The Effect of Parental Alcohol and Drug Disorders on Adolescent Personality
Abstract
OBJECTIVE: The relationship of parental alcohol or drug diagnosis to offspring personality was examined in a population-based sample of 17-year-old twins (568 girls and 479 boys) participating in the Minnesota Twin Family Study. Whether offspring personality characteristics 1) are specific to the type of substance use disorder in parents (alcohol versus drug) and 2) are found in high-risk offspring without substance use disorders as well as in offspring with substance use disorders was investigated. METHOD: Personality was assessed with the Multidimensional Personality Questionnaire; substance use disorders were assessed in person through diagnostic interviews. RESULTS: In both male and female offspring, parental history of alcohol dependence was associated with greater negative emotionality, aggression, stress reaction, and alienation but lower well-being; parental history of drug disorders was associated with lower constraint, control, harm avoidance, and traditionalism but higher social potency. Excluding offspring with a substance use disorder had virtually no effect on the statistical significance of these findings. CONCLUSIONS: In contrast to findings in some adult samples, personality characteristics associated with a family history of substance use disorders are found even in adolescent offspring who have not yet developed these disorders themselves, suggesting that personality might be one indicator of familial risk for substance use disorders during this developmental stage. Personality profiles of offspring of parents with substance use disorders also show some diagnostic specificity, with constraint associated with parental drug abuse and negative emotionality with parental alcoholism.
Alcohol and drug disorders show strong familial transmission (1). Twin studies have consistently demonstrated a substantial genetic component to both alcoholism (2, 3) and illicit drug abuse and dependence (4, 5). An obvious risk factor for a genetically influenced disorder is having a parent with the disorder. Although strong environmental influences have also been implicated by twin research, research in adoptive samples has generally found that being reared by an alcoholic parent does not significantly increase the risk for alcoholism in adopted offspring (6, 7). More research is needed to identify what other characteristics might aid in the early identification of those at risk in order to help prevent the development of these disorders.
Along these lines, it has been suggested that personality might represent a common mediating factor for alcoholism risk due to parental history (8). Like substance use disorders, personality has consistently been found to be moderately heritable (9). Behavioral disinhibition (i.e., novelty-seeking, impulsivity, lack of constraint) and negative emotionality (the tendency to experience negative mood states) are the personality traits most often implicated with alcoholism (10), and there is evidence that common genetic factors may underlie both these personality traits and alcoholism (11). Longitudinal studies have confirmed prospectively that indicators of behavioral disinhibition predict both early onset of substance use (12) and alcohol problems in early adulthood (13), although support for negative emotionality as a prospective predictor of substance use disorders is less consistent (14).
In contrast, a recent report based on 325 probands and 262 of their first-degree adult relatives (15) concluded that personality traits did not constitute familial or heritable risk factors for substance use disorders. Both probands and relatives with alcohol and drug disorders showed personality differences from those without substance use disorders. However, the relatives of probands with substance use disorder diagnoses but who did not have these disorders themselves did not. The sample consisted mostly of middle-aged adults who were beyond the age of risk for developing a substance use disorder. Whether the same lack of personality deviations might be observed in at-risk relatives who were free of substance use disorders at an earlier point in development is not clear.
Furthermore, although both alcohol and drug disorders were included by Swendsen et al. (15), how personality factors might differ based on type of disorder was not a focus of the investigation. Despite the high comorbidity of alcoholism with drug dependence (16), the personality factors that are specific to alcoholism alone or that are due to comorbidity with drug disorders have received little attention. What differentiates these disorders was examined in the parents of twins in the Minnesota Twin Family Study (17). Adults with a history of drug diagnosis, including those with comorbid alcoholism, were found to be low in constraint. However, those with alcoholism alone were not low in constraint but, rather, were high in negative emotionality. These results raise the possibility that previous findings associating behavioral disinhibition with alcoholism may have been due to the subset of alcoholics who abuse other drugs. Whether these specific profiles characterizing alcohol versus drug disorders extend to offspring or were simply a consequence of substance use disorders was not explored.
The present investigation used a large representative sample of older adolescent offspring, careful documentation of substance use disorders by means of direct interview, and a comprehensive measure of personality to ask the following questions:
| 1. | How is a parental alcohol or drug diagnosis related to offspring personality? | ||||
| 2. | Do alcohol and drug disorders in parents confer the same, or different, personality risks to offspring? | ||||
| 3. | Are these relationships primarily found in offspring who already have a substance use disorder, or do high-risk offspring who have not yet developed a substance use disorder also show these personality deviations? | ||||
This last question is particularly crucial because it controls for the possibility that personality traits can be consequences, rather than precursors, of substance use disorders (15). Finally, because alcohol and drug disorders are more prevalent in men than women (18) and personality characteristics are associated with gender (19), gender differences in the relationships just described were also assessed.
Method
The initial sample consisted of 674 girls and 578 boys from 626 twin pairs reared together who visited the Minnesota Twin Family Study with their parents. The Minnesota Twin Family Study is a longitudinal study designed to identify genetic and environmental factors that influence the development of substance abuse and related psychopathology (20). The study used a population-based ascertainment method in which all same-sex twin pairs born in the state of Minnesota in specified years were identified by public birth records, located (current addresses of over 90% of the twin births were established by using various public registries), then recruited to visit when the twins reached either age 11 or 17. For the present investigation, only data from the intake visit of twins in the 17-year-old cohort (mean age at assessment=17.5 years, SD=0.5) were used. Families were excluded from participation if the twins lived more than a day’s drive from Minneapolis, had been adopted, or had a physical or intellectual disability that precluded completing our daylong, in-person assessment. Of the eligible twin families, approximately 17% refused to participate. After a complete description of the study was given, written informed consent was obtained from the parents, and written assents were obtained from the twins.
Among the 626 initial families, all biological mothers and 88% (N=548) of the biological fathers completed an intake assessment. On the basis of responses to a brief telephone or mail survey (completed on over 80% of the ineligible or refusing families), the parents in the participating families differed minimally from the nonparticipants on socioeconomic status indicators (e.g., 0.3 years more education for the participants). They did not differ at all in self-reported rates of psychopathology (see reference 20 for a complete description of the sample and recruitment). Furthermore, because twins are neither systematically different in personality (21) nor in rates of psychopathology (22) from single offspring, the sample should be representative of the population of Minnesota. Mean years of education were 13.7 (SD=1.9) for the mothers and 14.2 (SD=2.3) for the fathers. Consistent with Minnesota demographics for the birth years sampled, 97% of the mothers and fathers were Caucasian.
Diagnostic and Personality Assessment
All twins, mothers, and fathers were interviewed separately at the University of Minnesota by different interviewers (with no knowledge of other family members’ status) regarding a variety of psychological disorders. Interviewers had a B.A. or an M.A. in psychology and went through extensive training and observation. Both parents and twins were assessed for alcohol and illicit drug disorders (i.e., amphetamines, cannabis, cocaine, hallucinogens, inhalants, opiates, phencyclidine, or sedatives) by using a modified version of the expanded substance abuse module of the Composite International Diagnostic Interview (23). For the small number of parents who were unavailable (e.g., because of death) or unwilling to participate (12% of the fathers), substance use disorders in the unavailable parent were assessed by means of spousal report with a modified version of the Family Informant Schedule and Criteria (24). Maternal reports of substance use disorders in the twins were also obtained by using a modified parent version of the Diagnostic Interview for Children and Adolescents (25), and a symptom was considered present if either the mother or twin reported it as present. Lifetime diagnoses based on DSM-III-R criteria (the diagnostic system in use when the Minnesota Twin Family Study began) were determined by teams of two advanced clinical psychology graduate students, and symptoms were assigned based on consensus between the two diagnosticians. Reliability of the consensus diagnoses of substance use disorders was 0.92 or greater (20).
Personality was assessed with the 198-item version of the Multidimensional Personality Questionnaire (26). The Multidimensional Personality Questionnaire is a self-report personality instrument developed through factor analysis to assess a broad range of personality characteristics in normal populations. Internal consistency reliabilities for the Multidimensional Personality Questionnaire range from 0.76 to 0.89, and 30-day test-retest reliabilities range from 0.82 to 0.92. Eleven primary personality characteristics are assessed, and scores on 10 of these scales contribute to scores on three superfactors. Positive emotionality refers to the tendency to view life as essentially a pleasurable experience and to be actively engaged socially. It consists of four primary scales (descriptions of high scorers are in parentheses): well-being (cheerful, feels good about self), social potency (forceful, likes to influence and lead others), achievement (works hard, likes demanding projects), and social closeness (sociable, likes people, affectionate). Negative emotionality, a propensity to experience psychological distress and negative mood states, consists of three primary scales: stress reaction (nervous, easily upset, irritable), alienation (feels mistreated, thinks others intend harm), and aggression (hurts others for own advantage, vindictive). Constraint, a propensity to endorse traditional values, act in a cautious and restrained manner, and avoid thrills, consists of three primary scales: control (reflective, cautious, plans activities), harm avoidance (avoids danger, prefers safer activities), and traditionalism (conservative, endorses high moral standards). The eleventh primary scale of absorption (responsive to sights and sounds) does not load principally on any one superfactor.
The Multidimensional Personality Questionnaire was mailed to the twins before their in-person assessment. If it was not completed by the time of their visit, the twins were asked to complete it at home and return it by mail. A total of 87.7% of the adolescents (1,098 of 1,252) eventually completed the Multidimensional Personality Questionnaire, with slightly higher completion rates among girls (89.6%) than boys (85.5%) (χ2=4.96, df=1, p<0.05). Among the girls, completion rates did not differ significantly between those with (87.4%) and without (90.0%) an alcohol or drug diagnosis (χ2=0.65, df=1, p=0.42). However, consistent with previous findings that men with substance use disorders are less likely to fully participate in studies of psychopathology (27), completion rates in boys were significantly higher among those having neither diagnosis (87.8%) compared to those having either diagnosis (77.3%) (χ2=8.73, df=1, p<0.01).
The 1,047 twins (568 girls and 479 boys) who completed the Multidimensional Personality Questionnaire and for whom complete diagnostic information was available for both parents were used in the analyses. Four groups were formed based on whether one or both parents qualified for either definite DSM-III-R alcohol dependence or definite drug abuse or dependence at some point in their lives:
| 1. | Parents having neither disorder | ||||
| 2. | Parents having alcohol dependence only | ||||
| 3. | Parents having drug abuse/dependence only | ||||
| 4. | Parents having both disorders | ||||
Because in over 70% of the families in which the mother had a substance use disorder the father did as well, it was difficult to examine the effects of the mothers’ diagnoses in isolation (a common problem noted by others [28]). Particularly given our examination here of the effects of type of diagnosis (alcohol or drug), the resulting groups were too small to permit meaningful analysis separately by parent gender.
Statistical Analyses
To account for the clustered twin observations, data were analyzed by means of hierarchical linear models (29) by using PROC MIXED from SAS (30). The three factors were parental alcohol dependence diagnosis (yes/no), parental drug abuse or dependence diagnosis (yes/no), and offspring sex (male or female). Because Multidimensional Personality Questionnaire superfactors are linear weighted composites of the primary scales, two separate multivariate analyses were computed: one with the 11 primary scales as dependent variables and one with the three superfactors as dependent variables.
To determine whether 1) personality characteristics found in offspring of parents with substance use disorders were due to the subset of offspring with substance use disorders themselves or 2) were observable among offspring without substance use disorders as well, the same set of analyses was repeated only with offspring who had never met DSM-III-R criteria for substance abuse or dependence for alcohol or one of eight illicit drugs mentioned earlier. Because maximizing detection of still developing disorders in adolescents is of concern (31), two levels of diagnostic certainty were used for dependence diagnoses: definite equaled all diagnostic criteria satisfied and probable equaled one symptom short of definite. The inclusion of probable cases resulted in identifying 15% of the girls (N=85) and 20% of the boys (N=94) as having developed a definite or probable substance use disorder.
Results
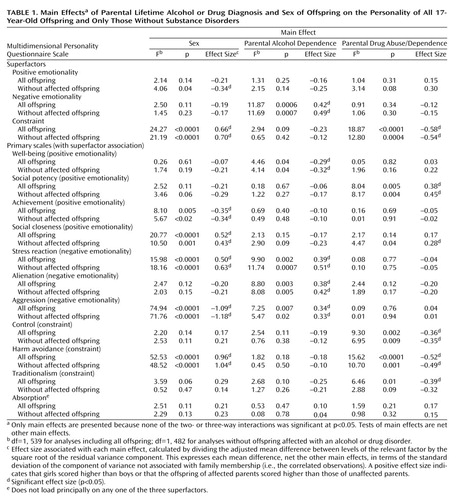
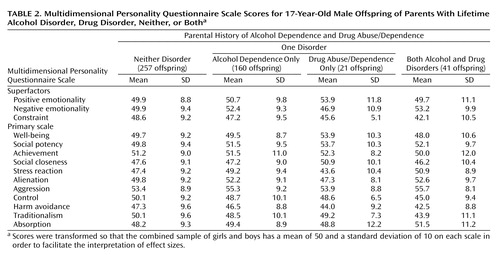
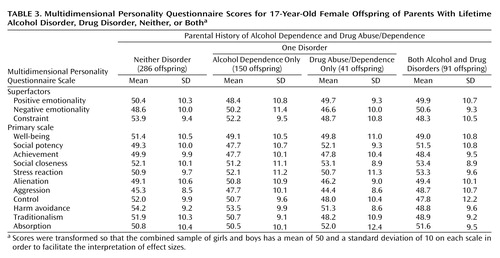
The results of the hierarchical linear model analyses, both with and without offspring affected by a substance use disorder themselves, are given in Table 1. None of the interactions was significant at p<0.05, so only main effects are discussed. For the main effect of offspring sex, adolescent girls scored significantly higher on constraint, social closeness, stress reaction, and harm avoidance than boys and significantly lower on aggression and achievement. The direction of these sex effects can be observed by the sign (positive or negative) of the effect sizes in Table 1 and through comparison of Table 2 and Table 3, which give the means and standard deviations on each Multidimensional Personality Questionnaire scale for male and female offspring, respectively, according to parental diagnosis. Although all analyses were conducted by using raw Multidimensional Personality Questionnaire scores, to facilitate interpretation of the magnitude of effects, raw scores were transformed into T scores in the tables so that the combined male and female sample had a mean of 50 (SD=10) on each scale.
The main effects (Table 1) associated with parental alcohol history control for the effect of drug history and the main effects of parental drug history control for the effect of alcohol history to show which effects are specific to each disorder. Thus, adolescents whose parents had alcohol dependence scored significantly higher on negative emotionality and on all of its primary scales of stress reaction, alienation, and aggression, as well as lower on well-being than those without a parental alcohol history. Adolescents whose parents had a drug disorder scored significantly lower on constraint and on all of its primary scales of control, harm avoidance, and traditionalism, as well as significantly higher on social potency, compared to the offspring of parents without a drug history. When analyses were repeated only for offspring free of a substance use disorder, only the parental drug effect on traditionalism was no longer significant (p increased from 0.01 to 0.09). In fact, some significant effects occurred only in offspring without substance use disorders (e.g., see parental drug effect on social closeness in Table 1). The findings were robust for both male and female offspring, but the importance of controlling for gender is shown by the fact that the mean score for constraint (48.6) for low-risk boys (neither disorder group in Table 2) is about the same as the mean (48.7) in a high-risk group of girls (drug abuse/dependent only group in Table 3).
However, the absence of significant interactions with sex suggests that the relationship of parental history of substance use disorders to offspring personality is not significantly different for male and female adolescents. Therefore, in Figure 1, means for the three superfactors were adjusted for gender and expressed as an effect size (relative to the low-risk group) for the offspring of parents with a history of an alcohol disorder, a drug disorder, or both disorders. The overall magnitude of parental drug diagnosis on constraint is slightly larger than the parental alcohol effect on negative emotionality. However, comparison of the left panel of Figure 1 (including all high-risk offspring) to the right panel (including only high-risk offspring without substance use disorders themselves) illustrates that excluding offspring with a substance use disorder had little impact. One small change was that scores for the offspring of parents with both disorders went from an effect size of 0.6 SD to an effect size of 0.4 SD below the mean for the low-risk offspring on constraint. This suggests that the offspring that are lowest in constraint are most likely to develop an early-onset substance use disorder by age 17 (in fact, nearly 25% of the adolescents whose parents had both disorders had developed an alcohol disorder, and nearly 20% had an illicit drug disorder).
Discussion
This study represents a rare attempt to incorporate parental diagnoses of both alcohol and drug disorders based on direct interviews of both mothers and fathers to investigate how a parental history of substance use disorders is associated with offspring personality. We found the following for both male and female adolescents:
| 1. | Those whose parents had an alcohol disorder scored higher on negative emotionality and all of its primary scales (aggression, alienation, and stress reaction) and had lower well-being than those without a parental alcohol history. | ||||
| 2. | Those whose parents had a drug disorder scored significantly lower on constraint and all of its associated primary scales (control, harm avoidance, and traditionalism) and higher on social potency than those without a parental drug history. | ||||
| 3. | A comparison of the results obtained when including or excluding adolescents with substance use disorders revealed that the relationships noted between parental history and offspring personality, although specific to the type of disorder, did not change appreciably when offspring with early-onset substance use disorders were removed from the analysis. Both negative emotionality and constraint remain elevated in high-risk adolescents who were free of a substance use disorder at age 17, strongly supporting the assertion that these traits represent familial risk factors. | ||||
Therefore, although the personality dimensions associated with substance use disorders in our sample were quite consistent with those reported by Swendsen et al. (15), although they did not compare alcohol and drug disorders, our findings, after we excluded affected relatives, were quite different. This could be because we were studying adolescents, whereas the sample investigated by Swendsen et al. consisted of adults. Because our subjects were only 17, some classified as unaffected will ultimately be affected by a substance use disorder. Genetic factors constitute the most important influence on adolescent personality factors related to substance use disorders (32). Thus, as our participants pass more fully through the age of risk, we expect that offspring inheriting the most deviant personality profiles would be most likely to develop a substance use disorder and thus be excluded from the analysis. This would lead to the possible impression that the effect of parental substance use disorders on offspring personality is diminishing with age when that is not the case. Rather, because some (but not all) offspring of parents with substance use disorders would be expected to inherit a risky personality, personality may increasingly overlap with substance use disorder phenotypes, and our results may be more similar to those of Swendsen et al. as twins in our group age.
Another possible reason for these discrepant results is how comorbidity is handled. In the study by Swendsen et al. (15), the presence of other disorders (e.g., antisocial personality) was carefully assessed and statistically controlled to prevent possible confounds in assessing the unique relationship of substance use disorders to personality. Other investigators consider comorbidity a naturally occurring phenomenon that should be explored directly. In other Minnesota Twin Family Study research, it was concluded that the comorbidity of substance use disorders, antisocial behavior, and low constraint could be accounted for by a single underlying highly heritable latent externalizing trait (33). Similar results have been obtained in other twin samples (11). Such a trait, along with related psychophysiological characteristics, has the potential to improve the phenotypic definition for molecular genetic studies of substance use disorders (20).
Finally, consistent with our findings that higher offspring negative emotionality is associated with parental alcohol (but not drug) diagnosis, twin studies suggest that the genetic overlap of internalizing disorders with substance use disorders is greater for alcoholism (34) than for illicit substance use disorders (35). While researchers (11, 36) have suggested that some forms of negative emotionality (e.g., hostility) may be more predictive of drinking than others, it should be noted that all aspects of negative emotionality assessed in the present study were deviant in the offspring of alcoholic parents.
In the future, we will assess whether new cases of substance use disorders arising between age 17 and follow-ups at age 20 and 24 are prospectively predicted by personality factors. Future understanding of the development of substance use disorders would also do well to include nicotine dependence among the outcomes studied. Personality, in tandem with other factors, may have use in refining identification of high-risk individuals and in initiating effective prevention or treatment efforts.
 |
 |
 |
Received March 10, 2003; revision received Aug. 26, 2003; accepted Aug. 28, 2003. From the Twin Cities Campus, University of Minnesota. Address reprint requests to Dr. Elkins, Department of Psychology, University of Minnesota, 75 E. River Rd., Minneapolis, MN 55455; [email protected] (e-mail). Supported by grants from the National Institute on Alcohol Abuse and Alcoholism (AA-09367) and the National Institute on Drug Abuse (DA-05147).
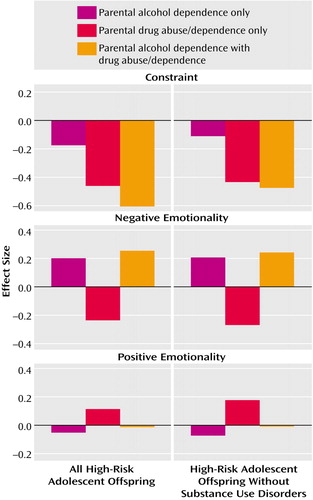
Figure 1. Personality Profiles of 17-Year-Old Offspring of Parents With Lifetime Alcohol Disorder, Drug Disorder, or Botha
aThe bars give gender-adjusted means for each of these high-risk groups, expressed as an effect size relative to the low risk group (offspring of parents with neither type of disorder) whose mean was set at 0. The figure illustrates effect sizes for offspring groups resulting from different combinations of parental substance use disorders; thus, the effect sizes may differ slightly from those calculated for each main effect in Table 1. The number of offspring in each group is as follows: for all high-risk adolescent offspring—parental alcohol dependence only, N=310; parental drug abuse/dependence only, N=62; both, N=132; for high-risk adolescent offspring without substance use disorders—parental alcohol dependence only, N=242; parental drug abuse/dependence only, N=51; both, N=94.
1. Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig M, Fenton B, Zhang H, O’Malley S, Rounsaville BJ: Familial transmission of substance use disorders. Arch Gen Psychiatry 1998; 55:973–979Crossref, Medline, Google Scholar
2. Heath AC, Bucholz KK, Madden PA, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB, Martin NG: Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychol Med 1997; 27:1381–1396Crossref, Medline, Google Scholar
3. Kendler KS, Prescott CA, Neale MC, Pedersen NL: Temperance board registration for alcohol abuse in a national sample of Swedish male twins, born 1902 to 1949. Arch Gen Psychiatry 1997; 54:178–184Crossref, Medline, Google Scholar
4. McGue M, Elkins I, Iacono WG: Genetic and environmental influences on adolescent substance use and abuse. Am J Med Genet 2000; 96:671–677Crossref, Medline, Google Scholar
5. Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Lin N, Meyer JM, Toomey R, Faraone SV, Eaves L: Genetic influences on DSM-III-R drug abuse and dependence: a study of 3,372 twin pairs. Am J Med Genet 1996; 67:473–477Crossref, Medline, Google Scholar
6. Goodwin DW, Schulsinger F, Moller N, Hermansen L, Winokur G, Guze SB: Drinking problems in adopted and nonadopted sons of alcoholics. Arch Gen Psychiatry 1974; 31:164–169Crossref, Medline, Google Scholar
7. Newlin DB, Miles DR, van den Bree MB, Gupman AE, Pickens RW: Environmental transmission of DSM-IV substance use disorders in adoptive and stepfamilies. Alcohol Clin Exp Res 2000; 24:1785–1794Crossref, Medline, Google Scholar
8. Tarter RE, Vanyukov M: Alcoholism: a developmental disorder. J Consult Clin Psychol 1994; 62:1096–1107Crossref, Medline, Google Scholar
9. McGue M: Genetics of personality, in Principles and Practice of Medical Genetics, 4th ed, vol 3. Edited by Rimoin DL, Connor JM, Pyeritz RE, Korf BR. London, Churchill Livingstone, 2001, pp 2791–2800Google Scholar
10. Sher KJ, Trull TJ, Bartholow BD, Vieth A: Personality and alcoholism: issues, methods, and etiological processes, in Psychological Theories of Drinking and Alcoholism, 2nd ed. Edited by Leonard KE, Blane HT. New York, Guilford, 1999, pp 54–105Google Scholar
11. Slutske WS, Heath AC, Madden PAF, Bucholz KK, Statham DJ, Martin NG: Personality and the genetic risk for alcohol dependence. J Abnorm Psychol 2002; 111:124–133Crossref, Medline, Google Scholar
12. Masse LC, Tremblay RE: Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatry 1997; 54:62–68Crossref, Medline, Google Scholar
13. Cloninger CR, Sigvardsson S, Bohman M: Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res 1988; 12:494–505Crossref, Medline, Google Scholar
14. Sher KJ, Bartholow BD, Wood MD: Personality and substance use disorders: a prospective study. J Consult Clin Psychol 2000; 68:818–829Crossref, Medline, Google Scholar
15. Swendsen JD, Conway KP, Rounsaville BJ, Merikangas KR: Are personality traits familial risk factors for substance use disorders? results of a controlled family study. Am J Psychiatry 2002; 159:1760–1766Link, Google Scholar
16. Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC: Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry 1997; 54:313–321Crossref, Medline, Google Scholar
17. McGue M, Slutske WS, Iacono WG: Personality and substance use disorders, II: alcoholism versus drug use disorders. J Consult Clin Psychol 1999; 67:394–404Crossref, Medline, Google Scholar
18. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
19. Costa PT Jr, McCrae RR: Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1992Google Scholar
20. Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M: Behavioral disinhibition and the development of substance use disorders: findings from the Minnesota Twin Family Study. Dev Psychopathol 1999; 11:869–900Crossref, Medline, Google Scholar
21. Johnson W, Krueger RF, Bouchard TJ, McGue M: The personalities of twins: just ordinary folks. Twin Res 2002; 5:125–131Crossref, Medline, Google Scholar
22. Kendler KS, Martin NG, Heath AC, Eaves LJ: Self-report psychiatric symptoms in twins and their non-twin relatives: are twins different? Am J Med Genet 1995; 60:588–591Crossref, Medline, Google Scholar
23. Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, Sartorius N, Towle LH: The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988; 45:1069–1077Crossref, Medline, Google Scholar
24. Mannuzza S, Fyer AJ, Endicott J, Klein DF: Family Informant Schedule and Criteria (FISC). New York, New York State Psychiatric Institute, Anxiety Disorders Clinic, 1985Google Scholar
25. Reich W: Diagnostic Interview for Children and Adolescents (DICA). J Am Acad Child Adolesc Psychiatry 2000; 39:59–66Crossref, Medline, Google Scholar
26. Tellegen A, Waller NG: Exploring Personality Through Test Construction: Development of the Multidimensional Personality Questionnaire. Minneapolis, University of Minnesota Press, 2001Google Scholar
27. Andreasen NC, Rice J, Endicott J, Reich T, Coryell W: The family history approach to diagnosis: how useful is it? Arch Gen Psychiatry 1986; 43:421–429Crossref, Medline, Google Scholar
28. DeLucia C, Belz A, Chassin L: Do adolescent symptomatology and family environment vary over time with fluctuations in paternal alcohol impairment? Dev Psychol 2001; 37:207–216Crossref, Medline, Google Scholar
29. Bryk AS, Raudenbush SW: Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park, Calif, Sage Publications, 1992Google Scholar
30. Littell RC, Milliken GA, Stroup WW, Wolfinger RD: SAS System for Mixed Models. Cary, NC, SAS Institute, 1996Google Scholar
31. Pollock NK, Martin CS: Diagnostic orphans: adolescents with alcohol symptoms who do not qualify for DSM-IV abuse or dependence diagnoses. Am J Psychiatry 1999; 156:897–901Link, Google Scholar
32. Mustanski BS, Viken RJ, Kaprio J, Rose RJ: Genetic influences on the association between personality risk factors and alcohol use and abuse. J Abnorm Psychol 2003; 112:282–289Crossref, Medline, Google Scholar
33. Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M: Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol 2002; 111:411–424Crossref, Medline, Google Scholar
34. Prescott CA, Aggen SH, Kendler KS: Sex-specific genetic influences on the comorbidity of alcoholism and major depression in a population-based sample of US twins. Arch Gen Psychiatry 2000; 57:803–811Crossref, Medline, Google Scholar
35. Tsuang MT, Bar JL, Harley RM, Lyons MJ: The Harvard Twin Study of Substance Abuse: what we have learned. Harv Rev Psychiatry 2001; 9:267–279Crossref, Medline, Google Scholar
36. Hussong AM, Hicks RE, Levy SA, Curran PJ: Specifying the relations between affect and heavy alcohol use among young adults. J Abnorm Psychol 2001; 110:449–461Crossref, Medline, Google Scholar



