Use of Psychotropic Medications Among HIV-Infected Patients in the United States
Abstract
OBJECTIVE: This study describes the prevalence and pattern of use of psychotropic medications by HIV-positive patients receiving medical care in the United States and the search for possible predictors of use. METHOD: The HIV Cost and Services Utilization Study database was analyzed. From the estimated 231,400 HIV-positive patients in medical care in the contiguous United States, a probability sample of 2,864 adults who had paid at least one visit to their medical provider in early 1996 was selected. A representative group of 1,561 received the long form of the Composite International Diagnostic Interview and a questionnaire on psychotropic medications used during the previous 6 months; 1,489 patients (95.4%) completed the assessments. RESULTS: An estimated 27.2% of HIV-positive patients took psychotropic medications in 1996. Antidepressants were the most commonly prescribed drug class (20.9% of patients), followed by anxiolytics (16.7%), antipsychotics (4.7%), and psychostimulants (3.0%). Among patients with major depression or dysthymia, 43.2% reported receiving antidepressants, and 34.3% reported receiving anxiolytics. Psychiatric comorbidity was associated with greater use of psychotropics. Use of psychotropics in general, and antidepressants in particular, was significantly lower among African Americans than whites or Hispanics. Among patients with mood disorders, 61.0% of whites, 51.4% of African Americans, and 66.7% of Hispanics reported use of antidepressant medications or some type of psychosocial intervention. CONCLUSIONS: Psychotropics were commonly used by HIV-positive patients in medical care. About half of the patients suffering from depressive disorders did not receive antidepressants. Psychotropic drug use was lower among African Americans than other ethnic groups.
Psychotropic medications, such as antidepressants, anxiolytics, antipsychotics, and psychostimulants, are commonly and increasingly prescribed in both primary care and psychiatric practice settings (1). No national survey of the rate of use of the different types of psychotropics by HIV-positive patients has been previously reported, to our knowledge. It is estimated that about one-half of HIV-positive patients receiving medical care in the United States suffer from symptoms indicative of mood or anxiety disorders (2). The importance of identifying and treating depression cannot be overstated. The presence of mood disorders in HIV-positive patients is accompanied by impaired functioning and lower quality of life (3). Both psychotherapy and pharmacotherapy are effective treatments of depression in psychiatric and primary care settings (4), and treatment can translate into lower medical costs (5). The efficacy of antidepressant medications has been specifically demonstrated in HIV-positive patients (6–8). Anxiolytics, antipsychotics, and psychostimulants are used for the treatment of anxiety, psychosis, mania, and cognitive impairment, respectively (9, 10). Because HIV-positive patients usually receive a variety of antiretroviral and antibiotic medications, the concomitant administration of psychotropics has implications for possible drug-drug interactions, burden of care, and treatment costs. Thus, data regarding psychotropic use by HIV-positive patients can be informative from various perspectives and relevant to clinicians, pharmacologists, pharmacists, health care administrators, and policy makers.
The HIV Cost and Services Utilization Study surveyed a national probability sample of adults with known HIV infection who received medical care in 1996. Previous analyses of the database have provided information on the prevalence of psychiatric disorders and substance abuse (2), the impact of psychiatric disorders on quality of life (3), and the use of alcohol, drug, and mental health services by these patients (11). The purpose of this report is to describe the prevalence and pattern of use of common psychotropic medications among HIV-positive patients receiving medical care in the United States. In addition, we evaluated the relationship between psychotropic use and patient characteristics, such as age, gender, ethnicity, presence of psychiatric disorder, stage of HIV infection, and medical insurance status. Although this study was descriptive, certain specific hypotheses were advanced. It was predicted that psychotropic drug use would be strongly associated with the presence of a psychiatric disorder. Since people with coexisting mental disorders often have more severe symptoms (12) and are more likely to use multiple medications, it was predicted that comorbidity, defined as the presence of two or more psychiatric disorders in the same patient, would be associated with greater use of psychotropics. Since female and white (non-Hispanic) patients are more likely to be treated for mood and anxiety disorders (1, 13, 14), higher rates of medication use were predicted for these groups. Since having Medicaid or no health insurance was associated with lower use of health services than having Medicare (11, 15), lower use of psychotropic medications was expected for patients with Medicaid or no insurance. Possible effects of age and severity of HIV infection were also explored.
Method
Sample
The sample from the HIV Cost and Services Utilization Study included 2,864 patients who had made at least one medical visit from Jan. 5 to Feb. 29, 1996. Visits to emergency rooms or to military or prison medical providers were not included. The sample was representative of the 231,400 (95% confidence interval [CI]=162,800–300,000) adults with known HIV infection who were estimated to be receiving medical care in the 48 contiguous United States in 1996. Detailed descriptions of the HIV Cost and Services Utilization Study sample have been published elsewhere (15–18).
Of the 2,864 patients who received a baseline interview about medical status and services use, 2,466 (86.1%) received a follow-up interview 6 months later, which included the World Health Organization Composite International Diagnostic Interview Short Form (19), as a screening for major depression, dysthymia, generalized anxiety disorder, and panic disorder within the last 6 months. Of the 2,466 patients, 1,405 (57.0%) screened positive for any of these disorders or illicit substance use. These 1,405 patients, plus another 156 (who were a random sample of the 1,061 patients who had screened negative for the targeted mental disorder or illicit substance use) were selected to receive an additional, more detailed interview. This included the full long form of the Composite International Diagnostic Interview about presence of DSM-IV mental disorders in the last 6 months (20) and a survey of psychotropic medications used during the last 6 months. Of these 1,561 patients, 1,489 (95.4%) completed the interview during which the data relevant to this report were collected. All interviews were conducted by using computer-assisted personal interviewing instruments.
The patients were approached by HIV Cost and Services Utilization Study researchers only after the patients’ medical providers had obtained the patients’ permission. The patients then gave written informed consent to participate in the study. Each patient was paid $25 for completing the interview. The RAND institutional review board and, when applicable, local boards approved the protocol procedures and study forms.
Assessments
The HIV Cost and Services Utilization Study interview included modules on demographic characteristics, stage of HIV infection, presence of HIV-related symptoms, antiretroviral and antibiotic medications, and use of medical services. Collection methods have already been described elsewhere (17, 18). The 1,489 patients who constituted the sampled group analyzed for the present report were interviewed with the long form of the Composite International Diagnostic Interview (20) and completed a self-administered questionnaire about use of “medications for personal or emotional problems, such as emotions, nerves, alcohol, drugs, or mental health.” A comprehensive list of prescription and nonprescription psychotropic medications (both generic and brand names) was available to the patients for review. The patients were instructed to report only about medications they had taken regularly for a month or more during the last 6 months.
The patients were also asked whether they had visited a mental health provider (including a psychiatrist, psychologist, psychiatric social worker, psychiatric nurse, or marriage or family counselor) on an individual or family basis for emotional or personal problems or whether they had attended support or psychotherapy groups (other than any 12-step programs or groups primarily for alcohol or substance abuse) during the last 6 months. The patients who answered either question affirmatively were considered to have received psychosocial intervention.
The patients were asked about the presence of the following HIV-related symptoms during the last 6 months: new or persistent headaches; fevers, sweats, or chills; pain in the mouth, lips, or gums; white patches in the mouth; painful rashes or sores on the skin; nausea or loss of appetite; trouble with the eyes; sinus infection, pain, or discharge; numbness or tingling in the hands or feet; Kaposi’s sarcoma lesions; persistent cough or difficulty breathing; diarrhea or watery stools; and among women, an abnormal vaginal discharge. Patients reporting at least one of these symptoms but not full criteria for AIDS were classified as “symptomatic,” and individuals with none of these symptoms were classified as “asymptomatic.”
Statistical Analysis
Statistical weights were determined for each respondent to adjust for the study sampling design and interview implementation in order to generate estimates relevant to the entire reference population of HIV-infected individuals receiving medical care in the contiguous United States in 1996 (2, 16). Descriptive statistics was used to report the prevalence of use of psychotropic medications.
Logistic regression models were applied to identify the possible association of age, gender, ethnicity, HIV infection stage, mental disorder, or insurance status with use of psychotropic medications in general and antidepressants in particular.
Results
Use of Psychotropic Medications
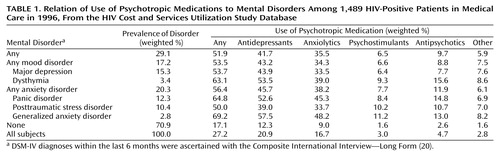
It was estimated that 27.2% of all HIV-positive patients in medical care in the contiguous United States in 1996 received at least one psychotropic drug during the last 6 months before the assessment (Table 1). Antidepressants were the most commonly used type of psychotropics (20.9% of all patients), followed by anxiolytic medications (16.7%), antipsychotics (4.7%), psychostimulants (3.0%), and other psychotropics (2.8%).
Use of Psychotropics by Mental Disorder
It was estimated that 29.1% of all patients suffered from at least one of the targeted disorders (i.e., major depression, dysthymia, generalized anxiety disorder, panic disorder, and posttraumatic stress disorder [PTSD]) in the 6 months before the interview (Table 1). The prevalence of anxiety disorders was 20.3%, and that of mood disorders was 17.2%. Major depression was the most common disorder (15.3%), followed by panic disorder (12.3%) and PTSD (10.4%).
Among patients with one or more mood disorders, 43.2% had taken antidepressants and 34.3% had taken anxiolytic medication during the last 6 months. Among patients with one or more anxiety disorders, the estimated use of antidepressants was 45.7%, and that of anxiolytics was 38.2%. Of the patients without a long-form Composite International Diagnostic Interview diagnosis of mood or anxiety disorder, 12.3% received antidepressants, 9.0% received anxiolytics, 2.6% received antipsychotics, and 1.6% received psychostimulant medications (Table 1).
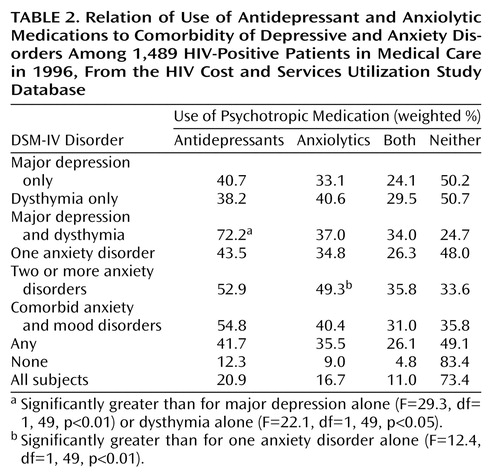
Use of antidepressants and anxiolytics tended to increase in the presence of comorbidity (Table 2). Thus, patients with both major depression and dysthymia were more likely to have taken antidepressants (72.2% of cases) than patients with only major depression or dysthymia (40.7% and 38.2%, respectively). Among patients with anxiety disorders, the presence of more than one anxiety disorder increased the rate of use of anxiolytics but not of antidepressants.
Number and Type of Medications
Selective serotonin reuptake inhibitors (SSRIs) were the most commonly used antidepressants among patients with any mental disorder (25.7%), followed by tricyclics (16.1%). Among patients with mood disorders, the rate of use of SSRIs (28.8%) was twice that of tricyclics (14.8%).
Benzodiazepines accounted for 66.3% of all anxiolytics. Of the patients with any mental disorder, 23.4% reported use of benzodiazepines. Alprazolam was the most commonly used benzodiazepine (10.9% of patients with any mental disorder), followed by diazepam (7.2%). Use of benzodiazepines was also reported by 5.6% of the patients who screened negative for mental disorders (2.4% took alprazolam, and 1.8% took diazepam).
Among patients taking psychotropics, the mean number of medications taken during the last 6 months was 2.8 (SD=2.0, range=1–24). Of the patients taking antidepressants, 63.0% also took at least one other type of psychotropic. Of the patients taking anxiolytics, 73.1% also took at least one other type of psychotropic.
Psychotropics and Antiretrovirals
Use of highly active antiretroviral therapy was reported by 61.9% of the patients. Of the patients receiving highly active antiretroviral therapy, 22.2% took an antidepressant (12.8% took an SSRI, and 9.3% took a tricyclic), 17.6% took an anxiolytic (11.0% took a benzodiazepine), 5.0% took an antipsychotic, and 3.0% took a psychostimulant. These rates are similar to those found among the patients not receiving highly active antiretroviral therapy, of whom 18.8% took an antidepressant (11.9% took an SSRI, and 5.2% took a tricyclic), 15.1% took an anxiolytic (10.4% took a benzodiazepine), 4.2% took an antipsychotic, and 3.0% took a psychostimulant.
Severity of HIV and Use of Psychotropics
No statistically significant differences in use of psychotropic drugs were found among the patients with asymptomatic HIV infection, symptomatic HIV infection, or AIDS.
Demographic and Clinical Characteristics
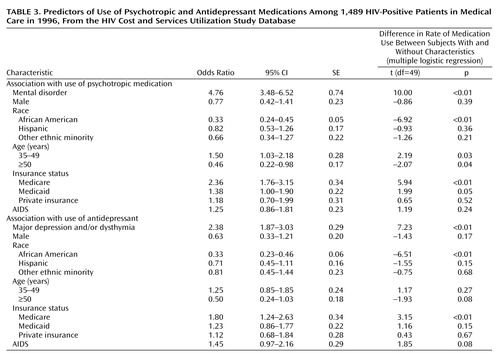
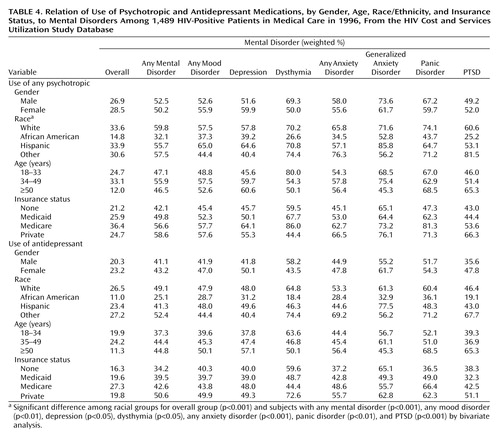
Use of psychotropic medications was greater among individuals with a mental disorder (odds ratio=4.76, 95% CI=3.48–6.52) or Medicare insurance coverage (odds ratio=2.36, 95% CI=1.76–3.15) or age 34–49 years (odds ratio=1.50, 95% CI=1.03–2.18) than among individuals without these characteristics (Table 3). No gender differences were found: 26.9% of men and 28.5% of women took psychotropic medications (Table 4). Use of psychotropic drugs was lower among individuals who identified themselves as African American (odds ratio=0.33, 95% CI=0.24–0.45) or were 50 years or older (odds ratio=0.46, 95% CI=0.22–0.98) (Table 3). No age differences were apparent, however, when patients with mental disorder only were considered (Table 4). Among patients with any mental disorder, the estimated rate of use of psychotropics was 59.8% for whites, 32.1% for African Americans, and 55.7% for Hispanics (Table 4).
Use of antidepressant medications was positively associated with the presence of a mood disorder (odds ratio=2.38, 95% CI=1.42–3.55) and Medicare insurance coverage (odds ratio=1.80, 95% CI=1.23–2.85) and negatively associated with self-identification as African American (odds ratio=0.33, 95% CI=0.23–0.45), compared to individuals without these characteristics (Table 3). Among patients with mood disorders (i.e., major depression and/or dysthymia), the rate of use of antidepressants was 47.9% among whites, 28.7% among African Americans, and 48.0% among Hispanics (Table 4).
Among the patients with mood disorders who did not receive antidepressant medication, the estimated use of psychosocial interventions (individual, group therapy, or a support group) was 25.2% for whites, 31.9% for African Americans, and 35.5% for Hispanics. Thus, overall, 61.0% of whites, 51.4% of African Americans, and 66.7% of Hispanics with mood disorders reported using antidepressant medications or some type of psychosocial intervention.
Discussion
To our knowledge, this is the first national probability study to examine the use of different types of psychotropic medications by HIV-positive patients. The results indicate that 27.2% of HIV-positive patients who received medical care in 1996 were treated with psychotropic medications in the 6 months before the study interview. This rate is consistent with that obtained through the baseline assessment of mental health services in the HIV Cost and Services Utilization Study sample (11), which was conducted 6 months before the survey of psychotropic use here reported. Antidepressants were the most commonly used psychotropic, followed by anxiolytics and, much less frequently, antipsychotics and psychostimulants. Among antidepressants, SSRIs were more commonly used than tricyclics. Most patients taking psychotropics took more than one class of medication. Comorbidity of mental disorders was associated with greater drug use. These results are generally consistent with previous reports regarding psychotropic prescribing patterns among patients in primary care and psychiatric practice settings (21, 22).
The estimated rates of mental health disorders during the 6 months before the interview are lower than the 12-month prevalence rate previously reported for the HIV Cost and Services Utilization Study sample (3). Several factors may have accounted for these lower rates, such as the shorter time frame (6 months), use of the long form of the Composite International Diagnostic Interview, which may be more specific than the short form used by Bing et al. (2, 23), and the repeated interviewing of the same patients with consequent possible regression to the mean and diagnostic attenuation.
We found that 43.9% of the HIV-positive patients with a DSM-IV diagnosis of major depression supported by the Composite International Diagnostic Interview took antidepressant medication. This rate is somewhat higher than expected on the basis of previous reports that only one-half of the primary care patients with major depression are accurately diagnosed (5, 22) and only one-half of those diagnosed are actually treated with antidepressants (24, 25). Some of these studies, however, were conducted in the mid-1980s, and there are indications that the rate of treatment of depression markedly increased in the 1990s (26). HIV-positive patients may be also more likely to be treated for psychiatric disorders, perhaps because of the extensive medical contacts related to HIV infection. More than one-half of the patients with a diagnosis of major depression under care for HIV infection reported not having been treated with antidepressants. How much this finding may be due to failure to recognize depression, failure to treat a diagnosed disorder, concern about polypharmacy and drug interactions in this population, or a preference for nonpharmacological interventions cannot be fully disentangled based on these data. On the basis of previous reports (5, 22), failure to recognize the disorder is rather common. However, a recent report that only about one-third of patients seeking treatment for mood or anxiety disorders may receive appropriate care (13) suggests that other causes besides failure to diagnose contribute to undertreatment. There are also indications that most primary care patients with depression prefer psychotherapy over medications (27). In our study, the rate of use of psychotherapy among depressed patients not receiving antidepressant medication was 25.2% for whites, 31.9% for African Americans, and 35.5% for Hispanics. The survey used a broad definition of “psychotherapy,” encompassing any contact with a mental health provider for individual or group therapy (including family and marriage counseling) and attendance at support group meetings. Even after an accounting for use of these psychosocial interventions, it appears that at least one-third of all patients with a mood disorder did not receive treatment.
Antidepressants are effective for both depressive and anxiety disorders, and this can explain the high use of these drugs by patients with anxiety disorders (Table 2). An estimated 12.3% of the patients with no mental disorder, based on the Composite International Diagnostic Interview, received antidepressant medication (Table 1). Given that 29.1% of all of the patients had a mental disorder and only 41.7% of them received antidepressants, it can be inferred that a sizable amount (41.8%) of all antidepressant use was by patients who did not have a diagnosis of a mental disorder according to the long-form Composite International Diagnostic Interview during the last 6 months. It is possible that a mental disorder had been previously present and that the medication was used to prevent recurrence (28). However, the average duration of antidepressant treatment is less than 3 months, and most patients discontinue medication within 6 weeks of starting treatment (28–30). Antidepressants could have been prescribed to treat subsyndromal forms of depression or anxiety (31) or to manage chronic pain (32). The study interview inquired about “medications for personal or emotional problems, such as emotions, nerves, alcohol, drugs, or mental health,” but the relationship between pain and depression is complex, and the two conditions can overlap (33). Likewise, anxiolytics are often used for managing insomnia, a common symptom in HIV-positive patients (34).
Use of multiple psychotropics was common. Although it cannot be ruled out that some medications were taken sequentially during the 6-month period, concomitant use was probably high. As expected, the concomitant use of antiretroviral and psychotropic medications was also common, with more than one-fifth of the patients receiving highly active antiretroviral therapy also taking an antidepressant. The study of the possible pharmacological interactions between antiretroviral and psychotropic medications has high clinical relevance (35). For instance, protease inhibitors can inhibit several cytochrome P-450 enzymes involved in the metabolism of psychotropics (36), resulting in a higher plasma concentration of these drugs (37).
After control for mental disorder, gender, age, insurance status, and presence of AIDS, African American patients were significantly less likely to have received psychotropic medications, and antidepressants in particular, than whites and Hispanics (Table 3 and Table 4). This finding is consistent with previous reports of less use of health care services for HIV infection by African Americans (15) and for mood and anxiety disorders in the general population (13, 38). This lower use of psychotropics by African Americans may be partly compensated by a higher reliance on psychosocial interventions. This is consistent with a recent survey showing that African Americans in primary care suffering from depression were twice as likely as white patients to prefer psychotherapeutic intervention than antidepressant medication (27). Unexpectedly, Hispanic ethnicity was not associated with lower use of psychotropics or antidepressants in this study. A national survey in the general population (i.e., not focused on HIV-positive patients) reported a greater unmet need of mental health services among Hispanics than among whites (14). Another study, however, found that, in the early and mid-1990s, the pharmacological treatment of depression dramatically increased among Hispanic patients but remained low among African Americans (39).
Contrary to our prediction, female sex was not associated with higher use of psychotropics in general or antidepressants in particular. Previous studies have reported that about two-thirds of psychotropic medication visits are for women, both in primary care and psychiatric settings. The present findings may reflect characteristics of HIV-positive men as being more likely to search for pharmacological treatment of mood and anxiety disorders than HIV-negative men. A less marked—but still significant—effect of age was also detected, with middle-age patients being more likely than older patients to have been treated with psychotropics (Table 3). This effect, however, was present only in the entire sample and disappeared when patients with a mental disorder only were analyzed (Table 4).
As expected, Medicare patients have a higher rate of psychotropic use (Table 3). Patients with Medicaid or without insurance, however, had rates of use that were comparable to those of patients with private insurance, thus indicating that for patients already in medical care these differences in insurance status do not significantly affect the use of psychotropics.
In addition to the study limitations mentioned, a few others also need to be pointed out. The severity of psychopathology was not assessed, and this limits inferences on the adequacy of treatment. For instance, undertreatment of severe depression would be of greater concern than undertreatment of milder forms. Also, chart diagnoses made by the patients’ providers were not obtained. Information about the prescribers of psychotropic medications (e.g., family doctor, psychiatrist), duration of treatment, and dose were not available.
In conclusion, this study of a national probability sample of HIV-positive patients found that psychotropic medications, and antidepressants and anxiolytics in particular, were commonly used by HIV-positive patients receiving medical care in the United States. However, more than one-half of the patients suffering from major depression were not treated with antidepressants, even though a substantial portion of those not receiving medication reported use of some type of psychosocial intervention. African Americans were less likely to have been treated with psychotropic medications, thus adding to other data indicating differences in health care among ethnic groups.
 |
 |
 |
 |
Received Jan. 18, 2002; revision received Aug. 29, 2002; accepted Sept. 17, 2002. From the Division of Services and Intervention Research, NIMH; RAND, Santa Monica, Calif.; and the Center for AIDS Research, Education and Services, Charles R. Drew University, Los Angeles. Address reprint requests to Dr. Vitiello, NIMH, Room 7147, 6001 Executive Blvd., MSC 9633, Bethesda, MD 20892-9633; [email protected] (e-mail). The HIV Cost and Services Utilization Study was conducted under cooperative agreement HS-08578 between RAND and the Agency of Healthcare Research and Quality (formerly Agency of Health Care Policy and Research) (principal investigator: Dr. M.F. Shapiro, co-principal investigator: Dr. S.A. Bozzette), with additional funding provided by the Health Services Resources Administration and NIH, Bethesda, Md. (NIMH, the National Institute of Drug Abuse, and the Office of Research on Minority Health through the National Institute for Dental Research). Dr. Bing received support from NIMH as a UCLA Faculty Scholar in Mental Health Services Research (MH-00990) and through the California Universitywide AIDS Research Program (IS99-DREW203). The authors thank Joan Tucker and Geoffrey Joyce for their comments and suggestions on the article. The opinions and assertions contained in this report are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Health and Human Services, the Agency of Healthcare Research and Quality, or NIH.
1. Pincus HA, Tanielian TL, Marcus SC, Olfson M, Zarin DA, Thompson J, Zito JM: Prescribing trends in psychotropic medications. JAMA 1998; 279:526-531Crossref, Medline, Google Scholar
2. Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Turner BJ, Eggan F, Beckman R, Vitiello B, Morton SC, Orlando M, Bozzette SA, Ortiz-Barron L, Shapiro M: Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry 2001; 58:721-728Crossref, Medline, Google Scholar
3. Sherbourne CD, Hays RD, Fleishman JA, Vitiello B, Magruder KM, Bing EG, McCaffrey D, Burnam A, Longshore D, Eggan F, Bozzette SA, Shapiro MF: Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry 2000; 157:248-254Link, Google Scholar
4. Schulberg HC, Katon W, Simon GE, Rush AJ: Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry 1998; 55:1121-1127Crossref, Medline, Google Scholar
5. Revicki DA, Simon GE, Chan K, Katon W, Heiligenstein J: Depression, health-related quality of life, and medical cost outcomes of receiving recommended levels of antidepressant treatment. J Fam Pract 1998; 47:446-452Medline, Google Scholar
6. Rabkin JG, Wagner GJ, Rabkin R: Fluoxetine treatment for depression in patients with HIV and AIDS: a randomized, placebo-controlled trial. Am J Psychiatry 1999; 156:101-107Link, Google Scholar
7. Elliott AJ, Uldall KK, Bergam K, Russo J, Claypoole K, Roy-Byrne PP: Randomized, placebo-controlled trial of paroxetine versus imipramine in depressed HIV-positive outpatients. Am J Psychiatry 1998; 155:367-372Abstract, Google Scholar
8. Gill D, Hatcher S: Antidepressants for depression in people with physical illness. Cochrane Database Syst Rev 2000; 2:CD001312Google Scholar
9. van Dick CH, McMahon TJ, Rosen MI, O’Malley SS, O’Connor PG, Lin CH, Pearsall HR, Woods SW, Kosten TR: Sustained-release methylphenidate for cognitive impairment in HIV-1-infected drug abusers: a pilot study. J Neuropsychiatry Clin Neurosci 1997; 9:29-36Crossref, Medline, Google Scholar
10. Wagner GJ, Rabkin JG, Rabkin R: Dextroamphetamine as a treatment for depression and low energy in AIDS patients: a pilot study. J Psychosom Res 1997; 42:407-411Crossref, Medline, Google Scholar
11. Burnam MA, Bing E, Morton SC, Sherbourne C, Fleishman J, London AS, Vitiello B, Stein M, Bozzette SA, Shapiro MF: Use of mental health and substance abuse treatment services among adults with HIV in the United States. Arch Gen Psychiatry 2001; 58:729-736Crossref, Medline, Google Scholar
12. Wells KB, Burnam MA, Rogers W, Hays R, Camp P: The course of depression in adult outpatients: results from the Medical Outcomes Study. Arch Gen Psychiatry 1992; 49:788-794Crossref, Medline, Google Scholar
13. Young AS, Klap R, Sherbourne CD, Wells KB: The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry 2001; 58:55-61Crossref, Medline, Google Scholar
14. Wells K, Klap R, Koike A, Sherbourne C: Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatry 2001; 158:2027-2032Link, Google Scholar
15. Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, Athey LA, Keesey JW, Goldman DP, Berry SH, Bozzette SA: Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA 1999; 281:2305-2315Crossref, Medline, Google Scholar
16. Bozzette SA, Berry SH, Duan N, Frankel MR, Leibowitz AA, Lefkowitz D, Emmons CA, Senterfitt JW, Berk ML, Morton SC, Shapiro MF (HIV Cost and Services Utilization Study Consortium): The care of HIV-infected adults in the United States. N Engl J Med 1998; 339:1897-1904Crossref, Medline, Google Scholar
17. Shapiro MF, Berk ML, Berry SH, Emmons CA, Athey LA, Hsia DC, Leibowitz AA, Maida CA, Marcus M, Perlman JF, Schur CL, Schuster MA, Senterfitt JW, Bozzette SA: National probability samples in studies of low-prevalence diseases, part I: perspectives and lessons from the HIV Cost and Services Utilization Study. Health Serv Res 1999; 34:951-968Medline, Google Scholar
18. Frankel MR, Shapiro MF, Duan N, Morton SC, Berry SH, Brown JA, Burnam MA, Cohn SE, Goldman DP, McCaffrey DF, Smith SM, St Clair PA, Tebow JF, Bozzette SA: National probability samples in studies of low-prevalence diseases, part II: designing and implementing the HIV Cost and Services Utilization Study sample. Health Serv Res 1999; 34:969-992Medline, Google Scholar
19. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods in Psychiatr Res 1998; 7:171-185Crossref, Google Scholar
20. World Health Organization: Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, WHO, 1997Google Scholar
21. Pincus HA, Zarin DA, Tanielian TL, Johnson JL, West JC, Pettit AR, Marcus SC, Kessler RC, McIntyre JS: Psychiatric patients and treatments in 1997: findings from the American Psychiatric Practice Research Network. Arch Gen Psychiatry 1999; 56:441-449Crossref, Medline, Google Scholar
22. Blacker CVR, Clare AW: Depression disorder in primary care. Br J Psychiatry 1987; 150:737-751Crossref, Medline, Google Scholar
23. Orlando M, Burnam MA, Sherbourne CD, Morton SC, London AS, Hays RD, Bing EG: Brief screening of psychiatric disorders among a national sample of HIV-positive adults: concordance between the Composite International Diagnostic Interview (CIDI) and the CIDI Short Form (CIDI-SF). Int J Methods Psychiatr Res 2001; 10:97-107Crossref, Google Scholar
24. Linden M, Lecrubier Y, Bellantono C, Benkert O, Kisely S, Simon G: The prescribing of psychotropic drugs by primary care physicians: an international collaborative study. J Clin Psychopharmacol 1999; 19:132-140Crossref, Medline, Google Scholar
25. Simon GE, Von Korff M, Rutter CM, Peterson DA: Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry 2001; 58:395-401Crossref, Medline, Google Scholar
26. Olfson M, Marcus SC, Druss B, Elison L, Tanielian T, Pincus HA: National trends in outpatient treatment of depression. JAMA 2002; 287:203-209Crossref, Medline, Google Scholar
27. Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB: Treatment preferences among depressed primary care patients. J Gen Intern Med 2000; 15:527-534Crossref, Medline, Google Scholar
28. Joffe RT, Iskedjian M, Einarson TR, O’Brien BJ, Stang MR: Examining the Saskatchewan Health Drug Database for antidepressant use: the case of fluoxetine. Can J Clin Pharmacol 2001; 8:146-152Medline, Google Scholar
29. Lawrenson RA, Tyrer F, Newson RB, Farmer RDT: The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. J Affect Disord 2000; 59:149-157Crossref, Medline, Google Scholar
30. Katon W, von Korff M, Lin E, Bush T, Ormel J: Adequacy and duration of antidepressant treatment in primary care. Med Care 1992; 30:67-76Crossref, Medline, Google Scholar
31. Rapaport MH, Judd LL: Minor depressive disorder and subsyndromal depressive symptoms: functional impairment and response to treatment. J Affect Disord 1998; 48:227-232Crossref, Medline, Google Scholar
32. Shlay JC, Chaloner K, Max MB, Flaws B, Reichelderfer P, Wentworth D, Hillman S, Brizz B, Cohn DL: Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: a randomized controlled trial. JAMA 1998; 280:1590-1595Crossref, Medline, Google Scholar
33. Evans S, Ferrando S, Sewell M, Goggin K, Fishman B, Rabkin J: Pain and depression. Psychosomatics 1998; 39:528-535Crossref, Medline, Google Scholar
34. Rubinstein ML, Selwyn PA: High prevalence of insomnia in an outpatient population with HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 19:260-265Crossref, Medline, Google Scholar
35. Ouellet D, Hsu A, Qian J, Lamm JE, Cavanaugh JH, Leonard JM, Granneman GR: Effect of fluoxetine on pharmacokinetics of ritonavir. Antimicrob Agents Chemother 1998; 42:3107-3112Crossref, Medline, Google Scholar
36. von Moltke LL, Greenblatt DJ, Grassi JM, Granda BW, Duan SX, Fogelman SM, Daily JP, Harmatz JS, Shader RI: Protease inhibitors as inhibitors of human cytochrome P450: high risk associated with ritonavir. J Clin Pharmacol 1998; 38:106-111Crossref, Medline, Google Scholar
37. Greenblatt DJ, von Moltke LL, Daily JP, Harmatz JS, Shader RI: Extensive impairment of triazolam and alprazolam clearance by short-term low-dose ritonavir: the clinical dilemma of concurrent inhibition and induction. J Clin Psychopharmacol 1999; 19:293-296Crossref, Medline, Google Scholar
38. Melfi CA, Croghan TW, Hanna MP, Robinson RL: Racial variation in antidepressant treatment in a Medicaid population. J Clin Psychiatry 2000; 61:16-21Crossref, Medline, Google Scholar
39. Skaer TL, Sclar DA, Robison LM, Galin RS: Trends in the rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992-1997. Clin Ther 2000; 22:1575-1589Crossref, Medline, Google Scholar



