Family Disruption in Childhood and Risk of Adult Depression
Abstract
OBJECTIVE: The authors examined the risk that family disruption and low socioeconomic status in early childhood confer on the onset of major depression in adulthood. METHOD: Participants were 1,104 offspring of mothers enrolled during pregnancy in the Providence, R.I., site of the National Collaborative Perinatal Project. Measures of childhood family disruption and socioeconomic status were obtained before birth and at age 7. Structured diagnostic interviews were used to assess respondents’ lifetime history of major depressive episode between the ages of 18 and 39. Survival analysis was used to identify childhood risks for depression onset. RESULTS: Parental divorce in early childhood was associated with a higher lifetime risk of depression among subjects whose mothers did not remarry as well as among subjects whose mothers remarried. These effects were more pronounced when accompanied by high levels of parental conflict. Independent of the respondents’ adult socioeconomic status, low socioeconomic status in childhood predicted an elevated risk of depression. CONCLUSIONS: Family disruption and low socioeconomic status in early childhood increase the long-term risk for major depression. Reducing childhood disadvantages may be one avenue for prevention of depression. Identification of modifiable pathways linking aspects of the early childhood environment to adult mental health is needed to mitigate the long-term consequences of childhood disadvantage.
An unresolved question concerning the development of adult depression is whether early childhood adversity confers risk that persists beyond childhood. It is known that family disruption and low socioeconomic status among children are related to behavioral and psychological disturbances as well as delays in cognitive development (1, 2). In the United States, the proportion of children under age 18 in households headed by a single female increased from 9.0% in 1959 to 22.4% in 1999; the prevalence of child poverty in female-headed households increased from 24.1% to 57.4% over the same time period (3). Moreover, epidemiologic evidence suggests that rates of depression have increased in recent generations (4). There is concern that these trends in the structure and socioeconomic circumstances of families contribute to increasing rates of depression.
In cross-sectional studies of adults (5, 6), reports of family disruption and low socioeconomic status are more common among depressed individuals than nondepressed individuals. Prospective data from several cohort studies have also demonstrated a link between childhood adversity and depressive symptoms in adulthood (7–9).
Previous investigations of the long-term psychiatric consequences of the childhood environment are limited in several respects. First, research in this area has often been conducted by analyzing cross-sectional samples of selected populations and has often relied on retrospective reports of the childhood environment. Although results from longitudinal population-based studies are emerging, most have used scales of psychological distress and depressive symptoms rather than psychiatric diagnoses based on modern diagnostic criteria. These scales often lack comparability across studies and do not correspond to DSM criteria for a depressive disorder. Second, although there is a close relation between socioeconomic status and family disruption in childhood (10), few studies have demonstrated their independent effects on adult mental health. Third, the long-term effects of divorce and other forms of family disruption on the development of depression are in doubt because of the unanswered question of whether it is the disruption or the often attendant parental conflict that poses the salient risk for subsequent depression (see, for example, Ni Bhrolchain et al. [11]).
In this study, we examined the prospective associations between family disruption and low socioeconomic status during the first 7 years of life and the adult onset of major depression. We also analyzed retrospective reports of parental conflict to investigate the impact of family disruption with and without conflict on subsequent depression.
Method
Study Sample and Adult Follow-Up Procedures
Subjects were offspring of participants in the Providence, R.I., site of the National Collaborative Perinatal Project (12), a multisite study that enrolled more than 50,000 pregnancies nationally and followed the offspring prospectively through the first 7 years of life. Obstetrical intake occurred between 1959 and 1966. In Providence, a total of 4,140 pregnancies were enrolled.
From the 4,140 Providence National Collaborative Perinatal Project births, 1,780 individuals were selected for participation in the adult follow-up study. Selection occurred in two separate phases; in each, a stratified random sample was drawn from the entire cohort to investigate the association between several early life factors and adult psychiatric disorders. During phase one, initiated in 1984, 995 eligible subjects 18–27 years old with and without maternal pregnancy/delivery complications were selected (13). In the second phase, initiated in 1996, 1,056 subjects 30–39 years old with and without learning disabilities were selected (14). There was a small overlap (N=271) between the first- and second-phase samples. For participants included in both phases, phase-two interviews were used unless depression had been reported at the initial (phase-one) assessment, in which case the earlier information was used. Written informed consent was obtained from all subjects.
Measures
Family disruption during childhood was defined according to the number of parents living in the household at the time of enrollment and at age 7 and according to any changes in the parents’ marital status during the first 7 years of life. This scheme resulted in the following six-category measure of early childhood family disruption: 1) one parent in the household at birth and age 7, no changes in parents’ marital status; 2) two parents at birth, mother widowed at age 7; 3) two parents at birth, mother separated at age 7; 4) two parents at birth, mother divorced at age 7; 5) two parents at birth and age 7, mother divorced and remarried; and 6) two parents at birth and age 7, no changes in parents’ marital status.
In preliminary analyses, we examined the relation between several indicators of childhood socioeconomic status (parental occupation, education, and household income) and adult depression. Because parental occupation was the indicator of childhood socioeconomic status most strongly associated with the onset of depression, childhood socioeconomic status based on parental occupation was used in the present analyses. Occupation was defined as either manual or nonmanual according to 1960 U.S. Census categories (15). Subjects in two-parent households were assigned to the occupational category of the parent in the higher category, and subjects in one-parent households were assigned to the occupational category of the parent with whom they were living, even if the other parent was in a higher category. Subjects with parents outside of the paid labor force at the time of either childhood assessment were categorized as not employed. Accordingly, parental occupation at the respondent’s birth and seventh year was coded in the following five categories: 1) manual at birth and age 7; 2) not employed at either occasion; 3) manual at birth, nonmanual at age 7; 4) nonmanual at birth, manual at age 7; and 5) nonmanual at birth and age 7.
History of parental conflict was determined by responses to four questions asked during the adult follow-up assessment: 1) Did your parents argue or fight in front of you? 2) Did either/any of your parents ever hit the other? 3) Did they hit the other often? 4) Did you ever see it happen? Participants endorsing at least three of the four parental conflict questions were coded as having a high level of parental conflict. Although this measure is imprecise and based on retrospective reports, the inclusion of information on parental conflict in the investigation of long-term effects of family disruption is essential for understanding the potential pathogenic mechanisms involved.
Lifetime diagnosis of major depressive episode was determined by using the National Institute of Mental Health Diagnostic Interview Schedule (DIS) (16), administered to subjects in adulthood by trained interviewers. The DIS has been used widely in community samples with demonstrated reliability and validity for the diagnosis of depression (17, 18). During the first phase of the follow-up study, diagnoses were based on DSM-III criteria, and in the second phase, begun in 1996, the DSM-IV version of the DIS was used. The analyses presented here combine DSM-III and DSM-IV diagnoses of major depressive episode, which are similar although not identical. Changes in diagnostic criteria for depression appeared to have little impact on the identification of cases in community surveys (19). This was also true in the present sample; we observed a high level of concordance between DSM-III and DSM-IV diagnoses of depression in the subset of respondents for whom we were able to assign both diagnoses (9).
Statistical Analysis
Discrete-time survival analysis, a Cox regression model for the analysis of events that are recorded in discrete time intervals, was used to model the retrospectively reported age at onset of depression (20). This model yields estimates of risk for the initial onset of depression that account for the number of years during which respondents were at risk for a first depressive episode. The analyses described here, therefore, were based on the person-years from birth through age at onset of depression for those respondents with a lifetime history of depression, and on the person-years from birth through age at interview for those respondents without a lifetime history of depression. The following control variables were included in the survival models: family history of mental disorders before the birth of the child, maternal age at the time of the respondent’s birth, and the respondent’s age at interview, sex, and race/ethnicity. Family history of mental disorders before the birth of the child was included as a control because of the known higher risk for depression among offspring of depressed parents (21). Family history was determined by the mother’s report on enrollment of whether she or the subject’s father had ever received treatment for emotional or behavioral problems. Finally, we included a set of indicator variables representing the factors used to select participants for the Providence National Collaborative Perinatal Project follow-up study (i.e., pregnancy or delivery complications and potential learning disabilities at age 7).
Results
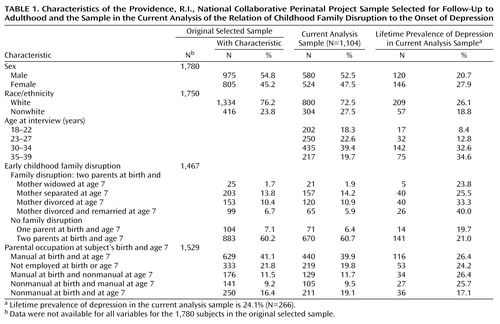
Characteristics of the Sample
The demographic characteristics of the 1,780 subjects originally selected for follow-up are shown in Table 1; 1,267 of these subjects were successfully located and interviewed, and complete data were available for 1,104 of the subjects. These 1,104 subjects make up the sample for the current analysis. The demographic characteristics of the current analysis sample, also shown in Table 1, were virtually identical to those of the original selected sample. Slightly more than half of the subjects in the current analysis were male, the majority were white, and the mean age was 29.1 (SD=5.7). More than half of respondents lived in two-parent families between birth and age 7. The subjects came from predominantly working class backgrounds; the parental occupations of 39.9% of the respondents was manual at their birth and seventh year. The current analysis sample was approximately balanced with regard to the study selection factors. Of the 1,104 respondents included in the current analysis sample, 242 (21.9%) were chosen for a history of pregnancy or delivery complications and 339 (30.7%) were chosen for the presence of potential learning disabilities at age 7; the numbers of respondents selected for the absence of these factors were 212 (19.2%) and 311 (28.2%), respectively.
The lifetime prevalence of major depression in the sample was 24.1% (N=266); this is somewhat higher than in nationally representative surveys (e.g., 17.1% in the National Comorbidity Survey [22]). Table 1 shows the lifetime prevalence of depression within each category of the sociodemographic variables. On preliminary inspection, we observed substantial variability in the lifetime risk of depression across categories of early childhood family disruption (χ2=23.7, df=5, p=0.0003), attributable mainly to higher lifetime risks among respondents who experienced parental divorce in early childhood (regardless of subsequent remarriage) than among respondents whose parents’ marital status remained unchanged between birth and age 7. Lifetime risk of depression also varied according to parental occupation, with the highest socioeconomic status category (employed in nonmanual occupations at both times) predicting a lower risk of depression (χ2=9.6, df=4, p=0.05).
Respondents whose parents were unemployed or had manual occupations were considerably more likely to reside in one-parent families than were respondents whose parents had nonmanual occupations. For example, 41 (12.2%) of respondents born to parents with nonmanual occupations lived in one-parent families, compared with 24 (30.4%) and 171 (25.9%) of respondents born to parents who were not employed or had manual occupations, respectively (χ2=28.2, df=2, p<0.001). The strong association between family disruption and socioeconomic status emphasizes the need to analyze both factors simultaneously as risks for the development of depression.
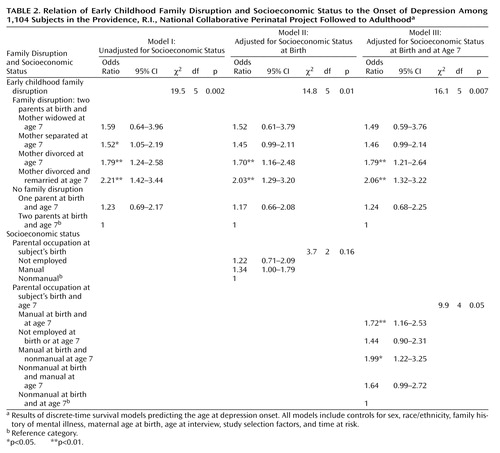
Family Disruption and Socioeconomic Status in Childhood and the Onset of Depression
The results of survival analyses of depression onset are shown in Table 2. Model I contains five indicator variables for family disruption, model II adds parental occupation at birth, and model III replaces parental occupation at birth with a combined measure of parental occupation at birth and age 7. In all three models, family disruption was significantly associated with the onset of major depression. Parental divorce between birth and age 7, regardless of subsequent remarriage, was predictive of a twofold higher depression risk. These results suggest an association between family disruption, particularly divorce, and subsequent depression that is independent of socioeconomic status, i.e., not attributable to the higher proportion of one-parent families among subjects with lower socioeconomic status.
Independent of family disruption, the risk for depression among participants belonging to the four lower childhood socioeconomic status categories was generally higher than the risk among those from the highest socioeconomic status background, with adjusted odds ratios ranging from 1.44 to 1.99. These results are consistent with the lifetime risks of depression shown in Table 1, which were 17% among respondents from the highest socioeconomic status background and approximately 25% among respondents from lower socioeconomic status backgrounds.
Two additional analyses were done at this point. First, to investigate whether family disruption more strongly predicted depression among children of lower socioeconomic status, we examined the consistency of the odds ratios for family disruption across categories of childhood socioeconomic status. The risk for depression associated with parental divorce was found to be of a similar magnitude across categories of childhood socioeconomic status. A second analysis considered whether the relation between childhood socioeconomic status and adult depression was independent of respondents’ own attained socioeconomic status. To address this question, we added respondents’ educational attainment to model III. However, the significant associations between childhood family disruption and low socioeconomic status and the development of depression persisted, and were of a similar magnitude, after we controlled for respondents’ education.
Parental Conflict
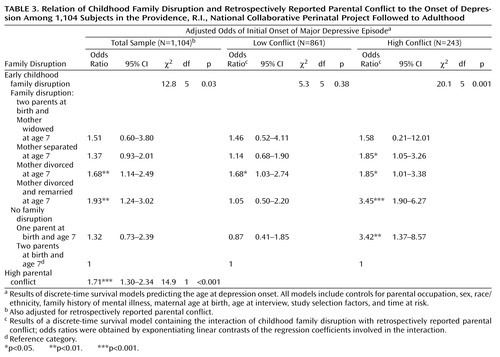
Finally, we examined the influence of parental conflict on the relation between childhood family disruption and the lifetime risk of depression. Twenty-two percent of the sample endorsed at least three of four questions reflecting parental conflict (internal consistency of the four items [alpha]=0.83).
Adding parental conflict to the survival model did not substantially change the association between family disruption and depression (Table 3). Parental conflict was independently related to a higher lifetime risk of depression (Table 3). The results of a second survival analysis of the interaction between childhood family disruption and low and high parental conflict are shown in Table 3 (χ2=11.0, df=5, p=0.05, for the interaction). Although interpretation of this interaction is tempered by the reduced sample sizes for this analysis, parental conflict appears to exacerbate the long-term effect of childhood family disruption on the development of depression. Thus, family disruption in childhood was associated with depression among individuals reporting low parental conflict, but its effect was much stronger among those reporting high levels of parental conflict.
The interaction between parental conflict and childhood family disruption is shown graphically in Figure 1: within each category of childhood family disruption, the adjusted lifetime prevalence of depression is plotted separately for the subjects reporting low and high levels of parental conflict. With the exception of children in stable two-parent families, and the small number of children whose mothers were widowed, rates of lifetime depression were elevated among subjects reporting high levels of parental conflict, irrespective of family type (the difference for divorced families was marginally significant). For example, among adults whose mother divorced and remarried by age 7, the adjusted lifetime risk of depression in subjects reporting high levels of parental conflict was 57.0%, compared with 20.5% in subjects reporting low levels of parental conflict.
Discussion
In this study, we examined the lifetime risk of major depressive episode associated with family disruption and low socioeconomic status in early childhood. Parental divorce by age 7 predicted a greater risk of adult depression. On average, respondents who experienced parental divorce were at twice the risk of depression than those whose parents’ marriages remained intact during their childhood; however, the risk associated with parental divorce was most pronounced when accompanied by a high level of parental conflict. The small number of respondents who experienced the death of a parent in childhood precluded a thorough analysis of long-term depression risk due to loss of a parent. Independent of family disruption, risk of depression was also elevated among children from low socioeconomic status backgrounds.
Limitations
The Providence, R.I., National Collaborative Perinatal Project sample was not designed to be representative of the general U.S. population or of Providence, R.I. However, our finding that low socioeconomic status and family disruption in childhood confer elevated risk for adult depression is consistent with the findings of previous investigations (7, 8) and suggests that our results are not specific to the present sample. Our sample was selected for the presence or absence of early childhood risk factors for adult psychopathology, including pregnancy/delivery complications and potential learning disabilities (13, 14). Although the distribution of these potential risk factors in the present sample may differ from the general population, the sampling scheme was accounted for by including controls for the study selection factors in all of the analyses.
Because our analyses of family disruption and socioeconomic status were limited to the period of early childhood, we were not able to examine the impact of childhood conditions beyond age 7 on the risk of depression. However, the early childhood period may be of special importance. In a report based on 935 participants in the Christchurch Health and Development Study, Fergusson et al. (23) found that parental separation predicted the onset of mood disorders only when it occurred by age 5.
Finally, our analyses of parental conflict have the usual drawbacks of retrospective recall, including the possibility of systematic differences in the reporting of parental conflict according to depression status. Our use of a dichotomous indicator of parental conflict also precluded a more detailed analysis of different kinds of parental conflict and the timing of such conflict with respect to changes in family structure. The measure of parental conflict used in this study likely reflects more severe forms of interpersonal conflict (i.e., physical aggression), although this has not been assessed in validation studies.
Comments
The systematic pattern of association between family disruption and socioeconomic status reflects the underlying reciprocal relations between family composition and economic disadvantage (10): economic hardship predicts marital strain and dissolution (24), and single-parent families are at greater risk of experiencing financial difficulties (25). In the present study, both of these factors contributed independently to an individual’s lifetime risk of depression. Thus, although the socioeconomic circumstances of children frequently decline after changes in parental marital status, such declines do not appear to be the sole reason that family disruption is predictive of depression. In view of the finding that family disruption and socioeconomic status in childhood predicted lifetime depression independent of the adult socioeconomic status of respondents, we conclude that the long-term mental health consequences of childhood conditions are not entirely mitigated by social mobility in adulthood.
Our analyses concern the long-term consequences of childhood disadvantage that occurred during the 1960s. It may be that along with the increasing rates of divorce during the past 40 years, intervening changes in policies and social norms have reduced the impact of family disruption among children today. Unfortunately, this does not seem to be the case. Socioeconomic disadvantage and family disruption continue to be adversely related to cognitive development and mental health among children in current samples (1, 26, 27).
Our data indicate that the association between childhood family disruption and adult depression can be intensified by family conflict. Since we were unable to determine whether such conflict occurred before divorce or was a result of stresses brought on by the divorce itself, multiple interpretations are possible. One is that predivorce conflict is responsible for long-term depression risk. Block et al. (28) prospectively observed personality differences between children whose parents subsequently divorced and those whose parents’ marriages remained intact; these differences presumably reflect exposure to predivorce familial conflict. Alternatively, the consequences of divorce may be of primary relevance for the development of depression. In a study of adolescents, Aseltine (27) found that the longitudinal association between parental divorce and depressive symptoms was attributable to postdivorce stresses rather than to circumstances preceding the divorce. Distinguishing between pre- and postdivorce conflict in future studies is essential for the comparative assessment of these two theories; it will also enable researchers to determine whether parental divorce in some cases may protect the mental health of children if it brings about the cessation of family conflict (29).
Our study did not permit an elaboration of the pathways linking childhood conditions to the onset of adult depressive disorders. According to existing evidence, the pathways involved will likely comprise factors in the proximal childhood period—including conduct and other psychiatric disorders (23)—as well as stressors in adult life that are farther removed in time from childhood disadvantage (30). In addition to identifying psychosocial pathways, a question of central interest concerns the biological translation of psychosocial stressors. Impaired neurodevelopment may be one route of translation, in view of evidence that environmental stressors in utero (31) as well as developmental delays in childhood (32) predict adult depression. Stress hormone responsiveness appears to be another promising area for further investigation (33). Chronic adversity has been linked to disturbances in the hypothalamic-pituitary-adrenal (HPA) axis in children with depression (34); HPA abnormalities in major depression may also become more pronounced in adulthood (35).
Further research to identify pathways of risk for major depression will facilitate the development of tailored clinical interventions and policies aimed at mitigating the long-term consequences of childhood disadvantage. At present, results of this study suggest that children from environments characterized by low socioeconomic status and parental divorce are at heightened risk for depression and may therefore benefit from interventions already shown to be effective in reducing risk for depression in other populations deemed at risk (36, 37).
 |
 |
 |
Portions of this work were presented at the 154th Annual Meeting of the American Psychiatric Association, New Orleans, May 5–10, 2001, and the Society for Epidemiologic Research/North American Congress of Epidemiology, Toronto, June 13–16, 2001. Received Jan. 9, 2002; revisions received April 25 and Oct. 2, 2002; accepted Oct. 14, 2002. From the Departments of Maternal and Child Health, Health and Social Behavior, Biostatistics, and Epidemiology, Harvard School of Public Health; and the Centers for Behavioral and Preventive Medicine, Brown Medical School and The Miriam Hospital, Providence, R.I. Address reprint requests to Dr. Gilman, Department of Maternal and Child Health, Harvard School of Public Health, 677 Huntington Ave., Boston, MA 02115; [email protected] (e-mail). Supported in part by NIMH grants MH-61953 (Drs. Buka and Gilman) and MH-17119 (Dr. Fitzmaurice), grant GM-29745 from the National Institute of General Medical Sciences (Dr. Fitzmaurice), and a grant from the MacArthur Foundation Network on Socioeconomic Status and Health (Drs. Kawachi and Gilman).The authors thank Dr. Richard Rende and Dr. Brian Hitsman for their helpful comments.
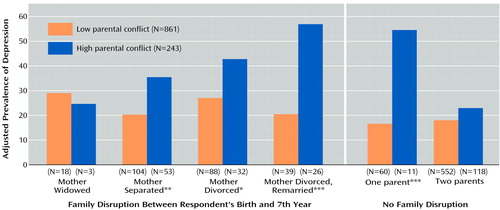
Figure 1. Adjusted Lifetime Prevalence of Major Depression Among 1,104 Subjects in the Providence, R.I., National Collaborative Perinatal Project Followed to Adulthood According to Childhood Family Disruption and Retrospectively Reported Parental Conflicta
aThe prevalence rates were adjusted for sex, race/ethnicity, family history of mental illness, maternal age at birth, age at interview, and study selection factors by using linear regression. The p values indicate the significance of the differences in the adjusted lifetime prevalence of depression between respondents reporting high versus low parental conflict in each category of childhood family disruption.
*p<0.06. **p<0.05. ***p<0.01.
1. McLeod JD, Shanahan MJ: Trajectories of poverty and children’s mental health. J Health Soc Behav 1996; 37:207-220Crossref, Medline, Google Scholar
2. Fergusson DM, Lynskey MT, Horwood LJ: The effects of parental separation, the timing of separation and gender on children’s performance on cognitive tests. J Child Psychol Psychiatry 1994; 35:1077-1092Crossref, Medline, Google Scholar
3. US Bureau of the Census: Historical Poverty Table 10: Related Children in Female Householder Families as a Proportion of All Related Children, by Poverty Status: 1959 to 2001. http://landview.census.gov/hhes/poverty/histpov/hstpov10.htmlGoogle Scholar
4. Lavori PW, Warshaw M, Klerman G, Mueller TI, Leon A, Rice J, Akiskal H: Secular trends in lifetime onset of MDD stratified by selected sociodemographic risk factors. J Psychiatr Res 1993; 27:95-109Crossref, Medline, Google Scholar
5. Kessler RC, Davis CG, Kendler KS: Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 1997; 27:1101-1119Crossref, Medline, Google Scholar
6. Harris T, Brown GW, Bifulco A: Loss of parent in childhood and adult psychiatric disorder: the role of social class position and premarital pregnancy. Psychol Med 1987; 17:163-183Crossref, Medline, Google Scholar
7. Power C, Hertzman C, Matthews S, Manor O: Social differences in health: life-cycle effects between ages 23 and 33 in the 1958 British birth cohort. Am J Public Health 1997; 87:1499-1503Crossref, Medline, Google Scholar
8. Sadowski H, Ugarte B, Kolvin I, Kaplan C, Barnes J: Early life family disadvantages and major depression in adulthood. Br J Psychiatry 1999; 174:112-120Crossref, Medline, Google Scholar
9. Gilman SE, Kawachi I, Fitzmaurice G, Buka SL: Socioeconomic status in childhood and the lifetime risk of major depression. Int J Epidemiol 2002; 31:359-367Crossref, Medline, Google Scholar
10. Eggebeen DJ, Lichter DT: Race, family structure, and changing poverty among American children. Am Sociol Rev 1991; 56:801-817Crossref, Google Scholar
11. Ni Bhrolchain M, Chappell R, Diamond I, Jameson C: Parental divorce and outcomes for children: evidence and interpretation. Eur Sociol Rev 2000; 16:67-91Crossref, Google Scholar
12. Niswander KR, Gordon M: The Women and Their Pregnancies: The Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. Washington, DC, National Institutes of Health, 1972Google Scholar
13. Buka SL, Satz P, Seidman L, Lipsitt L: Defining learning disabilities: the role of longitudinal studies. Thalamus 1998; 16:14-29Google Scholar
14. Buka SL, Tsuang MT, Lipsitt LP: Pregnancy/delivery complications and psychiatric diagnosis: a prospective study. Arch Gen Psychiatry 1993; 50:151-156Crossref, Medline, Google Scholar
15. Methodology and Scores of Socioeconomic Status: Working Paper Number 15. Washington, DC, US Bureau of the Census, 1963Google Scholar
16. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381-389Crossref, Medline, Google Scholar
17. Erdman HP, Klein MH, Greist JH, Bass SM, Bires JK, Machtinger PE: A comparison of the Diagnostic Interview Schedule and clinical diagnosis. Am J Psychiatry 1987; 144:1477-1480Link, Google Scholar
18. Oliver JM, Simmons ME: Affective disorders and depression as measured by the Diagnostic Interview Schedule and the Beck Depression Inventory in an unselected adult population. J Clin Psychol 1985; 41:469-477Crossref, Medline, Google Scholar
19. Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Lyketsos C, Chen LS: Natural history of Diagnostic Interview Schedule/DSM-IV major depression: the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 1997; 54:993-999Crossref, Medline, Google Scholar
20. Cox DR: Regression models and life-tables. J R Stat Soc Ser B 1972; 34:187-220Google Scholar
21. Beardslee WR, Keller MB, Lavori PW, Staley J, Sacks N: The impact of parental affective disorder on depression in offspring: a longitudinal follow-up in a nonreferred sample. J Am Acad Child Adolesc Psychiatry 1993; 32:723-730Crossref, Medline, Google Scholar
22. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8-19Crossref, Medline, Google Scholar
23. Fergusson DM, Horwood LJ, Lynskey MT: Parental separation, adolescent psychopathology, and problem behaviors. J Am Acad Child Adolesc Psychiatry 1994; 33:1122-1131Crossref, Medline, Google Scholar
24. Voydanoff P: Economic distress and family relations: a review of the eighties. J Marriage Fam 1990; 52:1099-1115Crossref, Google Scholar
25. McQuillan K: Falling behind: the income of lone-mother families, 1970-1985. Can Rev Sociol Anthropol 1992; 29:511-523Crossref, Google Scholar
26. Amato PR: Children of divorce in the 1990s: an update of the Amato and Keith (1991) meta-analysis. J Fam Psychol 2001; 15:355-370Crossref, Medline, Google Scholar
27. Aseltine RH Jr: Pathways linking parental divorce with adolescent depression. J Health Soc Behav 1996; 37:133-148Crossref, Medline, Google Scholar
28. Block JH, Block J, Gjerde PF: The personality of children prior to divorce: a prospective study. Child Dev 1986; 57:827-840Crossref, Medline, Google Scholar
29. Amato PR: Children’s adjustment to divorce: theories, hypotheses, and empirical support. J Marriage Fam 1993; 55:23-28Crossref, Google Scholar
30. Landerman R, George LK, Blazer DG: Adult vulnerability for psychiatric disorders: interactive effects of negative childhood experiences and recent stress. J Nerv Ment Dis 1991; 179:656-663Crossref, Medline, Google Scholar
31. Brown AS, van Os J, Driessens C, Hoek HW, Susser ES: Further evidence of relation between prenatal famine and major affective disorder. Am J Psychiatry 2000; 157:190-195Link, Google Scholar
32. van Os J, Jones P, Lewis G, Wadsworth M, Murray R: Developmental precursors of affective illness in a general population birth cohort. Arch Gen Psychiatry 1997; 54:625-631Crossref, Medline, Google Scholar
33. Plotsky PM, Owens MJ, Nemeroff CB: Psychoneuroendocrinology of depression: hypothalamic-pituitary-adrenal axis. Psychiatr Clin North Am 1998; 21:293-307Crossref, Medline, Google Scholar
34. Kaufman J, Birmaher B, Perel J, Dahl RE, Moreci P, Nelson B, Wells W, Ryan ND: The corticotropin-releasing hormone challenge in depressed abused, depressed nonabused, and normal control children. Biol Psychiatry 1997; 42:669-679Crossref, Medline, Google Scholar
35. Birmaher B, Dahl RE, Perel J, Williamson DE, Nelson B, Stull S, Kaufman J, Waterman GS, Rao U, Nguyen N, Puig-Antich J, Ryan ND: Corticotropin-releasing hormone challenge in prepubertal major depression. Biol Psychiatry 1996; 39:267-277Crossref, Medline, Google Scholar
36. Beardslee WR, Gladstone TRG: Prevention of childhood depression: recent findings and future prospects. Biol Psychiatry 2001; 49:1101-1110Crossref, Medline, Google Scholar
37. Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR: Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995; 34:312-321Crossref, Medline, Google Scholar



