figure 2 ).
Discussion
Our data about the clinical features of probands and the pattern of transmission of ADHD among relatives found little evidence for the validity of retrospective reports of subthreshold ADHD. In contrast, our results suggest that late-onset ADHD is valid and that DSM-IV’s age-at-onset criterion may be too stringent.
Clinical Features
Compared with the group without ADHD, the subthreshold group had a greater lifetime prevalence of oppositional defiant disorder. Consistent with the elevated rate of this disorder, the subthreshold group was more impaired than the group without ADHD, as assessed by the need for academic tutoring in childhood, the traffic citations received, the grade achieved in school, and occupational status. Although the clinical differences between the subthreshold group and the group without ADHD might be attributed to ADHD, the subthreshold group showed less psychopathology and impairment compared with both the late-onset and full ADHD groups. Thus, although the subthreshold group was significantly impaired, these results give only weak support for the validity of subthreshold ADHD.
Our analyses of clinical features yielded stronger evidence for the validity of late-onset ADHD. Notably, the fraction of subjects meeting full criteria for ADHD at the time of the interview did not differ between the late-onset and full ADHD groups. When compared with the subjects without ADHD, both groups had increased lifetime prevalences of mood, disruptive behavior, substance use, and anxiety disorders, each of which are known to be elevated among youth with ADHD (15 , 16) , clinically referred ADHD adults (17 , 18) , and ADHD youth followed into adulthood (19 , 20) . Our results confirm the finding of Hesslinger et al. (17) that adults with late-onset ADHD had the same pattern of psychiatric comorbidity as adults whose ADHD onset met DSM-IV’s criterion. In contrast, in an epidemiological sample of 9- to 16-year-old children, Willoughby et al. (8) did not find late-onset ADHD to be associated with oppositional defiant, conduct, or anxiety disorders. It was associated with depression among inattentive ADHD cases.
We found evidence of significant functional impairments in both the late-onset and full ADHD groups. These impairments were in domains known to affect ADHD children and adolescents: school functioning, legal difficulties, and traffic accidents. Compared with the subjects without ADHD, both the full and late-onset ADHD groups had achieved lower grade and occupational levels. These results confirm other studies showing adults with ADHD to be at risk for driving difficulties (21) , legal problems (19) , and school failure (22) . In the study by Willoughby et al. (8) of youth with ADHD, late onset of ADHD was associated with more functional impairments and greater service use in relation to comparison subjects without ADHD.
Familial Transmission
The family analyses are consistent with the analyses of clinical features in providing little evidence for the validity of subthreshold ADHD. When diagnosed in the proband, subthreshold ADHD predicted full ADHD in relatives and, hence, showed familial validity. But the diagnosis of subthreshold ADHD was equally prevalent among relatives without ADHD or full ADHD and the probands without ADHD, which argues against its validity. Notably, subthreshold ADHD was highly prevalent among the relatives of the probands without ADHD (25%). Because this prevalence provides a rough estimate of the population prevalence, it suggests that lowering the DSM-IV symptom threshold for retrospective diagnoses would yield many false positive diagnoses.
The two familial transmission analyses supported the idea that late-onset ADHD is a valid form of ADHD in adults. Relatives of late-onset probands had a significantly elevated risk for full ADHD, and the adult relatives of the proband with full ADHD had a significantly elevated risk for late-onset ADHD. The prevalence of late-onset ADHD was low (3%) among adult relatives of subjects without ADHD.
In contrast, the child relatives of probands with full ADHD did not have a significantly elevated risk for late-onset ADHD, and the prevalence of late-onset ADHD was high (19%) among adult relatives of subjects without ADHD. These findings suggest that late-onset ADHD diagnoses could produce a substantial rate of false positive diagnoses in youth.
Among the adult relatives of the probands without ADHD, the prevalence of full ADHD was 2%, and the prevalence of late-onset ADHD was 3%. Thus, allowance for later onset of ADHD symptoms in adults does not dramatically increase the prevalence of the disorder, and the combined prevalence of 5% is consistent with reports from other studies. Murphy and Barkley (23) used a self-report measure to assess ADHD among adults applying for driver’s licenses. They found a 4.7% prevalence of ADHD. Heiligenstein et al. (24) assessed ADHD among adult college students; 4% of these young adults met DSM-IV criteria for ADHD. In the National Comorbidity Survey, the prevalence of adult ADHD was 4.4% (25) .
Clinical Implications
There is no prior literature about retrospective reports of subthreshold lifetime diagnoses of ADHD in adults, and our results are ambiguous regarding the validity of such diagnoses. The 25% prevalence of subthreshold ADHD among relatives of the group without ADHD provides a rough estimate of how common subthreshold cases might be in the population. Because this is very high, logic dictates that the group must include many false positives. Given our relatively small subgroup of subthreshold ADHD probands, we could not determine if there might be a subset of subthreshold patients who truly have ADHD or if subthreshold symptoms and associated impairments are simply secondary to the comorbid disorders observed in this group.
Our data supporting the validity of late-onset ADHD is consistent with prior work suggesting that the DSM-IV requirement of onset before age 7 is too stringent for the diagnosis of adults. When viewed in the light of these studies, our data suggest that DSM-IV criteria for ADHD should be modified to allow for onset of symptoms after age 7. The available data do not allow for strong suggestions about how the cutoff point should be revised. Like prior studies, ours was not designed to determine what age at onset would be the most valid. Such a study would require sufficient numbers of subjects for each age category to be considered potentially valid. Ideally, the next DSM field trial for ADHD would incorporate such sampling considerations. Lacking a definitive cutoff point, what should clinicians do when faced with a patient with late-onset adult ADHD? Most of the subjects with late-onset ADHD reported onset before age 12. This suggests that later onsets, being relatively rare, should engender more clinician skepticism before they are diagnosed with ADHD not otherwise specified, the category DSM-IV provides for patients who appear to have ADHD but do not meet full criteria. This recommendation is consistent with that made by McGough and Barkley (5) based on a review of the adult ADHD literature.
Revision of the DSM age-at-onset criterion will face several challenges, which should be a focus for future research. Choosing a new cutoff point (or dropping the cutoff point altogether, as was done for schizophrenia) is not straightforward. Current research certainly supports the idea that a cutoff point of age 12 would be more valid than age 7, but no study has had a sufficient group size to ensure that another cutoff point might not be better. Future research should also seek to create a better definition of the clinical features of onset. Currently, DSM-IV describes onset rather vaguely as “symptoms that caused impairment” (p. 84). Inclusion of an impairment criterion for age at onset is essential because, as discussed by Gordon et al. (26) , the symptoms of ADHD can occur in the absence of impairment, so ignoring impairment will lead to false positive diagnoses (27) .
An alternative interpretation of our findings is that DSM-IV age at onset for ADHD is correct but that, because of recall biases, patients who actually have an onset before age 7 report their ages at onset to be greater than 7. If that idea is correct, then increasing the reliability of the age-of-onset assessment should decrease evidence for the validity of late-onset ADHD. The reliability of an age-at-onset assessment could be increased by using multiple informants or by selecting adult subjects from prospective follow-up studies. Although our study cannot determine if such a bias exists, data from longitudinal follow-up studies would be able to make that determination.
Our analysis of treatment histories showed that 39% of adults with full ADHD and 59% of adults with late-onset ADHD had never been treated for ADHD, and only 58% of the group with full ADHD and 32% of the late-onset group had ever been pharmacologically treated. Current rates of treatment were even lower: 17% for full ADHD and 10% for late-onset ADHD. Similar findings have been reported in both referred (18 , 28) and nonreferred (29) groups of adults with ADHD. In the National Comorbidity Study, only 10.9% of the adults with ADHD had received treatment for ADHD in the 12 months before the interview (25) . Among the subthreshold patients with ADHD, 19% had received pharmacotherapy for ADHD at some time in their lives, and 15% were currently being treated. Although this suggests that the clinicians treating these patients viewed their subthreshold symptoms as clinically significant, given the dearth of evidence for the validity of this subgroup, it raises questions about the appropriateness of such treatment.
Limitations
Because our study group was referred for ADHD, our results cannot be generalized to nonreferred samples. The work by Mannuzza et al. (30) suggested that any retrospective diagnosis of ADHD in adults should be used cautiously in epidemiological studies and primary care settings. The authors followed 176 children with ADHD and 168 children known to not have ADHD in childhood to a mean age of 25. Eleven percent of the subjects from the group without ADHD were retrospectively diagnosed as having had ADHD in childhood. The authors concluded that retrospective diagnoses might yield many false positive results among adults not referred for ADHD.
The diagnoses of adult ADHD relied entirely on the self-report of adult subjects. Although this method allowed us to evaluate the validity of retrospective self-reports, these findings may not generalize to diagnoses defined by using data from informants. As Barkley et al. (31) showed in a study of ADHD youth followed into adulthood, informant reports can boost the validity of diagnosing ADHD in adulthood. Another limitation to the generalizability of our results is that our group was skewed toward Caucasian participants and was not representative of lower socioeconomic strata.
Despite these limitations, by using converging evidence from multiple domains in a family study design, we can reasonably conclude that there is only modest evidence for the validity of adult ADHD for subjects who report a lifetime history of some ADHD symptoms that fail to meet DSM-IV’s threshold for diagnosis. Much more work is needed to better understand the nature of this subgroup and how it should be defined. Regarding the age at onset of ADHD, our data suggest that DSM-IV’s age-at-onset criterion is too stringent for the diagnosis of adults. Although this requires more research, clinicians should not dismiss the diagnosis of ADHD in adults when onset occurs later than allowed by DSM-IV, especially when the age at onset is no later than age 12. As McGough and Barkley (5) concluded, clinicians should be flexible when applying the current DSM criteria for ADHD to adults. Our findings and those of others discussed should be taken into consideration in planning field trials for future revisions of DSM.
1. Adler LA, Chua HC: Management of ADHD in adults. J Clin Psychiatry 2002; 63:29–35Google Scholar
2. Murphy P, Schachar R: Use of self-ratings in the assessment of symptoms of attention deficit hyperactivity disorder in adults. Am J Psychiatry 2000; 157:1156–1159Google Scholar
3. Faraone SV, Biederman J, Feighner JA, Monuteaux MC: Assessing symptoms of attention deficit hyperactivity disorder in children and adults: which is more valid? J Consult Clin Psychol 2000; 68:830–842Google Scholar
4. Faraone SV, Spencer T, Montano CB, Biederman J: Attention deficit hyperactivity disorder in adults: a survey of current practice in psychiatry and primary care. Arch Intern Med 2004; 164:1221–1226Google Scholar
5. McGough JJ, Barkley RA: Diagnostic controversies in adult attention deficit hyperactivity disorder. Am J Psychiatry 2004; 161:1948–1956Google Scholar
6. Schaughency E, McGee R, Raja SN, Feehan M, Silva PA: Self reported inattention, impulsivity and hyperactivity at ages 15 and 18 in the general population. J Am Acad Child Adolesc Psychiatry 1994; 33:173–184Google Scholar
7. Rohde LA, Biederman J, Zimmermann H, Schmitz M, Martins S, Tramontina S: Exploring ADHD age-of-onset criterion in Brazilian adolescents. Eur Child Adolesc Psychiatry 2000; 9:212–218Google Scholar
8. Willoughby MT, Curran PJ, Costello EJ, Angold A: Implications of early versus late onset of attention-deficit/hyperactivity disorder symptoms. J Am Acad Child Adolesc Psychiatry 2000; 39:1512–1519Google Scholar
9. Applegate B, Lahey B, Hart E, Biederman J, Hynd G, Barkley R, Ollendick T, Frick P, Greenhill L, McBurnett K, Newcorn J, Kerdyk L, Garfinkel B, Waldman I, Shaffer D: Validity of the age of onset criterion for attention-deficit/hyperactivity disorder: a report from the DSM-IV field trials. J Am Acad Child Adolesc Psychiatry 1997; 36:1211–1221Google Scholar
10. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983–987Google Scholar
11. First M, Spitzer R, Gibbon M, Williams J: Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC, American Psychiatric Press, 1997Google Scholar
12. Orvaschel H: Schedule for Affective Disorders and Schizophrenia for School-Age Children Epidemiologic Version. Ft Lauderdale, Fla, Nova Southeastern University, Center for Psychological Studies, 1994Google Scholar
13. Leckman JF, Sholomskas D, Thompson D, Belanger A, Weissman MM: Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982; 39:879–883Google Scholar
14. Biederman J, Mick E, Faraone SV: Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry 2000; 157:816–818Google Scholar
15. Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, March JS, Arnold LE, Cantwell DP, Conners CK, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Pelham WE, Severe JB, Swanson JM, Wells KC, Wigal T, Vitiello B: ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 2001; 40:147–158Google Scholar
16. Biederman J, Faraone SV, Lapey K: Comorbidity of diagnosis in attention deficit hyperactivity disorder (ADHD). Child Adolesc Psychiatr Clin North Am 1992; 1:335–360Google Scholar
17. Hesslinger B, Tebartz van Elst L, Mochan F, Ebert D: Attention deficit hyperactivity disorder in adults: early vs late onset in a retrospective study. Psychiatry Res 2003; 119:217–223Google Scholar
18. Biederman J: Impact of comorbidity in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry 2004; 65:3–7Google Scholar
19. Mannuzza S, Gittelman-Klein R, Horowitz-Konig P, Giampino TL: Hyperactive boys almost grown up: IV: criminality and its relationship to psychiatric status. Arch Gen Psychiatry 1989; 46:1073–1079Google Scholar
20. Fischer M, Barkley RA, Smallish L, Fletcher K: Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnorm Child Psychol 2002; 30:463–475Google Scholar
21. Barkley R: Driving impairments in teens and adults with attention-deficit/hyperactivity disorder. Psychiatr Clin North Am 2004; 27:233–260Google Scholar
22. Fischer M, Barkley RA, Edelbrock CS, Smallish L: The adolescent outcome of hyperactive children diagnosed by research criteria: II: academic, attentional, and neuropsychological status. J Consult Clin Psychol 1990; 58:580–588Google Scholar
23. Murphy K, Barkley R: Prevalence of DSM-IV symptoms of ADHD in adult licensed drivers: implications for clinical diagnosis. J Atten Disord 1996; 1:147–161Google Scholar
24. Heiligenstein E, Conyers LM, Berns AR, Miller MA: Preliminary normative data on DSM-IV attention deficit hyperactivity disorder in college students. J Am Coll Health 1998; 46:185–188; erratum, 46, 213Google Scholar
25. Kessler RC: Prevalence of adult ADHD in the United States: results from the National Comorbidity Survey Replication (NCS-R), in 2004 Annual Meeting Syllabus and Proceedings Summary. Arlington, Va, American Psychiatric Association, p 6Google Scholar
26. Gordon M, Antshel K, Faraone S, Barkley R, Lewandowski L, Hudziak JJ, Biederman J, Cunningham C: Symptoms versus impairment: the case for respecting DSM-IV’s criterion D. J Atten Disord 2006; 9:465–475Google Scholar
27. Faraone SV, Sergeant J, Gillberg C, Biederman J: The worldwide prevalence of ADHD: is it an American condition? World Psychiatry 2003; 2:104–113Google Scholar
28. Shekim W: Comprehensive evaluation of attention deficit disorder: residual type. Compr Psychiatry 1989; 31:416–425Google Scholar
29. Zametkin AJ, Nordahl TE, Gross M, King AC, Semple WE, Rumsey J, Hamburger S, Cohen RM: Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990; 323:1361–1366Google Scholar
30. Mannuzza S, Klein RG, Klein DF, Bessler A, Shrout P: Accuracy of adult recall of childhood attention deficit hyperactivity disorder. Am J Psychiatry 2002; 159:1882–1888Google Scholar
31. Barkley RA, Fischer M, Smallish L, Fletcher K: The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol 2002; 111:279–289Google Scholar