Social Adversity in Childhood and the Risk of Developing Psychosis: A National Cohort Study
Abstract
OBJECTIVE: There is conflicting evidence concerning the association of social childhood factors and subsequent psychosis. Previous studies have had inadequate designs. The aim of the present study was to describe a broad range of social factors during childhood and the risk of developing psychosis later in life in a national cohort. METHOD: The study population consisted of all children born in Sweden in 1963–1983—2.1 million persons—in family households participating in the national census of 1970, 1980, 1985, or 1990. Hazard ratios were estimated for five different indicators of socioeconomic position (living in rented apartments, low socioeconomic status, single-parent households, unemployment, and households receiving social welfare benefits) from hospital admissions for schizophrenia and other psychoses during 1987–2002. RESULTS: Increased age- and sex-adjusted hazard ratios for schizophrenia and other psychoses were found for all childhood socioeconomic indicators, ranking from lowest to highest hazard ratio: rented apartments, low socioeconomic status, single-parent households, unemployment, and households receiving social welfare benefits. Hazard ratios increased with an increasing number of adverse social factors present. Those with four measures of adversity had a 2.7-fold higher risk of schizophrenia than those with none. CONCLUSIONS: The results indicate that social adversity in childhood and fetal life is independently associated with the risk of developing schizophrenia and other psychoses later in life. The risks increased with an increasing number of exposures, suggesting a dose-response relationship.
Schizophrenia and other psychoses cause much suffering and have disabling effects. Psychotic illnesses often lead to long periods of absence from work, inability to keep a job, and difficulty in finding employment—all which are costly both to the community and to the person with the illness. The etiology of schizophrenia is still largely unknown.
Several studies in the 1930s–1960s have consistently shown that schizophrenia is more frequent in economically disadvantaged groups (1–4). A serious disorder, such as schizophrenia, will undoubtedly have an effect on a person’s life situation (5), and it is uncertain whether the association between social class and schizophrenia is a consequence of the disorder itself, leading to a drift down the social class scale, or an etiological factor increasing the risk of developing schizophrenia and other psychoses. According to the social-causation hypothesis, social adversity implies a larger stress in life and limited resources to cope with stress, and this could cause psychosis in genetically vulnerable individuals. How social factors are related to psychosis is important to understand—both from a scientific point of view and for preventive purposes.
For decades, etiological research interest in social factors has been virtually absent, but the issue has gained renewed interest (6, 7). Several researchers have studied the association with social class at birth to avoid studying only the effect of the illness. Some of these studies supported the theory of social drift (8), and some showed support for the social-causation hypothesis (9–11). Among the latter, some found an association of an increased risk for schizophrenia with high social class (10), others with middle class (8), and yet others with low social class (9, 11). In the largest study, with 352 patients with schizophrenia, no association was found between lower social class at birth and schizophrenia (12).
Most studies have used the father’s occupation grouped into social class (socioeconomic status) as the only indicator of social adversity in childhood, which may be an incomplete measurement. One study (11) used two indicators: paternal social class and birth in deprived areas. The choice of social indicators is, of course, important (13). Social class includes several different social aspects, such as income, employment possibilities, occupational position, and choice of living accommodations. Many of the studies also failed to take into account alternative explanations, i.e., possible confounders (e.g., migration, psychosis in a parent, and urban birth). Some study groups were too small to detect modest effect sizes. Thus, methodological problems (study size, few indicators of social adversity, and lack of adjustment for confounders) may explain the contradictory results published so far.
To study if social factors contribute to the risk of developing schizophrenia and other psychoses, a large cohort of 2.1 million Swedish children born in 1963–1983 were followed in the national inpatient discharge register from 1987 to 2002 and linked to the national census from 1970 to 1990. Five social indicators during childhood were included in the analysis: parental socioeconomic status, adults in the household receiving social welfare benefits, parental unemployment, single-parent household, and housing situation. Several possible confounders were taken into account.
Method
Study Population
This study was based on data from the national registers held by the Swedish National Board of Health and Welfare and Statistics Sweden that were linked through each individual’s unique personal identification number.
A cohort of 2.1 million children born in 1963–1983 and living in family households identified in the Swedish Population and Housing Census of 1970, 1980, 1985, or 1990 were linked to the inpatient discharge register from 1987 to 2002. Children without identifiable parents and foreign adopted children were excluded because of missing data for biological parents. To use social variables in early childhood, children born in 1963–1968 were linked to the census of 1970 (1980 for single-parent households and socioeconomic status); children born in 1969–1977 were linked to the census of 1980; and children born in 1978–1983 were linked to the census of 1985. Social welfare benefits, only available for 1990, were linked to children born in 1973–1983. Paternal age was dichotomized into ≥40 years or younger than 40.
Social Indicators of Childhood Adversity and Demographic Data
The five investigated indicators (living in rented apartments, low socioeconomic status, single-parent households, unemployment, and households receiving social welfare benefits) were created by linkage to the following registers:
| 1. | Swedish Population and Housing Census of 1970, 1980, and 1985: sex, year of birth, country of birth, single-parent household, employment, socioeconomic status of the household, housing (coded as rent apartment, own apartment, or own house), and geographic location of the home (urbanicity) (coded as metropolitan, town, or rural) were used. Socioeconomic status was defined according to a classification used by Statistics Sweden, which is based on occupation but also takes educational level of occupation, type of production, and position at work of the head of the household into account (14). Workers were divided into blue collar (unskilled and skilled employees in goods and services production: socioeconomic status 11, 12, 21, or 22), white collar (assistant nonmanual employees, intermediate-level executives, and upper-level executives: socioeconomic status 33–36, 40–49, 50–59, or 60), farmers and self-employed professionals (socioeconomic status 79 or 89), and unclassified (unemployment or a nonclassified occupation). Single-parent household and socioeconomic status were available for the years 1980 and 1985. | ||||
| 2. | Total Enumeration Income Survey for 1990: whether social welfare benefits were received. This variable was used only for the birth cohort 1973–1983 to avoid measuring situations in adulthood since people born in 1955–1972 were 18–35 years old in 1990. | ||||
A combined measure of the number of adverse social factors present was created, including unclassified socioeconomic status, living in a rented apartment, single-parent household, and parental unemployment.
Hospital Discharge Variables
Dichotomized outcome variables (at least once/never) were obtained through individual records linkage to the National Hospital Discharge Register from January 1987 to December 2002:
| 1. | Schizophrenia was defined by a main diagnosis of 295, excluding 295E, 295F, and 295H (ICD-9) in 1987–1996 and F20 (ICD-10) in 1997–2002. | ||||
| 2. | “Other psychoses” were defined by 1) a main diagnosis of 295E, 295F, 295H, or 297–298, excluding 298A (ICD-9), in 1987–1996 and F21–29 (ICD-10) in 1997–2002 and 2) no hospital discharge that fulfilled the criteria of schizophrenia, as defined in variable 1. | ||||
| 3. | To define psychosis in parents, the biological parents of the youth study group were identified in the multigenerational register held by Statistics Sweden and linked to hospital discharges with a diagnosis of 295, 297, or 298, excluding 298A (ICD-9), in 1987–1996 and F20–29 (ICD-10) in 1997–2002. | ||||
| 4. | For substance abuse in parents, alcohol abuse was defined as a main or contributory diagnosis of codes 291, 303, 305A, 357F, 425F, 535D, or 571A–571D (ICD-9) in 1987–1996 or F10, K70, G621, I426, or K294 (ICD-10) in 1997–2002. Drug abuse was defined as a main or contributory diagnosis of 292, 304, 965A, 968F, 969G, or 969H (ICD-9) in 1987–1996 or F11, F12, F14, F16, F19, T40, Z503, or Z722 (ICD-10) in 1997–2002. | ||||
Statistical Methods
Hazard ratios with 95% confidence intervals (CIs) were estimated by multivariate Cox proportional hazards models of time in the study with schizophrenia and other psychoses as the outcome variables. Time in the study was calculated with the date of first hospital admission from the National Hospital Discharge Register and the date of death from the National Cause of Death Register. The starting date was Jan. 1, 1987, and the ending date was the date of diagnoses, the date of death, or Dec. 31, 2002—whichever came first. The birth year was entered as a continuous variable in the regression models. Other variables were entered as categorical variables into the models. Population-attributable fractions were calculated according to the following formula: p(hazard ratio–1)÷p(hazard ratio–1)+1, where p was the proportion of the population with exposure. Adjusted hazard ratios were used. Logistic regression was used to study the association between social adversity and possible confounders. The SPSS software package, version 11.5, was used in all statistical analyses (SPSS, Inc., Chicago).
Results
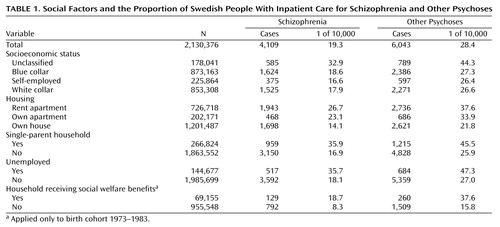
Table 1 shows the number of people with schizophrenia and other psychoses. The diagnosis of schizophrenia as well as other psychoses was more frequent among children from households with more adverse social grouping. Schizophrenia was, for instance, more frequent (18.7 of 10,000) among children from households that received social welfare benefits than in children from households without social welfare benefits (8.3 of 10,000). The cumulative rates for other psychoses were 37.6 of 10,000 and 15.8 of 10,000, respectively.
An analysis of possible confounders revealed higher risks for schizophrenia and other psychoses in association with urbanicity (for schizophrenia, hazard ratio=1.3, 95% CI=1.2–1.5; for other psychoses, hazard ratio=1.3, 95% CI=1.2–1.4), parental inpatient care for substance abuse (for schizophrenia, hazard ratio=1.7, 95% CI=1.5–2.0; for other psychoses, hazard ratio=1.9, 95% CI=1.7–2.2), foreign-born parents (for schizophrenia, hazard ratio=2.1, 95% CI=1.9–2.2; for other psychoses, hazard ratio=1.7, 95% CI=1.6–1.8), and paternal age (for schizophrenia, hazard ratio=1.4, 95% CI=1.3–1.5; for other psychoses, hazard ratio=1.3, 95% CI=1.2–1.4). The highest risk was found in association with parental inpatient care for psychosis (for schizophrenia, hazard ratio=8.4, 95% CI=7.1–9.9; for other psychoses, hazard ratio=6.1, 95% CI=5.2–7.1). These possible confounders all covaried with social adversity; the odds ratio for urbanicity was 2.3 (95% CI=2.3–2.3); for foreign-born parents, it was 3.3 (95% CI=3.2–3.3); for paternal age, it was 1.2 (95% CI=1.2–1.2); for parental psychosis, it was 3.4 (95% CI=3.3–3.6); and for parental alcohol/drug abuse, it was 3.6 (95% CI=3.5–3.7). Consequently, we adjusted for these possible confounders in the following analyses.
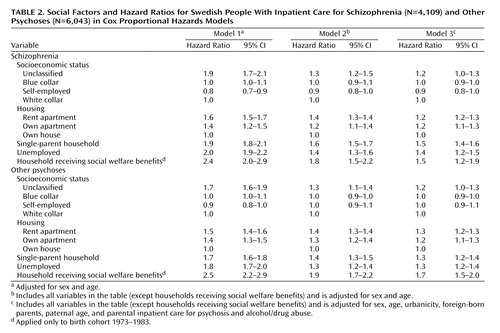
The hazard ratios for schizophrenia and other psychoses associated with social factors were adjusted for sex and age, as well as for possible confounders, and are presented in Table 2. The hazard ratios for schizophrenia associated with the social risk factors varied from 1.6 (95% CI=1.5–1.7) to 2.4 (95% CI=2.0–2.9) in the first regression model, with adjustment for sex and age. In the second model, where the social factors were adjusted for each other (in addition to sex and age), the hazard ratios were somewhat reduced. The third model, which added adjustments for possible confounders—urbanicity, foreign-born parents, paternal age, and parental inpatient care for psychosis and alcohol/drug abuse—again showed slightly reduced hazard ratios but was still statistically significant for most social factors: renting apartments, unemployment, single-parent households, and households receiving social welfare benefits.
The hazard ratios for other psychoses and social risk factors varied between 1.5 (95% CI=1.4–1.6) and 2.5 (95% CI=2.2–2.9) (Table 2), thus at a slightly lower level than for schizophrenia. The second model showed the same reduction pattern in hazard ratios for other psychoses as for schizophrenia. The third model—with adjustments for urbanicity, foreign-born parents, paternal age, and parental inpatient care for psychosis and alcohol/drug abuse—again showed slightly reduced hazard ratios that were still statistically significant for all social factors except unclassified socioeconomic status.
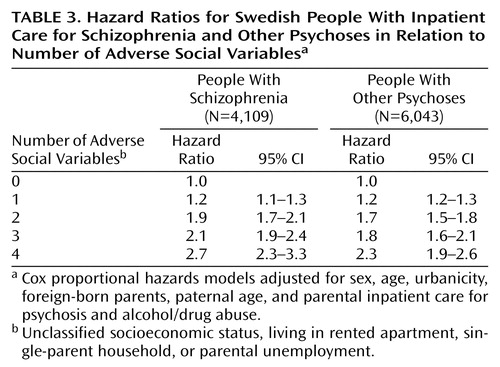
To study the increase in risk of schizophrenia and other psychoses with increasing levels of adverse exposures in childhood, a measurement of the number of present adverse social factors was created, varying from 0 to 4 (the social welfare benefits variable was excluded because it was only available for income year 1990 and was thus only applicable to birth cohort 1973–1983). Table 3 shows increasing hazard ratios for each added adverse social factor. This pattern applied to schizophrenia as well as to other psychoses.
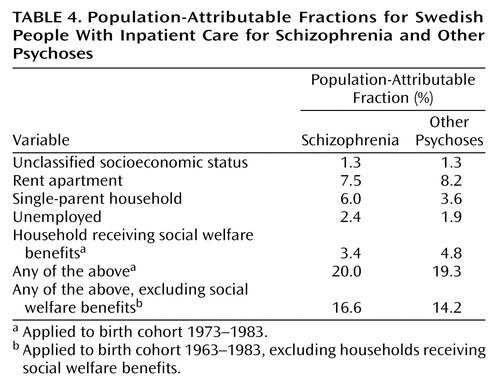
Population-attributable fraction is defined as the proportion of cases in the population that would be avoided if the risk factor were abolished, assuming it to be causally related to disease risk. Attributable fractions were calculated by using significant hazard ratios from model 3, representing an independent factor. Exploring the importance of all social factors combined (15) resulted in population-attributable fractions of 20.0% in the case of schizophrenia and 19.3% in the case of other psychoses (Table 4).
Discussion
In this large national population-based cohort study of two generations and taking several possible confounders into account, we found that a number of social factors related to the parental socioeconomic situation were associated with an increased risk of schizophrenia (hazard ratio=1.2–1.5) and other psychoses (hazard ratio=1.3–1.7). In addition, a stronger association was found with an increasing number of exposures indicative of a dose-response relationship.
Earlier studies, including only the father’s occupation (grouped into socioeconomic status) as an indicator of social adversity, have shown contradictory results (8–12). This study shows that only the socioeconomic status group associated with an increased risk of schizophrenia and other psychoses was the unclassified group, and this effect was no longer significant after adjustment for the various confounders. Thus, in that aspect, our study is in accordance with others.
To our knowledge, this is the first study of schizophrenia that has used several different measurements of social adversity during childhood. The analysis enables us to distinguish between the effects of different social factors, and the majority seem to be independently associated with an increased risk of schizophrenia and other psychoses (rented apartments, single-parent households, parental unemployment, and households receiving social welfare benefits) (model 2, Table 2). It is difficult to assess what the different independent aspects of the social factors represent in a register study like the present one. They are all indirect measures of a social position that is a complex sociological construct. Further research with a more qualitative design is needed to elucidate the mechanisms underlying the observed patterns of association.
However, some of the effect was shared (model 2, Table 2). The social factors—single-parent household, parental unemployment, and receiving social welfare benefits—all represent a situation of exclusion. Maybe it is not the gradient of socioeconomic position but rather the adverse/excluding situations that influence the risk of developing schizophrenia and other psychoses. The only group of the socioeconomic status classification that represents a situation of social exclusion is the unclassified group (unemployed and nonclassified occupations). The other socioeconomic status groups consist of people actually having an occupation and therefore may not be an appropriate measure to use in studies of social risk factors. Social exclusion has been associated with mental illness (16), as have other kinds of discrimination, such as skin color, age, gender, and disability, etc. (17, 18). The size of minority groups has also been associated with schizophrenia, with a greater incidence of schizophrenia among people of ethnic minorities (19). Social adversity/exclusion could lead to isolation, alienation, and a stressful life situation. In a stressful life situation, there may also be fewer opportunities for social support. In genetically vulnerable individuals, these situations could be of significance in developing schizophrenia and other psychoses. One explanation among several is the possibility of deleterious effects by increased levels of the stress hormone cortisol. The individual vulnerability to cortisol levels may, in turn, be genetically determined (20).
There are other possible mediating pathways. The role of urbanicity, immigration, and paternal age, which we were able to adjust for, do not seem to explain our result (model 3, Table 2), nor do parental psychotic illness, although a genetic component cannot be excluded. This also applies to substance abuse, although the effect may be underestimated because of a lack of contact with inpatient care for part of this diagnostic group. All indicators of social adversity in this study were measurements in childhood (linkage from censuses from 1970 to 1990), but it is likely that there is a strong correlation between exposure in early childhood and exposure in utero. We were not able to adjust for obstetric complications (21, 22), maternal stress (23), and infections (24, 25). Thus, mediating factors acting throughout fetal life and birth cannot be excluded.
The causal direction of the association always has to be interpreted cautiously. Goldberg and Morrison (3) even suggested that social drift could include a change in generations through hereditary factors. This study included two generations, and when the risk in the second generation was adjusted for psychotic illness and substance abuse in the parental generation, the effects were quite marginal (Table 2). This is not what would be expected if social drift explained the major effects of the social factors on the risk of schizophrenia in this study. By studying exposure to social factors in childhood and adjusting for parental psychotic illness and substance abuse, the effect of drift from parents was minimized. It is unlikely that the associations between social factors and schizophrenia can be explained by drift from grandparents alone.
Assuming that the relationship between schizophrenia and other psychoses and the social factors are causal (regardless of underlying mediating factors), about 20% of the cases of schizophrenia and 19% of the cases of other psychoses could be attributed to adverse social exposure. This causal assumption can, of course, not easily be made, so the proportion of attribution has to be interpreted with caution. Earlier studies of obstetric complications and schizophrenia have estimated the attributable risk at 11%–27% (26). A Danish study of the effect of place and season of birth on schizophrenia (27) revealed attributable fractions of 6% for hereditary factors (schizophrenia in a parent or a sibling), 10% for season of birth, and 35% for urban birth. Thus, in comparison, social factors maybe significant factors to be considered.
Other Methods Issues
Even though this study included several different social indicators, the social indicators were unspecific, and the age at the time of exposure varied. We were not able to study the duration of exposure. Therefore, the effects of adverse social exposure could be underestimated. However, we did have the opportunity to study the number of exposures. The result showed a stronger association between adverse social factors and schizophrenia, as well as other psychoses, with increasing numbers of exposures. We relied upon register-based clinical diagnoses of schizophrenia and other psychoses, but the validity of the diagnosis in Sweden is high. Two studies have found that about 85% of the cases fulfilled DSM-III (28) and DSM-IV (29) criteria for schizophrenia.
In conclusion, this national population-based cohort study of two generations showed increased risks for schizophrenia and other psychoses in children from less-advantaged households, thus indicating that social adversity in childhood or fetal life contributes to the risk of developing schizophrenia.
 |
 |
 |
 |
Received July 12, 2004; revision received Oct. 6, 2004; accepted Nov. 8, 2004. From the Unit of Epidemiology, Stockholm Centre for Public Health; the Department of Public Health Sciences, Karolinska Institutet, Stockholm; the Centre for Epidemiology, National Board of Health and Welfare, Stockholm; the Department of Children and Women’s Health, Uppsala University, Uppsala, Sweden; and the Department of Social Medicine and the Department of Community Based Medicine, University of Bristol, U.K. Address correspondence and reprint requests to Ms. Wicks, Unit of Epidemiology, Stockholm Centre for Public Health, Norrbacka, Floor 5, 171 76 Stockholm, Sweden; [email protected] (e-mail). Supported by a grant from the Swedish Council for Working Life and Social Research, project number 2003-0376.
1. Faris REL, Dunham HW: Mental Disorder in Urban Areas. Chicago, University of Chicago Press, 1939Google Scholar
2. Hare E: Mental illness and social conditions in Bristol. J Ment Sci 1956; 102:349–357Crossref, Medline, Google Scholar
3. Goldberg EM, Morrison SL: Schizophrenia and social class. Br J Psychiatry 1963; 109:785–802Crossref, Medline, Google Scholar
4. Jablensky A: The epidemiological horizon, in Schizophrenia, 2nd ed. Edited by Hirsch SR, Weinberger D. Boston, Blackwell Publishing, 2003, pp 203–231Google Scholar
5. Agerbo E, Byrne M, Eaton WW, Mortensen PB: Marital and labor market status in the long run in schizophrenia. Arch Gen Psychiatry 2004; 61:28–33Crossref, Medline, Google Scholar
6. Cohen CI: Poverty and the course of schizophrenia: implications for research and policy. Hosp Community Psychiatry 1993; 44:951–958Abstract, Google Scholar
7. Van Os J, McGuffin P: Can the social environment cause schizophrenia? Br J Psychiatry 2003; 182:291–292Crossref, Medline, Google Scholar
8. Timms D: Gender, social mobility and psychiatric diagnoses. Soc Sci Med 1998; 46:1235–1247Crossref, Medline, Google Scholar
9. Castle DJ, Scott K, Wessley S, Murray RM: Does social deprivation during gestation and early life predispose to later schizophrenia? Soc Psychiatry Psychiatr Epidemiol 1993; 28:1–4Crossref, Medline, Google Scholar
10. Makikyro T, Isohanni M, Monny J, Oja H, Hakku H, Jones P, Rantakallio P: Is a child’s risk of early onset schizophrenia increased in the highest social class? Schizophr Res 1997; 23:245–252Crossref, Medline, Google Scholar
11. Harrison G, Gunnell D, Glazebrook C, Page K, Kwiecinski R: Association between schizophrenia and social inequalities at birth: case-control study. Br J Psychiatry 2001; 179:346–350Crossref, Medline, Google Scholar
12. Mulvany F, O’Callaghan E, Takei N, Byrne M, Fearon P, Larkin C: Effect of social class at birth on risk and presentation of schizophrenia: case-control study. BMJ 2001; 323:1398–1401Crossref, Medline, Google Scholar
13. Manor O, Matthews S, Power C: Comparing measures of health inequalities. Soc Sci Med 1997; 45:761–771Crossref, Medline, Google Scholar
14. Socio-Economic Classification (SEI). Stockholm, Statistics Sweden, 1982Google Scholar
15. Gustavsson P, Ahlbom A, Andersson T, Scheele P: Calculations of fractions of lung cancer incidence attributable to occupational exposure to asbestos and combustion products in Stockholm, Sweden. Eur J Epidemiol 2003; 18:937–940Crossref, Medline, Google Scholar
16. Huxley P, Thornicroft G: Social inclusion, social quality and mental illness. Br J Psychiatry 2003; 182:289–290Crossref, Medline, Google Scholar
17. Janssen I, Hanssen M, Bak M, Bijl RV, De Graaf R, Vollenbergh W, McKenzie K, Van Os J: Discrimination and delusional ideation. Br J Psychiatry 2003; 182:71–76Crossref, Medline, Google Scholar
18. Hjern A, Wicks S, Dalman C: Social adversity contributes to high morbidity in psychoses in immigrants—a national cohort study in two generations of Swedish residents. Psychol Med 2004; 34:1025–1033Crossref, Medline, Google Scholar
19. Boydell J, van Os J, McKenzie K, Allardyce J, Goel R, Murray RM: Incidence of schizophrenia in ethnic minorities in London: ecological study into interactions with environment. BMJ 2001; 323:1–4Crossref, Medline, Google Scholar
20. Lightman SL, Insel TR, Ingram CD: New genomic avenues in behavioural neuroendocrinology. Eur J Neurosci 2002, 16:369–372Google Scholar
21. Dalman C, Allebeck P, Cullberg J, Grunewald C, Koster M: Obstetric complications and the risk of schizophrenia: a longitudinal study of a national birth cohort. Arch Gen Psychiatry 1999; 56:234–240Crossref, Medline, Google Scholar
22. Hultman CM, Sparen P, Takei N, Murray R, Cnattingius S: Prenatal and perinatal risk factors for schizophrenia, affective psychosis, and reactive psychosis on early onset: case-control study. BMJ 1999; 318:421–426Crossref, Medline, Google Scholar
23. Van Os J, Selten JP: Prenatal exposure to maternal stress and subsequent schizophrenia: the May 1940 invasion of the Netherlands. Br J Psychiatry 1998; 172:324–326Crossref, Medline, Google Scholar
24. Buka S, Tsuang M, Torrey E, Klebanoff M, Bernstein D, Yolken R: Maternal infections and subsequent psychosis among off-spring. Arch Gen Psychiatry 2001; 58:1032–1037Crossref, Medline, Google Scholar
25. Brown AS, Ezra S: In utero infection and adult schizophrenia. Ment Retard Dev Disabil Res Rev 2002; 8:51–57Crossref, Medline, Google Scholar
26. Dalman C: Early Life Risk Factors for Schizophrenia—Studies of Foetal and Perinatal Complications. Göteborg, Sweden, Göteborg University, Department of Social Medicine, 2001Google Scholar
27. Mortensen PB, Pedersen CB, Westergaard T, Wohlfahrt J, Ewald H, Mors O, Andersen PK, Melbye M: Effects of family history and place of birth and season of birth on the risk of schizophrenia. N Engl J Med 1999; 340:603–608Crossref, Medline, Google Scholar
28. Kristjansson E, Allebeck P, Wistedt B: Validity of the diagnosis schizophrenia in a psychiatric inpatient register. Nord J Psychiatry 1987; 41:229–234Crossref, Google Scholar
29. Dalman C, Broms J, Cullberg J, Allebeck P: Young cases of schizophrenia identified in a national inpatient register: are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol 2002; 37:527–531Crossref, Medline, Google Scholar



