Predictors of Self-Neglect in Community-Dwelling Elders
Abstract
OBJECTIVE: The study assessed the contribution of depressive symptoms and cognitive impairment to the prediction of self-neglect in elderly persons living in the community. METHOD: Data were drawn from the New Haven Established Populations for Epidemiologic Studies of the Elderly cohort, which included 2,812 community residents age 65 years and older in 1982. The principal outcome examined was the incidence of self-neglect, corroborated by the state’s investigation, during 9 years of follow-up (1982–1991). RESULTS: Among the 2,161 subjects included in the analysis, 92 corroborated cases of self-neglect occurred from 1982 to 1991. The prevalence of clinically significant depressive symptoms at baseline (score ≥16 on the Center for Epidemiologic Studies Depression Scale [CES-D]) was 15.4%, and the prevalence of clinically significant cognitive impairment (four or more errors on the Pfeiffer Short Portable Mental Status Questionnaire) was 7.5%. Subjects with clinically significant depressive symptoms and/or cognitive impairment were more likely than others to experience self-neglect. Clinically significant depressive symptoms and cognitive impairment remained significant predictors of self-neglect in a multivariate model that included age, gender, race, and income. A final model for self-neglect constructed with stepwise selection of risk factors included depressive symptoms and cognitive impairment, as well as male gender, older age, income less than $5,000 per year, living alone, history of hip fracture, and history of stroke. CONCLUSIONS: Elderly individuals living in the community who experience clinically significant depressive symptoms and/or cognitive impairment may be at risk for the development of self-neglect and may become candidates for intervention.
The past few decades of research have established two categories of psychiatric illness in late life—depression and dementia—as conditions of protean clinical expressions and consequences (1–7). Depressive symptoms are associated with suicide in elderly persons (1) and have also been shown to adversely influence measures of functional status (2–5) and quality of life in geriatric patients (5, 6). The clinical implications of cognitive impairment in elderly persons may be even farther ranging (7). However, in contrast to these extensively studied clinical phenomena, the social sequelae of depression and dementia, or their implications for elderly individuals living in the community, are not well understood (8).
A recent focus of social-epidemiological investigation of community-dwelling elders has been in the area of self-neglect (8–13). Described by early authors as a “senile breakdown in standards” (11), self-neglect is a multifaceted behavioral entity involving inability or refusal to attend adequately to one’s own health, hygiene, nutrition, or social needs; it is distinguished from neglect proper, which is a form of elder abuse (8).
Self-neglect is assumed to result from mental, physical, and social disturbances and also to promote such disturbances (10–12). Although information on the prevalence of self-neglect is limited to a single population-based study (8, 9, 14), related referrals to an adult protective services agency have been shown to increase with age (14). In addition, self-neglect has implications for excess mortality and institutionalization among the frailest elderly individuals living in the community (9).
In the present study we considered the possibility that elderly persons who have depressive symptoms, cognitive impairment, or both might lack the energy, motivation, integrative memory, or judgment to care for themselves adequately; these individuals could therefore be at heightened risk to fall into a state of self-neglect. To examine this question we sought to evaluate the contribution of depressive symptoms and cognitive impairment to the prediction of self-neglect by using longitudinal data from community-dwelling elders in New Haven, Connecticut, who participated in the Established Populations for Epidemiologic Studies of the Elderly developed by the National Institute on Aging (15). We hypothesized that depressive symptoms and cognitive impairment would each predict self-neglect. We also hypothesized that these mental status factors would contribute to the prediction of self-neglect as components of a multivariate model that would include sociodemographic and medical risk factors, such as living alone, advanced age, and medical burden (14).
Method
Study Cohort
The study was based on longitudinal data from a community-based sample of men and women aged 65 years and over who were living in New Haven, Connecticut, in 1982. Participants were part of the Established Populations for Epidemiologic Studies of the Elderly program of the National Institute on Aging (15). The cohort of 2,812 elderly adults was selected by using stratified probability sampling methods, with strata defined by three types of housing: community housing, age- and income-restricted public housing, and age-restricted private housing.
Sample weights were derived to account for the oversampling of subjects in the age-restricted private housing stratum and the oversampling of men in the age-restricted private housing and community housing strata. Weighted analyses of these data permitted generalization of findings to the population of community-dwelling elderly adults in New Haven.
Written informed consent was obtained from subjects after the study procedures had been fully explained. Participants underwent in-person baseline interviews at the time of enrollment in 1982. Interviews covered broad domains of demographic, medical, functional, and psychosocial information and also included the use of standardized instruments assessing depressive symptoms, cognitive functioning, and chronic medical conditions. These instruments are described in greater detail in a later section.
After the baseline interviews in 1982, follow-up in-person interviews that used the same battery of instruments were conducted in 1985, 1988, and 1994. Telephone interviews also took place in the years between the in-person assessments. The analyses presented in this study are based on a follow-up period of 9 years, starting in 1982 and concluding on December 31, 1991.
Identifying Cases of Self-Neglect
In Connecticut, as in other states, the elderly protective services agency represents the final safety net for elderly individuals whose needs have eluded other medical or social resources (14). The Connecticut referrals to the elderly protective services agency, because of either abuse or neglect, come from mandatory reporters, such as health care workers having direct contact with clients, and from nonmandatory reporters, including family members, neighbors, clergy, and postal or utility workers. The nonmandatory reporters may be anonymous.
The operational definition of self-neglect in Connecticut is the inability of an elderly person to provide for him- or herself the services necessary to maintain good health; neglect refers to the failure of an elderly person to receive essential services from a responsible caregiver; and exploitation involves taking advantage of an elderly person for personal gain.
The assessment of each referral of an elderly community resident (i.e., one not living in a nursing home or other institutional facility) is shared by the state ombudsman on aging and protective services staff. The ombudsman has initial contact with the client and investigates all cases of suspected abuse, neglect, or self-neglect in the community. If a reported problem is corroborated, elderly protective services staff either manage the case or arrange for referrals.
To determine which cohort members had corroborated cases of self-neglect, information abstracted from ombudsman records in the New Haven office was matched to cohort data in a manner ensuring the confidentiality of subjects. Details on the matching process, the method by which confidentiality was ensured, and descriptions of substudies conducted to ensure reliability and quality of data are available elsewhere (9).
Measures
Corroborated self-neglect
The principal outcome measure for this study was the incidence of self-neglect during the 9-year follow-up period (1982–1991). Only incidents of suspected self-neglect corroborated by the state’s ombudsman were coded as cases of self-neglect. Suspected self-neglect that was not corroborated and instances of elder abuse were coded as noncases in the analyses.
Since the outcome period for the study began at the point of the initial investigation, the time periods in which data were viewed as predictive of self-neglect were limited to those occurring before the state’s investigation. The rationale for this approach was that although the same incident could be reported by more than one complainant (e.g., physician, neighbor) and multiple investigations could be undertaken, once self-neglect is identified, additional investigations may be more a function of agency surveillance than a new source of data on subject risk factors. Also, the investigation itself might result in changes in the subject’s behavior or initiation of supports that could change the predictive variables under study.
Depressive symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D) (16) was used to assess depressive symptoms at the baseline and in-person follow-up assessments. Previous research has suggested that a score ≥16 on the CES-D is a useful screen for major depression (16), although that score does not itself represent a clinical diagnosis.
Cognitive functioning
Cognitive functioning was assessed at the baseline and in-person follow-up interviews by using the Pfeiffer Short Portable Mental Status Questionnaire (17). On the basis of previous experience with this 10-item scale, subjects scoring four or more errors were classified as screening positive for cognitive impairment (18). However, the Short Portable Mental Status Questionnaire score alone does not confer a clinical diagnosis of dementia.
Sociodemographic characteristics
Information on demographic characteristics, including gender, age, race, education, and income, was obtained at the baseline interview. Marital status and living situation (alone versus not alone) were assessed at baseline and at each of the in-person follow-up interviews.
Chronic medical conditions
A standardized assessment was used to gain information on history of chronic medical conditions, including arthritis, cancer, diabetes, hip fracture, myocardial infarction, and hypertension. At baseline the prevalence of each condition was ascertained by questions inquiring whether a doctor had ever told the subject that he or she had the condition. At each annual follow-up telephone interview the subject was asked whether a doctor had said since the last interview that he or she had the condition. For each disorder, data were updated at the 1985 and 1988 follow-ups to reflect information from the preceding 3-year interval.
Analysis
Descriptive statistics were calculated for the baseline characteristics of the 2,161 cohort members included in the statistical analysis. A pooled logistic regression model was used to examine the relationship between potential risk factors and the time to the first investigation for self-neglect (19, 20). The time to an outcome event is analyzed in this method by pooling separate records that represent independent time periods of observation.
For this study the 9-year follow-up period was divided into three nonoverlapping observation periods from 1982 to 1985, 1985 to 1988, and 1988 to 1991. A 3-year time interval was used as the period of observation to allow for information on the time-varying risk factors to be updated with data obtained at the in-person interviews in 1985 and 1988. The initial occurrence of the outcome, corroborated self-neglect, was determined across the three time periods with data from the files of the protective services agency. Subjects who were not investigated for self-neglect and survived the entire 9-year follow-up period contributed three observations to the analysis, with the outcome at each interval coded as no self-neglect. If a subject was investigated for self-neglect that was subsequently corroborated, he or she would contribute one to three observations, depending on the interval in which the initial investigation occurred. The study outcome reflects the number of subjects experiencing a first investigation of self-neglect divided by the total time until the first investigation occurred.
The pooled logistic regression method also accounts for right censoring by incorporating partial information on subjects with incomplete follow-up data. Cohort members who died during the 9-year follow-up period were included in the analysis until the 3-year interval in which the death occurred. In addition, subjects who were admitted to skilled nursing facilities during any of the 3-year intervals were included in the analysis for the intervals during which they spent the entire time period living at home, i.e., were at risk for self-neglect.
The incidence of corroborated self-neglect per person-year was calculated by dividing the weighted number of corroborated self-neglect investigations by the weighted number of follow-up periods. This ratio was divided by 3 to obtain the incidence of self-neglect per person-year. The crude incidence rate ratio for each risk factor was estimated from the odds ratios computed in the pooled logistic regression models. These models included the risk factor and a set of dummy variables that reflected the time interval. Both stable risk factors (gender, race, education, income) and time-varying risk factors (marital status, living situation, health history, cognitive functioning, depression) were examined in these analyses. Each model was also tested for significant (p<0.05) interactions between the time interval and the risk factor.
The second set of models estimated the association between each risk factor and the incidence of self-neglect, while adjusting for age, gender, race, and income. Finally, a combined model was constructed by using a stepwise selection procedure among the risk factors. This procedure required significance levels of 0.25 for entering the model and 0.15 for staying in the model. All hypothesis testing and multivariate analyses were conducted with SUDAAN software (21) to account for the complex sampling design. This software uses Taylor linearization to estimate the variance-covariance matrix of estimated parameters. The robust variance estimation method used in SUDAAN does not rely on distributional assumptions for computing p values and confidence intervals (CIs) (22).
Results
The aim of these analyses was to measure the contribution of depressive symptoms and cognitive impairment to the prediction of corroborated cases of self-neglect in the Established Populations for Epidemiologic Studies of the Elderly New Haven cohort. Data from 2,161 of the original cohort of 2,812 subjects were included in the analysis.
Cohort members who died (N=474) or entered skilled nursing facilities (N=100) during the first interval were excluded from the analysis. In addition, 77 subjects had missing data at the baseline (N=51) and follow-up (N=26) visits.
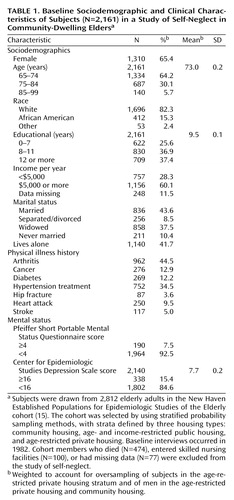
Baseline descriptive data for these subjects are summarized in Table 1. Overall, the subjects were elderly (mean age=73 years), white (82.3%), poor (28.3% with an annual income of less than $5,000), and female (65.4%). The prevalence of clinically significant depressive symptoms (CES-D Scale score ≥16) was 15.4%. A total of 7.5% of subjects reached the threshold for clinically significant cognitive impairment (four or more errors on the Pfeiffer Mental Status Questionnaire). Various chronic medical conditions were also reported in the group, with arthritis the most prevalent (44.5%).
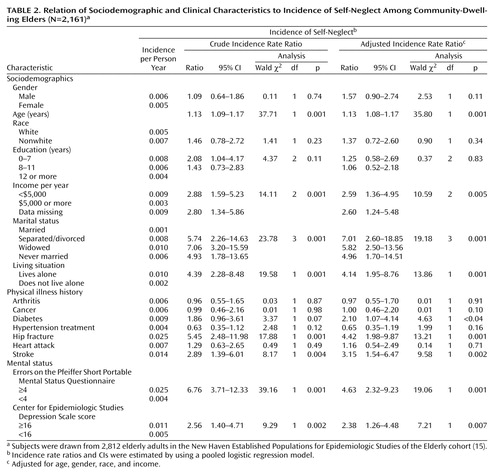
From 1982 to 1991 there were 92 cases of corroborated self-neglect for the 2,161 subjects in the analysis, resulting in a weighted crude incidence of seven cases of self-neglect per 1,000 person-years. The crude incidence of self-neglect according to the subjects’ sociodemographic and clinical characteristics, the incidence rate ratio (i.e., odds ratio), and the 95% CI associated with each characteristic are displayed in Table 2.
Subjects with clinically significant depressive symptoms (CES-D Scale score ≥16) at baseline or follow-up were more likely than others to undergo a corroborated self-neglect investigation (odds ratio=2.56, 95% CI=1.40–4.71; Wald χ2=9.29, df=1, p<0.002). The incidence of self-neglect was also higher among subjects with cognitive impairment than among those without cognitive impairment (odds ratio=6.76, 95% CI=3.71–12.33; Wald χ2=39.16, df=1, p<0.001). Depressive symptoms and cognitive impairment remained significant predictors of self-neglect after adjustment for age, gender, race, and income (adjusted odds ratio for depressive symptoms=2.38, 95% CI=1.26–4.48; Wald χ2=7.21, df=1, p<0.007; adjusted odds ratio for cognitive impairment=4.63, 95% CI=2.32–9.23; Wald χ2=19.06, df=1, p<0.001).
As presented in Table 2, several non-mental-status factors, such as advanced age and poor socioeconomic status (indicated by lower education and income levels) were significantly associated with the incidence of corroborated self-neglect. Reduced social ties, including not being married and living alone, were also associated with the incidence of self-neglect, with crude incidence rate ratios ranging from 4.4 to 7.1. Among physical health variables, subjects with a history of hip fracture (odds ratio=5.45, 95% CI=2.48–11.98; Wald χ2=17.88, df=1, p<0.001) or a history of stroke (odds ratio=2.89, 95% CI=1.39–6.01; Wald χ2=8.17, df=1, p<0.01) were also at increased risk for self-neglect.
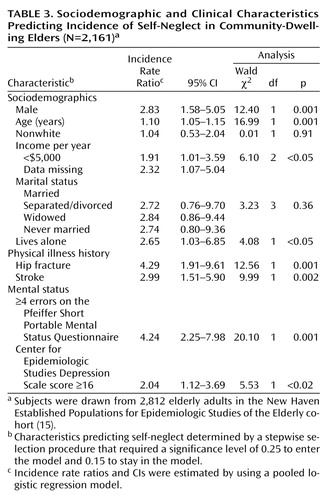
Incidence rate ratios for the final combined model for self-neglect are displayed in Table 3. Depressive symptoms at the CES-D Scale score ≥16 level and cognitive impairment at the level of four or more errors on the Short Portable Mental Status Questionnaire were again significant predictors of corroborated self-neglect in the final model (adjusted odds ratio for depression=2.04, 95% CI=1.12–3.69; Wald χ2=5.53, df=1, p<0.02; adjusted odds ratio for cognitive impairment=4.24, 95% CI=2.25–7.98; Wald χ2=20.10, df=1, p<0.001). The final model also included several demographic characteristics (older age, male gender, low income, and living alone, but not race), and two additional clinical characteristics (history of hip fracture, history of stroke) that were significantly associated with the rate of self-neglect. Individuals with both mental status factors had a rate of self-neglect that was 8.6 times higher than those with a CES-D Scale score <16 and less than four errors on the Short Portable Mental Status Questionnaire, but there were no significant interactive effects between the two factors.
For purposes of analysis, activities of daily living were viewed as defining components of the self-neglect syndrome. Thus, they were not included in the model. However, we investigated whether individual activities of daily living, such as bathing, grooming, toileting, etc., mediated the effects of depressive symptoms or cognitive impairment in the final model; we found that they did not. Only the ability to transfer from bed to chair slightly reduced the effect of depression (adjusted odds ratio for depression=1.78, 95% CI=0.94–3.36; Wald χ2=3.11, df=1, p<0.08).
Finally, a sensitivity analysis was performed by constructing a second data set that used covariate (i.e., time-varying) information from the preceding interview in cases where the subject was missing that information at a particular visit. This procedure increased the number of corroborated self-neglect cases from 92 to 108. The resulting rate ratio for depressive symptoms was larger than the original model estimate (adjusted odds ratio for depressive symptoms=2.39, 95% CI=1.33–4.30; Wald χ2=8.53, df=1, p<0.004), while the rate ratio for cognitive impairment became somewhat smaller but remained significant (adjusted odds ratio for cognitive impairment=3.94, 95% CI=2.13–7.28; Wald χ2=19.27, df=1, p<0.001).
Discussion
In this study clinically significant depressive symptoms and cognitive impairment predicted self-neglect in an epidemiological sample of community-dwelling elderly residents. Depressive symptoms and cognitive impairment were independent predictors and also contributed to multivariate models that took into account broader social and medical contexts.
That cognitive impairment proved a stronger predictor of self-neglect than depressive symptoms was not surprising, as cognitively impaired persons have difficulty taking care of themselves because of the nature of their deficits in memory and judgment. However, the prevalence of screen-positive depressive symptoms at baseline was twice that of cognitive impairment while remaining within the range of reported prevalences of clinically significant depression in elderly patients in primary care (23). Individuals with both clinically significant depressive symptoms and cognitive impairment had an enhanced risk of self-neglect. However, the reasons for that relationship did not emerge, that is, there were no significant interactive effects between the two mental status risk factors. Further investigation is needed to clarify these relationships.
Among the limitations of this study is the potential for overlapping definitions or tautologies (i.e., behaviors inherently related to self-neglect predict self-neglect). We therefore adopted a narrow definition of self-neglect—that used by Connecticut in its case determinations—and included only corroborated cases in the analysis. This strategy was justified by evidence that individuals with corroborated self-neglect differ not only from those never suspected of self-neglect but also from those for whom self-neglect is investigated but not corroborated. For example, Lachs et al. (9), using data from the same cohort, found that persons with noncorroborated allegations of abuse or neglect did not have survival rates significantly different than those never seen by the protective services agency.
To minimize tautologies, deficiencies in activities of daily living were excluded from the predictive models and were viewed as being within the definition of self-neglect. For example, low motivation to perform activities of daily living is a core feature of self-neglect, and poor grooming may be its most tangibly visible feature. Also, in the final model, depressive symptoms and cognitive impairment both contributed to self-neglect independent of the level of functioning in activities of daily living. In contrast to activities of daily living, “living alone” was treated as a correlate of self-neglect, because the Connecticut elderly protective services agency was able to identify a group of elderly persons with a corroborated case of self-neglect who did not live alone.
Another issue concerned the small number of new self-neglect cases, which resulted partly from the requirement for corroboration. However, after missing covariates were duplicated, the number of cases increased from 92 to 108. For other reasons, it may be difficult to infer from these data the true extent of self-neglect in community elders. For example, although this study focused on incidence, prevalence may be a more appropriate paradigm for self-neglect, because it is a condition from which individuals are unlikely to revert; stated differently, most incident cases become prevalence cases. Moreover, in the original investigation involving this cohort, 7.4% were referred to elderly protective services over 11 years; of these referrals, 75% had corroborated self-neglect cases, suggesting a “geriatric prevalence” of about 5% for the follow-up period (14).
Other limitations of this study included the use of dimensional screening instruments to assess depressive symptoms, cognitive impairment, and the lack of clinically derived diagnoses. Consequently, the terms “depressive symptoms” or “cognitive impairment” do not refer to specific diagnoses. However, the instruments used have been validated in relation to clinical diagnoses (16–18), and cutoff points were selected to ensure a likelihood of clinically significant depression or cognitive impairment.
Nevertheless, the findings that mental status factors contribute to the prediction of self-neglect had considerable strength. Also, the New Haven sample was a representative one, at least with respect to corroboration rates. Data from the Connecticut elderly protective services agency showed that in 1992, just after the conclusion of this study, the corroboration rate for self-neglect investigations in the state’s south central region (including New Haven) was 55.6%, similar to rates reported for the state as a whole (X. Dong, personal communication, 2001).
The study findings have important lessons for clinicians, who may be helped to recognize the antecedents of elderly self-neglect. As the population ages, psychiatrists and other physicians in the community are increasingly being asked to comment on elderly patients’ functional status and safety. In some states, physicians are mandatory reporters of abuse or neglect. Although the study data are preliminary and need to be replicated in the context of other important issues, such as alcoholism, a profile has begun to emerge of community-dwelling elders—i.e., low-income men, living alone, who have had a stroke or fracture—for whom depressive symptoms and cognitive impairment may be likely to contribute to self-neglect. Such information may promote early detection and interventions targeting preventable suffering and mortality.
 |
 |
 |
Received May 3, 2001; revision received March 13, 2002; accepted May 1, 2002. From Weill Medical College of Cornell University, New York. Address reprint requests to Dr. Abrams, Payne Whitney Clinic, New York Presbyterian Hospital–Cornell Medical Center, Box 140, 525 E. 68th St., New York, NY 10021; [email protected] (e-mail). Supported by NIMH grants MH-49762 and MH-51842 and grant AG-00853-03 from the National Institute on Aging. The authors thank Shelly O’Brien, M.S.W., and the staff of the State of Connecticut Elderly Protective Services Division for their assistance with the study.
1. Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED: Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996; 153:1001-1008Link, Google Scholar
2. Bruce ML, Seeman TE, Merrill SS, Blazer DG: The impact of depressive symptomatology on physical disability: MacArthur studies of successful aging. Am J Public Health 1994; 84:1796-1797Crossref, Medline, Google Scholar
3. Laukkanen P, Kauppinen M, Era P, Heikkinen E: Factors related to coping with physical and instrumental activities of daily living among people born in 1904-1923. Int J Geriatr Psychiatry 1993; 8:287-296Crossref, Google Scholar
4. Alexopoulos GS, Vrontou C, Kakuma T, Meyers BS, Young RC, Klausner E, Clarkin J: Disability in geriatric depression. Am J Psychiatry 1996; 153:877-885Link, Google Scholar
5. Abrams RC, Alexopoulos GS, Spielman LA, Klausner E, Kakuma T: Personality disorder symptoms predict declines in global functioning and quality of life in elderly depressives. Am J Geriatr Psychiatry 2001; 9:67-71Crossref, Medline, Google Scholar
6. Fredman L, Weissman MM, Leaf PJ, Bruce ML: Social functioning in community residents with depression and other psychiatric disorders: results of the New Haven ECA study. J Affect Disord 1988; 15:103-112Crossref, Medline, Google Scholar
7. Willis SL: Cognition and everyday competence, in Annual Review of Gerontology and Geriatrics, vol 11. Edited by Schaie KW, Lawton MP. New York, Springer, 1991, pp 80-109Google Scholar
8. Lachs MS, Williams C, O’Brien S, Hurst L, Horowitz R: Risk factors for reported elder abuse and neglect: a nine-year observational cohort study. Gerontologist 1997; 37:469-474Crossref, Medline, Google Scholar
9. Lachs MS, Williams CS, O’Brien S, Pillemer KA, Charlson ME: The mortality of elder mistreatment. JAMA 1998; 280:428-432Crossref, Medline, Google Scholar
10. Rathbone-McCuan E, Fabian DR (eds): Self-Neglecting Elders: A Clinical Dilemma. Westport, Conn, Auburn House, 1992Google Scholar
11. McMillan D, Shaw P: Senile breakdown in standards of personal and environmental cleanliness. Br Med J 1966; 2:1032-1037Crossref, Medline, Google Scholar
12. Granick R, Zeman FD: The aged recluse—an exploratory study with particular reference to community responsibility. J Chronic Dis 1960; 12:639-653Crossref, Medline, Google Scholar
13. Halliday G, Banerjee S, Philpot M, Macdonald A: Community study of people who live in squalor. Lancet 2000; 355:882-886Crossref, Medline, Google Scholar
14. Lachs M, Williams C, O’Brien S, Hurst L, Horwitz R: Older adults: an 11-year longitudinal study of adult protective service use. Arch Intern Med 1996; 156:449-453Crossref, Medline, Google Scholar
15. Cornoni-Huntley J, Brock DB, Ostfeld AM, Taylor JO, Wallace BP (eds): Established Populations for Epidemiologic Studies of the Elderly: NIH Publication 86-2443. Bethesda, Md, US Department of Health and Human Services, National Institutes of Health, 1986Google Scholar
16. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385-401Crossref, Google Scholar
17. Pfeiffer E: A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975; 23:433-441Crossref, Medline, Google Scholar
18. Albert MS, Smith LA, Scherr PA, Taylor JO, Evans DA, Funkenstein HH: Use of brief cognitive tests to identify individuals in the community with Alzheimer’s disease. Int J Neurosci 1991; 57:167-178Crossref, Medline, Google Scholar
19. Cupples LA, D’Agostino RB, Anderson KI, Kannel WB: Comparison of baseline and repeated measure covariate techniques in the Framingham Heart Study. Stat Med 1998; 7:205-218Crossref, Google Scholar
20. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, John Wiley & Sons, 1989, pp 238-245Google Scholar
21. Shah BV, Barnwell BG, Beiler GS: SUDAAN User’s Manual, Release 7.0. Research Triangle Park, NC, Research Triangle Institute, 1996Google Scholar
22. Binder DA: On the variance of asymptotically normal estimators for complex surveys. Int Statistical Rev 1983; 51:279-292Crossref, Google Scholar
23. Katon W, Schulberg HC: Epidemiology of depression in primary care. Gen Hospital Psychiatry 1992; 12:237-242Crossref, Google Scholar



