Remission in Depressed Geriatric Primary Care Patients: A Report From the PROSPECT Study
Abstract
OBJECTIVE: This study compared time to first remission for elderly depressed patients in primary care for practices that implemented a care management model versus those providing usual care. In addition, it sought to identify risk factors for nonremission that could guide treatment planning and referral to care managers or specialists. METHOD: Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) data were analyzed. Participants were older patients (≥60 years) selected following screening of 9,072 randomly identified primary care patients. The present analysis examined patients with major depression and a 24-item Hamilton Depression Rating Scale score of 18 or greater who were followed for at least 4 months (N=215). Primary care practices were randomly assigned to offer the PROSPECT intervention or usual care. The intervention consisted of services of trained care managers, who offered algorithm-based recommendations to physicians and helped patients with treatment adherence over 18 months. RESULTS: First remission occurred earlier and was more common among patients receiving the intervention than among those receiving usual care. For all patients, limitations in physical and emotional functions predicted poor remission rate. Patients experiencing hopelessness were more likely to achieve remission if treated in intervention practices. Similarly, the intervention was more effective in patients with low baseline anxiety. CONCLUSIONS: Longitudinal assessment of depression, hopelessness, anxiety, and physical and emotional functional limitations in depressed older primary care patients is critical. Patients with prominent symptoms or impairment in these areas may be candidates for care management or mental health care, since they are at risk for remaining depressed and disabled.
A critical goal in the care of depression is the attainment of remission, defined as an almost asymptomatic state. Patients displaying residual depressive symptoms have functional impairment, compromised quality of life, and high utilization of health care services (1). Moreover, remission is a stable state with a lower risk for relapse than depression improvement, which leaves the patient with residual symptoms (2). While remission is desirable, clinical trials have shown that only a little over one-third of patients treated with antidepressants achieve this clinical state (3). Time to achieve remission has been the focus of studies of psychiatric populations (4), since persisting depression increases suffering, disability, and suicide risk. Remission may be more difficult to achieve in depressed older patients in primary care because of the clinical complexity of this population and the limitations of the primary care setting.
Most depressed older adults are treated by primary care physicians (5). Over 80% of depressed primary care patients prefer to be treated by their primary care physician (6). These preferences might be even stronger among older patients concerned about stigma (7).
Geriatric depression frequently remains inadequately treated in primary care settings. Previous studies have documented that approximately 41% of depressed primary care patients received no antidepressant treatment regardless of age and medical comorbidity (8). While antidepressant prescriptions are rising in primary care practices (9), antidepressants continue to be used at insufficient dosages and for an inadequate length of time (10). Poor treatment adherence by patients further compromises the care of depressed primary care patients (11).
Several health services models have sought to improve the treatment of depression in primary care settings. Training primary care physicians (12), introducing computer-driven decision support (13), and integrating the management of depression with the care of other medical illnesses (14, 15) have had varying success. However, collaborative care of primary care physicians with on-site mental health specialists has enhanced quality of care and improved the outcomes of depression (16).
Recently, the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) compared a primary care-based intervention with usual care in subjects with geriatric depression (17). The intervention relied on “depression care managers” who used operationalized guidelines (18) to provide “on-time and on-target” recommendations to primary care physicians and help patients with treatment adherence. The PROSPECT initial report demonstrated that patients receiving the care management intervention had less severe depressive symptoms and greater remission rates at 4, 8, and 12 months than patients receiving usual care. The initial report included patients with either major or minor depression and a wide range of depression severity (i.e., score >10 on the 24-item Hamilton Depression Rating Scale [19]). The report also did not distinguish patients who achieved first remission from those with a fluctuating course of depression.
The present analysis focuses on the time to first remission for primary care patients experiencing major depression and significant depressive symptom severity. Two hypotheses were tested. The first postulated that patients in primary care practices implementing the PROSPECT intervention would achieve first remission more rapidly than would patients in practices providing usual care. The second hypothesis was that patients with a complex clinical picture, i.e., those with hopelessness and disability, would be less likely to achieve remission. Finally, this analysis sought to identify patients with risk factors for nonremission for whom the intervention was more effective than usual care.
Method
The PROSPECT study compared the outcomes of depressed elderly primary care patients in practices that implemented an intervention based on care management versus practices that offered usual care.
Practices and Participants
Twenty practices participated from three regions: greater New York City, Philadelphia, and Pittsburgh. They were paired within each region by setting (urban, suburban, rural), academic affiliation, size, and racial distribution of patients. Within pairs, practices were randomly assigned to provide either the PROSPECT intervention or usual care. Randomization by practice was chosen in order to reduce “contamination” of usual care by that offered by care managers.
A two-stage sampling generated a representative sample of primary care patients with DSM-IV major or minor depression persisting for at least 1 month. The subject flow has been reported elsewhere (17). Briefly, an age-stratified (60–74 years, ≥75 years) random sample was screened by telephone for depressive symptoms with the Center for Epidemiologic Studies Depression Scale (CES-D Scale) (20) following oral consent. All patients with a CES-D Scale score above 20, those with a history of depression, and a 5% random sample of patients with lower scores were invited to participate. After signing institutional review board-approved consent, patients were interviewed in person according to a protocol (21).
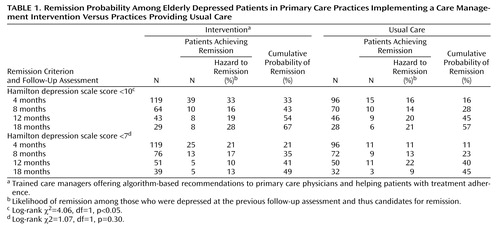
Remission was one of the primary outcomes of the PROSPECT study and was defined as the first occurrence of achieving a Hamilton depression scale score <10. This definition is often used in studies focusing on time to remission of geriatric depression (4) and reflects the concern that elderly patients who no longer have depressive symptoms may still receive Hamilton depression scale score points because of somatic symptoms originating from medical illnesses. Secondary analysis used a second, stricter definition (Hamilton depression scale score <7).
PROSPECT Intervention
The intervention (described elsewhere [17]) was implemented by 15 “care managers,” who used operationalized Agency for Health Care Policy and Research Guidelines (22) to provide appropriately timed and targeted recommendations to physicians. The care managers monitored psychopathology, treatment adherence, response, and side effects and provided follow-up care at predetermined intervals or when clinically necessary. However, the physicians remained responsible for the patients’ clinical care. The first step of the algorithm recommended the selective serotonin reuptake inhibitor citalopram at a target daily dose of 30 mg in order to minimize the likelihood of undertreatment. Patients who refused drug treatment were offered the option to receive interpersonal psychotherapy by the depression care managers; 12.1% of participants in the intervention arm received interpersonal psychotherapy alone. Research funds covered the cost of citalopram and interpersonal psychotherapy but not the cost of other antidepressants or psychotherapy. Covering the cost of citalopram and interpersonal psychotherapy limited the study of cost as a barrier to treatment.
Usual Care
Physicians of “usual care” practices were notified in writing of the patients’ depression diagnosis and contacted by the investigators when the study’s Risk Management Guideline (23) indicated suicide risk in individual patients. Physicians received a videotape and printed material on geriatric depression and treatment guidelines. These measures reduced barriers to recognition of depression.
Systematic Assessment
Depression diagnoses were assigned by trained research assistants after administration of the Structured Clinical Interview for DSM-IV (24) and review of ratings by study psychiatrists. Severity of depression was assessed with the 24-item Hamilton depression scale (19). Suicide ideation was rated with the Scale for Suicide Ideation (25). Interrater reliability and rater drift were monitored throughout the study and have been reported elsewhere (17). Anxiety was quantified with the Clinical Anxiety Scale (26). Hopelessness was assessed with the Beck Hopelessness Scale (27). Cognitive impairment was rated with the Mini-Mental State Examination (28). The Medical Outcomes Study 12-item Short-Form Health Survey (29) was used to assess limitations in functioning due to physical problems (physical component summary) and emotional difficulties (emotional component summary). The intensity of antidepressant pharmacotherapy at entry was quantified by using the Composite Antidepressant Treatment Intensity Scale (30), a 5-point scale modified to include recently introduced antidepressants.
Participants were followed for 18 months; they had telephone assessments at 4, 8, and 18 months and an in-person interview 12 months after entry. Although desirable, it was not feasible to blind the research assistants to the treatment assignments (intervention versus usual care) of the practices.
Data Analysis
Baseline demographic and clinical characteristics were compared by using t tests for continuous variables and chi-square analyses for binary variables. Kaplan-Meier survival analysis was employed to test the significance of differences in the study outcome, time until first remission of depressive symptoms. For the identification of predictors to remission we used mixed effects logistic regression models to fit the outcome with adjustment for months during which the research assessment occurred. This approach is an extension of logistic regression models for grouped survival times, and the random effects accounts for the clustering of primary care practices (31). We used SAS GLIMMIX macro for statistical inference based on penalized quasi-likelihood, which was found more accurate than quadrature implemented in SAS PROC NLMIXED when comparing a small number of large clusters (32). Goodness of fit was measured by the deviance statistic as suggested by Littell et al. (33).
The multivariate models sought to identify groups for which the intervention was more effective than usual care, i.e., to identify predictors for which interaction with the intervention was significant. To this end, we applied a hierarchical backward elimination procedure in which the full model conformed to the “hierarchical principle” (34) and contained all the main effects of the demographic and clinical putative predictors plus their interactions with the treatment assignment.
Results
Participants
The flow of participants has been reported elsewhere (17). Briefly, 16,708 older patients were sampled, and 9,072 were screened for depression with the CES-D Scale. Of the screened patients, 1,888 were invited to enroll in the study, and 1,238 agreed to a baseline interview. Among them, 267 met criteria for major depression and had a Hamilton depression scale score ≥18 at entry. This analysis included only participants (N=215) who at least had been evaluated at the 4-month follow-up visit. Outcomes during the follow-up period were either 1) first instance of remission identified before any missed assessment session; or 2) no instance of remission identified before the first missed appointment. This strategy enabled determination of the most accurate time to remission within the constraints of infrequent follow-up assessments. Time to remission was defined as the time from entry into the study until initially meeting criteria for remission. There were no statistically significant differences in age, gender, race, education, severity of depression, anxiety, cognitive impairment, disability, or intensity of antidepressant treatment at baseline among patients included in this analysis and those who were excluded because of missed follow-up assessments.
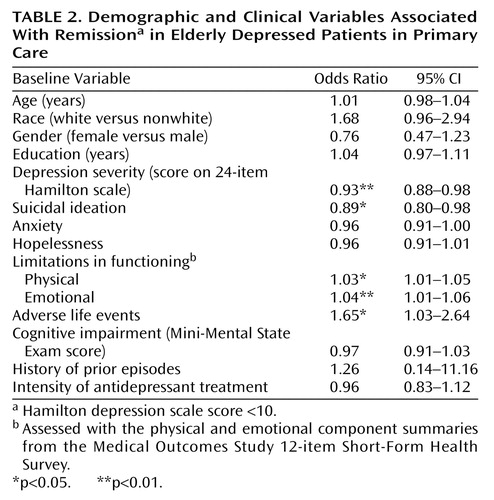
Probability of Remission
When remission was defined as Hamilton depression scale score <10, patients treated by practices implementing the care management intervention had a higher cumulative probability of remission (probability of achieving remission at each follow-up point) than practices offering usual care (Table 1, Figure 1). Similarly, the hazard to remission (likelihood of remission among those were depressed in the previous follow-up assessment and thus candidates for remission) was significantly higher among the intervention than among the usual care patients. When remission was defined as Hamilton depression scale score <7, these differences approximated the less strict remission criteria results but did not reach statistical significance (Table 1, Figure 1).
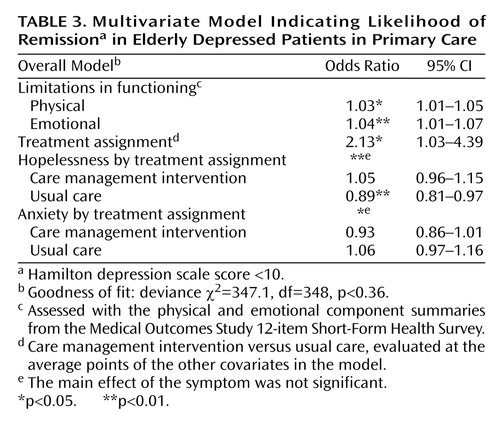
The occurrence of remission differed across the three regions (F=7.03, df=2, 471, p<0.01), but there was no site-by-treatment assignment interaction. Bivariate analysis demonstrated that demographic variables such as age, gender, race, and education were not significantly associated with the occurrence of remission. In contrast, clinical variables such as severity of depression, suicidal ideation, physical and emotional functioning limitations, and adverse life events each were significantly associated with the occurrence of remission (Table 21).
The most parsimonious multivariate model indicated that patients with limitations in physical and emotional aspects of functioning, hopelessness, and anxiety were less likely to achieve remission regardless of treatment assignment (Table 3). Patients experiencing hopelessness were less likely to achieve remission if treated by practices offering usual care. However, hopelessness did not influence the remission rate of patients of the intervention practices (Figure 2). Anxiety interacted with treatment assignment and influenced remission rates (p<0.04). This effect was principally related to the differential efficacy of intervention practices. Nonanxious patients were more likely to achieve remission if treated in intervention than in usual care practices. However, anxious patients of intervention and usual care practices had similar remission rates (Table 3, Figure 3). Inclusion of study site in the model did not influence the relationships of predictor variables to remission.
The three regions differed in rates of remission when defined as Hamilton depression scale score <7 (F=3.54, df=2, 512, p=0.03), but there was no site-by-treatment assignment interaction. The model predicting remission defined as Hamilton depression scale score <10 (Table 3) had a similar goodness of fit in predicting remission defined as Hamilton depression scale score <7 (deviance χ2=305.6, df=384, p<0.99).
Discussion
The principal finding of this analysis is that the PROSPECT intervention was more effective than usual care in promoting remission of depression in elderly primary care patients, especially when remission was defined as a Hamilton depression scale score lower than 10. Differences in remission rates between intervention and usual care were most pronounced among depressed elders experiencing hopelessness. When remission was defined according to stricter criteria, i.e., Hamilton depression scale score less than 7, the intervention group had numerically higher rates of remission during the early phases of treatment but, when the whole 18-month period was taken into consideration, differences in remission rates did not reach significance. Regardless of the remission criterion, depressed patients with comorbid anxiety disorders, hopelessness, and limitations in physical and emotional functioning were associated with low remission rates in primary care elderly patients receiving either the intervention or usual care.
A strength of this study is the use of random sampling and screening that may have resulted in a representative sample of depressed older primary care patients. Therefore, its findings may be relevant to clinical practice. Limitations of the study include the lack of blinding of raters, the infrequent follow-up, the lack of information on discrete medical problems of participants, and the lack of information about specific antidepressant treatments received by each group during the 18 months of the study. While more frequent follow-up assessments would have been desirable, concerns about participant burden and cost led us to select few, yet clinically meaningful, follow-up times. This analysis used disability resulting from physical problems as a proxy of medical burden (the Short-Form Health Survey physical component summary). Data on specific medical disorders and their impact on remission need further attention. Finally, treatment changed frequently both in the intervention and the usual care practices. Future analyses may compare the impact on remission of selected treatments at specific times. Nonetheless, focusing on predictors of the first remission occurrence serves to identify the clinical profile of elderly primary care patients likely to remain depressed and in need of close follow-up and perhaps referral to mental health specialists.
The favorable remission rates of the PROSPECT intervention on depression is consistent with evidence that interventions aimed at changing primary care practice can improve the quality of depression care in mixed-age (14) and elderly (15) patients. Despite differences in design, measurements, and type of intervention, both the PROSPECT and the Improving Mood-Promoting Access to Collaborative Treatment studies (the latter being another study of depressed primary care elders) demonstrated differences in remission rates favoring the intervention over usual care (15). These findings underscore the value of such interventions for resolving late-life depression in primary care patients.
Remission occurred earlier for patients in practices providing the intervention than for those in practices providing usual care. By 8 months, 43% of patients receiving the care management intervention had achieved remission (Hamilton depression scale score <10) compared with 28% of patients receiving usual care. The remission rate with usual care eventually reached the level achieved with the intervention, perhaps reflecting the fact that some depressive episodes eventually subside and those that persist or worsen receive additional attention. These observations suggest that in at least some patients, the use of trained care managers can accelerate remission and perhaps reduce suffering, disability, and family disruption several months earlier than usual care.
Compromised physical and emotional function predicted low remission rates in patients treated by either the intervention or usual care. There is evidence, however, that antidepressant treatment and reduction of depressive symptoms can improve the functional status of elderly patients (35). These observations suggest that older primary care patients with major depression and physical and emotional function limitations need aggressive antidepressant treatment and perhaps referral to mental health professionals if their symptoms persist.
Depressed elderly primary care patients experiencing hopelessness were more likely to benefit from the PROSPECT intervention than usual care. Hopelessness is a set of beliefs that influence how a person interprets information and behaves. Hopeless thoughts can be chronic and persistent in some individuals and activated during depression in others (36). Hopelessness has a strong association with suicidal ideation and behavior in younger adults (37). A similar relationship between hopelessness and suicidal ideation was demonstrated in institutionalized elderly patients and was dependent upon the level of depression (38). Hopelessness was associated with suicidal ideation in patients with severe depression, but there was no significant relationship between hopelessness and suicidal ideation in patients with mild depression. These observations suggest that elderly primary care patients experiencing hopelessness require special clinical attention—and perhaps a referral to care managers—since these patients have a low likelihood for remission under usual care and may even be at increased risk for suicide, especially in the presence of a severe depression. The provision of care management is particularly feasible in large medical practices such as HMOs, which often include behavioral specialists on their staff.
Anxiety adversely influenced the rate of remission in patients of the intervention practices, whereas it had a nonsignificant effect in patients receiving usual care. Specifically, the intervention was more effective than usual care in patients with low anxiety but added little benefit for patients with higher anxiety severity. Patients with comorbid anxiety and depression frequently exhibit more severe symptoms overall, have a more protracted course of illness, and experience less positive treatment outcomes (39). Therefore, care management may be insufficient treatment for some anxious depressed elderly primary care patients, and their physicians should recognize this clinical pattern as one of several warranting referral to a psychiatrist.
Primary care occupies a strategic position in the management of late-life depression. This study has documented that remission of late-life depression occurs in a large percentage of primary care patients. Collaborative care by trained care managers and primary care physicians leads to earlier remission than usual care and can reduce suffering and disability. As many of the care managers’ services are reimbursable under the existing Medicare codes, referral to appropriately trained care managers is feasible. Priority for such services may be given to depressed elders experiencing hopelessness, since usual care is less likely to be helpful. Longitudinal assessment of anxiety and limitations in physical and emotional functioning of depressed older primary care patients is critical. Some patients with prominent impairment in these areas may not achieve remission when treated in primary care settings and may require mental health consultation and care.
 |
 |
 |
Received June 2, 2004; revision received July 15, 2004; accepted July 23, 2004. From the Department of Psychiatry, Weill Medical College of Cornell University, New York; the Departments of Psychiatry and Medicine, University of Pennsylvania, Philadelphia; the Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh; and the Geriatric Research, Education and Clinical Center, VA Pittsburgh Health Care System, Pittsburgh. Address correspondence and reprint requests to Dr. Alexopoulos, Cornell Medical Center–Westchester Division, 21 Bloomingdale Rd., White Plains, NY 10605; [email protected] (e-mail). This work was supported by grants from NIMH (RO1 MH-59366, R01 MH-059380, RO37 MH-51842, RO1 MH-59318, P30 MH-68638, P30 MH-52247, and P30 MH-066270), the Hartford Foundation, and Forest Pharmaceuticals, Inc.
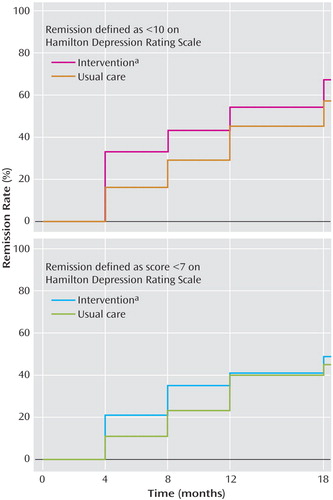
Figure 1. Cumulative Probability of Remission Among Elderly Depressed Primary Care Patients in Practices Implementing a Care Management Intervention Versus Practices Providing Usual Care
aTrained care managers offering algorithm-based recommendations to primary care physicians and helping patients with treatment adherence.
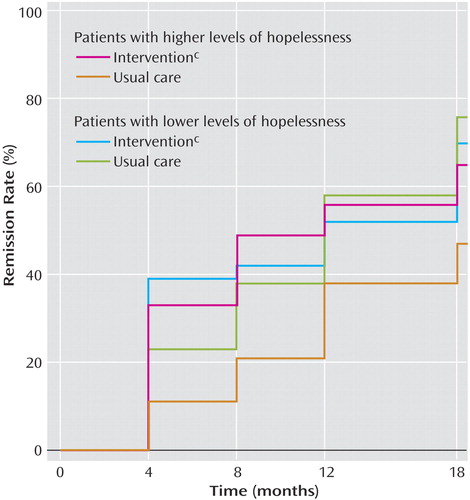
Figure 2. Estimated Probability of Remissiona in Elderly Depressed Primary Care Patients in Practices Implementing a Care Management Intervention Versus Practices Providing Usual Care, by Level of Hopelessnessb
aHamilton depression scale score <10.
bLevel of hopelessness determined by Beck Hopelessness Scale score: those scoring higher than the median were classified as having higher levels of hopelessness.
cTrained care managers offering algorithm-based recommendations to primary care physicians and helping patients with treatment adherence.
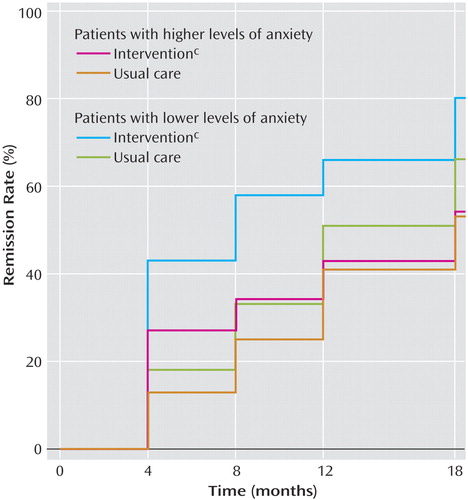
Figure 3. Estimated Probability of Remissiona in Elderly Depressed Primary Care Patients in Practices Implementing a Care Management Intervention Versus Practices Providing Usual Care, by Level of Anxietyb
aHamilton depression scale score <10.
bLevel of anxiety determined by Clinical Anxiety Scale score: those scoring higher than the median were classified as having higher levels of anxiety.
cTrained care managers offering algorithm-based recommendations to primary care physicians and helping patients with treatment adherence.
1. Paykel ES, Ramana R, Cooper Z, Hayhurst H, Kerr J, Barocka A: Residual symptoms after partial remission: an important outcome in depression. Psychol Med 1995; 25:1171–1180Crossref, Medline, Google Scholar
2. Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Paulus MP, Kunovac JL, Leon AC, Mueller TI, Rice JA, Keller MB: Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. J Affect Disord 1996; 50:97–108Crossref, Google Scholar
3. Thase ME, Entsuah AR, Rudolph RL: Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors. Br J Psychiatry 2001; 178:234–241Crossref, Medline, Google Scholar
4. Whyte EM, Dew MA, Gildngers A, Lenze EJ, Bharucha A, Mulsant BH, Reynolds CF III: Time course of response to antidepressants in late-life major depression: therapeutic implications. Drugs Aging 2004; 21:531–554Crossref, Medline, Google Scholar
5. Fortney J, Rost K, Zhang M: A joint choice model of the decision to seek depression treatment and choice of provider sector. Med Care 1998; 36:307–320Crossref, Medline, Google Scholar
6. Brody DS, Khaliq AA, Thompson TL: Patients’ perspectives on the management of emotional distress in primary care. J Gen Intern Med 1997; 12:403–406Crossref, Medline, Google Scholar
7. Leaf PJ, Bruce ML, Tischler GL, Holzer CE: The relationship between demographic factors and attitudes toward mental health services. J Community Psychol 1987; 15:275–284Crossref, Medline, Google Scholar
8. Luber MP, Alexopoulos GS, Hollenberg J, Charlson M, Callahan M: Recognition, treatment, comorbidity, and resource utilization of depressed patients in a general medical practice (abstract). J Gen Intern Med 1996; 11(May suppl):134Google Scholar
9. Harman JS, Mulsant BH, Kelleher KJ, Schulberg HC, Kupfer DJ, Reynolds CF III: Narrowing the gap in the treatment of depression. Int J Geriatr Psychiatry 2001; 31:239–253Crossref, Google Scholar
10. Unützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Tang L, Oishi S: Depression treatment in a sample of 1,801 depressed older adults in primary care. J Am Geriatr Soc 2003; 51:505–514Crossref, Medline, Google Scholar
11. Cramer JA, Rosenheck R: Compliance with medication regimens for mental and physical disorders. Psychiatr Serv 1998; 49:196–201Link, Google Scholar
12. Gilbody S, Whitty P, Grimshaw J, Thomas R: Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA 2003; 289:3145–3151Crossref, Medline, Google Scholar
13. Rollman BL, Hanusa BH, Lowe HJ, Gilbert T, Kapoor WN, Schulberg HC: A randomized trial using computerized decision support to improve treatment of major depression in primary care. J Gen Intern Med 2002; 17:493–503Crossref, Medline, Google Scholar
14. Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, Miranda J, Carney MF, Rubenstein LV: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000; 283:212–220; correction, 283:3204Crossref, Medline, Google Scholar
15. Unutzer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C (IMPACT [Improving Mood-Promoting Access to Collaborative Treatment] Investigators): Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002; 288:2836–2845Crossref, Medline, Google Scholar
16. Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, Bush T, Russo J, Ludman E: Stepped collaborative care for primary care patients with persistent symptoms of depression. Arch Gen Psychiatry 1999; 56:1109–1115Crossref, Medline, Google Scholar
17. Bruce ML, Ten Have TR, Reynolds CF III, Katz IR, Schulberg HC, Mulsant BH, Brown GK, McAvay GJ, Pearson JL, Alexopoulos GS: Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA 2004; 291:1081–1091Crossref, Medline, Google Scholar
18. Depression Guideline Panel: Clinical Practice Guideline Number 2: Treatment of Major Depression, 5: Depression in Primary Care: AHCPR Publication 93–0551. Rockville, Md, US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993Google Scholar
19. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
20. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
21. Raue PJ, Alexopoulos GS, Bruce ML, Klimstra S, Mulsant BH, Gallo JJ (PROSPECT Study Group): The systematic assessment of depressed elderly primary care patients. Int J Geriatr Psychiatry 2001; 16:560–569Crossref, Medline, Google Scholar
22. Mulsant BH, Alexopoulos GS, Reynolds CF, Katz IR, Abrams RC, Oslin D, Schulberg HC (PROSPECT Study Group): Pharmacological treatment of depression in older primary care patients: the PROSPECT algorithm. Int J Geriatr Psychiatry 2001; 16:585–592Crossref, Medline, Google Scholar
23. Brown GK, Bruce ML, Pearson JL: High-risk management guidelines for elderly suicidal patients in primary care settings. Int J Geriatr Psychiatry 2001; 16:593–601Crossref, Medline, Google Scholar
24. First M, Spitzer R, Williams J, Gibbon M: Structured Clinical Interview for DSM-IV—Non-Patient Edition (SCID-NP, Version 1.0). Washington, DC, American Psychiatric Press, 1995Google Scholar
25. Beck AT, Kovacs M, Weissman A: Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol 1979; 47:343–352Crossref, Medline, Google Scholar
26. Snaith RP, Baugh SJ, Clayden AD, Husain A, Sipple MA: The Clinical Anxiety Scale: an instrument derived from the Hamilton Anxiety Scale. Br J Psychiatry 1982; 141:518–523Crossref, Medline, Google Scholar
27. Beck AT, Steer RA, Beck JS, Newman CF: Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide Life Threat Behav 1993; 23:139–145Medline, Google Scholar
28. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
29. Ware J Jr, Kosinski M, Keller SD: A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233Crossref, Medline, Google Scholar
30. Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E: Recovery in geriatric depression. Arch Gen Psychiatry 1996; 53:305–312Crossref, Medline, Google Scholar
31. Ten Have TR, Uttal DH: Subject-specific and population-averaged continuous ratio logit models for multiple discrete time survival profiles. Appl Stat 1994; 43:371–384Crossref, Google Scholar
32. Ten Have TR, Localio AR: Empirical Bayes estimation of random effects parameters in mixed effects logistic regression models. Biometrics 1999; 55:1022–1029Crossref, Medline, Google Scholar
33. Littell RC, Milliken GA, Stroup WW, Wolfinger RD: SAS System for Mixed Models. Cary, NC, SAS Institute, 1996, pp 445–447Google Scholar
34. Kleinbaum DG, Klein M: Logistic Regression: A Self-Learning Text, 2nd ed. New York, Springer, 2002Google Scholar
35. Heiligenstein JH, Ware JE, Beusterien KM, Roback PJ, Beusterian KM, Roback PJ, Andrejasich C, Tollefson GD: Acute effects of fluoxetine versus placebo on functional health and well being in late-life depression. Int Psychogeriatr 1997; 7(suppl):125–137Google Scholar
36. Weishaar ME, Beck AT: Hopelessness and suicide. Int Rev Psychiatry 1992; 4:177–184Crossref, Google Scholar
37. Dyer JAT, Kreitman N: Hopelessness, depression, and suicidal intent in parasuicide. Br J Psychiatry 1984; 144:127–133Crossref, Medline, Google Scholar
38. Uncarper H, Gallagher-Thompson D, Osgood NJ, Bongar B: Hopelessness and suicidal ideation in older adults. Gerontologist 1998; 38:62–70Crossref, Medline, Google Scholar
39. Gorman JM: Comorbid depression and anxiety spectrum disorders. Depress Anxiety 1996; 4:160–168Crossref, Medline, Google Scholar



