Effectiveness of Partial Hospitalization in the Treatment of Borderline Personality Disorder: A Randomized Controlled Trial
Abstract
OBJECTIVE: This study compared the effectiveness of psychoanalytically oriented partial hospitalization with standard psychiatric care for patients with borderline personality disorder. METHOD: Thirty-eight patients with borderline personality disorder, diagnosed according to standardized criteria, were allocated either to a partially hospitalized group or to a standard psychiatric care (control) group in a randomized controlled design. Treatment, which included individual and group psychoanalytic psychotherapy, was for a maximum of 18 months. Outcome measures included the frequency of suicide attempts and acts of self-harm, the number and duration of inpatient admissions, the use of psychotropic medication, and self-report measures of depression, anxiety, general symptom distress, interpersonal function, and social adjustment. Data analysis used repeated measures analysis of covariance and nonparametric tests of trend. RESULTS: Patients who were partially hospitalized showed a statistically significant decrease on all measures in contrast to the control group, which showed limited change or deterioration over the same period. An improvement in depressive symptoms, a decrease in suicidal and self-mutilatory acts, reduced inpatient days, and better social and interpersonal function began at 6 months and continued until the end of treatment at 18 months. CONCLUSIONS: Psychoanalytically oriented partial hospitalization is superior to standard psychiatric care for patients with borderline personality disorder. Replication is needed with larger groups, but these results suggest that partial hospitalization may offer an alternative to inpatient treatment.
Most patients with borderline personality disorder are treated with nonspecialist standard psychiatric services by using inpatient treatment, partial hospitalization, and outpatient services as necessary. However, more specific psychological interventions have been developed. These include individual psychoanalytic psychotherapy (1, 2), dialectical behavior therapy (3), group psychotherapy (4), family therapy (5), and supportive psychotherapy (6). While a number of naturalistic outcome studies have been done, particularly of inpatient treatment, randomized controlled trials of outpatient treatment and partial hospitalization are rare (7, 8).
In one of the few controlled studies of intensive outpatient treatment of individuals with borderline personality disorder, Linehan and colleagues (3) showed that dialectical behavior therapy was partially effective. Dialectical behavior therapy (9) is a treatment incorporating cognitive, behavioral, and supportive psychotherapies. Skilled practitioners in an intensive outpatient program use a combination of individual and group approaches centered on a patient-therapist relationship. Treatment with dialectical behavior therapy for 1 year compared with standard treatment led to a reduction in the number and severity of suicide attempts and decreased the frequency and length of inpatient admissions. However, there were no between-group differences on measures of depression, hopelessness, or reasons for living and, although patients receiving dialectical behavior therapy continued to show less parasuicidal behavior at the 6-month follow-up examination, there was no difference in measures of self-destructive acts between groups at the 1-year follow-up (10).
Using a randomized design of treatment versus control (delayed treatment), Piper and colleagues (11) found significant treatment effects after 18 weeks of psychodynamically group-oriented partial hospitalization for patients with both affective disorder and long-standing personality disorder, many of whom were borderline. Interpersonal functioning, illness symptoms, self-esteem, life satisfaction, and defensive functioning all improved after 4 months’ treatment when compared with the control group, and gains were maintained at the 8-month follow-up.
Although they differed both in approach and in the context of treatment, both controlled studies showed promising results, having in common a well-structured program. We developed a psychoanalytically oriented intervention specifically targeting cases of severe borderline personality disorder that integrated individual and group psychoanalytic psychotherapy within a limit-setting, structured, flexible, consistent, and reliable partial hospitalization program. The aims of this program reflected both the therapeutic and management difficulties of the patient with borderline personality disorder, with an emphasis on the relational aspects of the disorder. These aims were as follows: 1) to engage the patient in treatment; 2) to reduce general psychiatric symptoms, particularly depression and anxiety; 3) to decrease the number of self-destructive acts and suicide attempts; 4) to improve social and interpersonal function; and 5) to prevent reliance on prolonged hospital stays.
In a randomized controlled trial, we compared psychoanalytically oriented partial hospitalization with standard psychiatric care in terms of effectiveness. This report is of the first 18 months of the trial. Patients are being followed up in twice-weekly outpatient group psychotherapy, and data on the follow-up will be reported at a later stage.
METHOD
This study was conducted at the Halliwick Psychotherapy Unit, which forms part of the general psychiatric services of an inner-city population of 300,000. Patients could not receive psychiatric or medical treatment elsewhere in order to ensure accurate collection of data.
Halliwick Psychotherapy Unit offers partial hospitalization consisting of long-term psychoanalytically oriented treatment to 30 patients between the ages of 16 and 65 years who suffer from borderline or severe personality disorder. Patients may stay in the program for 18 months.
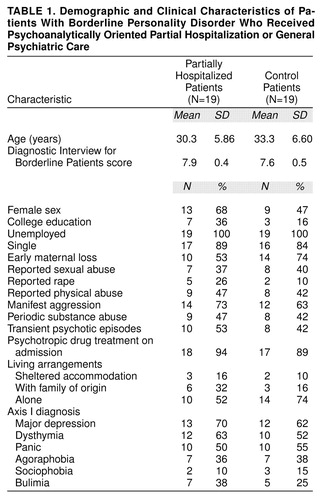
In the present study, we randomly assigned patients either to treatment by means of partial hospitalization or to general psychiatric services (control group). All patients referred during 1993 and 1994 were assessed by using standardized criteria for borderline personality disorder, namely, the Structured Clinical Interview for DSM-III-R (SCID) (12) and the Diagnostic Interview for Borderline Patients (13). A cutoff score of 7 or more was used to determine a formal diagnosis of borderline personality disorder. If patients met both sets of criteria for borderline personality disorder, they were selected for random assignment either to treatment by means of partial hospitalization or to standard outpatient psychiatric treatment. Patients were excluded from the study if they also met DSM-III-R criteria (based on the SCID) for schizophrenia, bipolar disorder, substance misuse, or mental impairment or had evidence of organic brain disorder. Institutional review board approval required that patients were able to cross over into the partially hospitalized group if the psychiatrist in charge thought it necessary. Sixty referred patients met the criteria for inclusion in the study. After complete description of the study to the subjects, written informed consent was obtained, a full clinical history was taken, and demographic information was recorded. Ten patients refused to participate in the random assignment. Six of these patients were admitted to the partial hospitalization program and excluded from the present study, and four declined further treatment of any type. Six other patients did not wish to participate in regular self-assessment and therefore were not included. There were no significant differences on any of the baseline measures for these patients compared with those who entered the study. This left 44 patients in the study, who were randomly assigned to the two groups. Within the first month of the study, three patients in the control group crossed over into the partially hospitalized group after serious suicide attempts leading to inpatient medical and psychiatric treatment. Three patients (12%) in the partially hospitalized group dropped out of treatment within 6 months. All were available for follow-up, but crossover and dropout patients were not included in the formal statistical analysis, leaving 19 subjects in each of the partially hospitalized and control groups. No subjects dropped out of the control group. Demographic and clinical characteristics of the cohort of patients are shown in Table 1. After random assignment, there were no significant differences on any variable between the two groups, including frequencies or average number of axis I and axis II disorders. Particularly notable was the association of mood and anxiety disorders with borderline personality disorder.
Treatment for the partially hospitalized group consisted of 1) once-weekly individual psychoanalytic psychotherapy, 2) thrice-weekly group analytic psychotherapy (1 hour each), 3) once-a-week expressive therapy oriented toward psychodrama techniques (1 hour), and 4) a weekly community meeting (1 hour), all spread over 5 days. In addition, on a once-per-month basis, subjects had 5) a meeting with the case administrator (1 hour) and 6) medication review by the resident psychiatrist (A.B.). Therapies and informal patient-staff contact were organized in accordance with the psychoanalytic model of borderline personality disorder as a disorder of attachment, separation tolerance, and mentalization (the capacity to think about oneself in relation to others and to understand others’ state of mind) (14). Medication consisted of antidepressant and antipsychotic drugs prescribed as appropriate; polypharmacy was discouraged. The average length of stay was 1.45 years, and attendance at the program’s psychotherapy sessions was 62%.
All therapy was given by psychiatrically trained nurses who were members of the partial hospitalization program’s team but who had no formal psychotherapy qualifications. Adherence to therapy was monitored through supervision (twice per week with the whole team), by using verbatim session reports, and by completion of a monitoring form collecting information about the activities and interventions of therapists. Other aspects of the partial hospitalization program have been described elsewhere (15, 16).
We chose standard treatment in the general psychiatric services as our control condition. This consisted of 1) regular psychiatric review with a senior psychiatrist when necessary (on average, twice per month); 2) inpatient admission as appropriate (admission rate=90%, average stay=11.6 days), with discharge to nonpsychoanalytic psychiatric partial hospitalization focusing on problem solving (72% were partially hospitalized, with an average length of stay of 6 months); followed by 3) outpatient and community follow-up (100%, every-2-week visits by a community psychiatric nurse) as standard aftercare. Members of the control group received no formal psychotherapy. The initial types and doses of medication were the same for both groups. Although the control group was not considered to have received the same amount of professional attention as the partially hospitalized group, this approach controlled for spontaneous remission.
Measures of Outcome
Acts of self-harm and clinical measures. Suicidal acts were defined as having the following characteristics: 1) deliberate, 2) life-threatening, 3) resulted in medical intervention, and 4) medical assessment consistent with a suicide attempt. Criteria for acts of self-mutilation were as follows: 1) deliberate, 2) resulted in visible tissue damage, and 3) nursing or medical intervention required.
A semistructured interview (the Suicide and Self-Harm Inventory, available by request from Dr. Bateman, was used to obtain details of both suicidal and self-mutilating acts for the 6-month period before patients entered the study. This interview asks specific questions not only about the numbers of acts but also about the dangerousness of acts—i.e., the presence or absence of another person, the likelihood of being found, preparation for the act, and lethality of the act. Multiple acts over a short period of time—for example, a frenzied self-cutting—were counted as a single act. Partially hospitalized patients were monitored carefully with regard to self-destructive acts, and patients in the control group were interviewed every 6 months regarding self-mutilation and suicide attempts. Self-reports of suicidal and self-mutilatory acts were cross-checked with medical and psychiatric records.
For all patients, a search of the hospital inpatient database was made to obtain the number of hospital admissions and the lengths of stay during a period of 6 months before entry into the study. The results were cross-checked with medical records. All patients were admitted to the local hospital’s psychiatric unit. Hospital admission, length of stay, and participation in the partial hospitalization program’s psychotherapy sessions were monitored throughout the study for all patients.
Psychiatric symptoms. The patients’ subjective experience of symptoms was measured by using the SCL-90-R (17). Depression and anxiety symptoms were measured by using the Beck Depression Inventory (18) and the Spielberger State-Trait Anxiety Inventory (19), respectively. To assess areas targeted by psychoanalytic therapy, social adjustment and interpersonal function were measured pre- and posttrial by using the modified Social Adjustment Scale—self-report (20) and the Inventory of Interpersonal Problems—circumflex version (21, 22). The Social Adjustment Scale—self-report and Inventory of Interpersonal Problems—circumflex version provide an assessment of an individual’s work, leisure activities, and family life and difficulties with interpersonal function. The reliability and validity of all of these instruments is well established.
Monitoring of symptoms during treatment was with self-rating questionnaires at 3-month intervals on all symptom measures except the SCL-90-R, which was given at 6-month intervals.
Statistical Analysis
All analyses were carried out by using the Statistical Package for the Social Sciences for Windows (version 7). The statistical approach adopted for the analyses of the symptom data was repeated measures analysis of covariance (ANCOVA) (SPSS General Linear Models module). The baseline measure of each variable was used as a covariate, and the group-by-time interaction provided the measure of the significance of treatment effect on most measures. When an interaction was significant, Newman-Keuls post hoc tests were used to test differences between groups at a particular time point. In order to examine differences in trends between the two groups, the treatment group-by-time interactions were decomposed, and linear and quadratic polynomial components were also tested. In all repeated measures ANCOVAs, the p values for Greenhouse-Geisser corrected degrees of freedom are reported. When assumptions of univariate analysis of variance were not met (either in terms of the sphericity test or the test of equality of error variances), a more conservative multivariate solution to the repeated measures problem was adopted. After the application of the general linear model, diagnostic plots of standardized residuals against predicted values were examined in order to confirm that the assumptions of the model were met. The same statistical analyses were performed, including the three crossover and three dropout subjects, leading to an identical pattern of findings.
The distributional properties of the clinical measures did not permit the application of ANCOVAs. Here the trend for change was tested separately for each group by using a nonparametric test of trend (Kendall’s W). In addition, differences between the two groups could be examined at the end of treatment by using Mann-Whitney U tests.
RESULTS
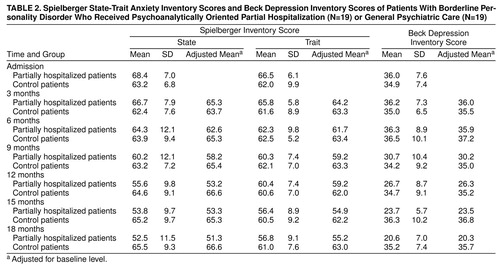
Means and standard deviations for the dependent variables are displayed in Table 2 and Table 3. The tables include scores adjusted for initial values of variables where the two groups were significantly different at intake.
Acts of Self-Harm and Clinical Measures
The number of incidents of self-mutilating behavior decreased over the course of treatment in the partially hospitalized group but remained constant in the control group (Figure 1). In the partially hospitalized group, the median number of self-mutilations per 6-month period was reduced from 9 to 1, whereas in the control group over the same time period, the change was from 8 to 6. The trend test was highly significant for the partially hospitalized group (Kendall’s W=0.21, χ2=11.9, df=3, p<0.008) but not significant for the control group (Kendall’s W=0.05, χ2=2.4, df=3, n.s.). Group differences in the number of attempts at self-mutilation emerged by 12 months, and the number of individuals no longer self-mutilating was significantly greater by 18 months in the partially hospitalized group than in the control group (χ2=7.0, df=1, p<0.008).
Individuals were interviewed and coded every 6 months for the presence or absence of suicide attempts. Figure 1 shows the proportion of each group with reported suicide attempts in the previous 6 months, on admission, at 6 months, at 12 months, and at 18 months. In the partially hospitalized group, there was a clear reduction from 94.7% on admission (mean=1.68) to 5.3% (mean=0.16) at 18 months. This trend was highly significant (Kendall’s W=0.59, χ2=33.5, df=3, p<0.001). The same test revealed no significant trend for the control group (Kendall’s W=0.04, χ2=2.4, df=3, n.s.). Group differences emerged by 6 months. The number of individuals who were no longer parasuicidal was significantly greater in the partially hospitalized group than in the control group by 12 months (χ2=4.3, df=1, p<0.05).
Changes in inpatient treatment showed a somewhat more complicated pattern. The average length of hospitalization, adjusted for preadmission values, is displayed in Figure 2. This confirms that the average length of hospitalization in the control group in the last 6 months of the study increased dramatically, whereas in the partially hospitalized group, it remained relatively stable at around 4 days per 6 months. The group-by-time interaction was significant (F=7.7, df=1, 35, p<0.01), with a highly significant quadratic component (F=13.3, df=1, 35, p<0.001). The post hoc tests yielded significant differences at 6 months (t=7.66, df=36, p<0.001) and 18 months (t=13.23, df=36, p<0.001). An identical pattern emerged for the number of inpatient episodes (F=14.1, df=1, 35, p<0.001, and F=19.9, df=1, 35, p<0.001, for the two-way and quadratic components of the interaction, respectively).
The need for medication was reduced in both groups. In the control group, of those who were taking medication at the start of the study, 78% were still taking medication compared to only 38% of those in the partially hospitalized group at the end of the trial (corrected χ2=4.8, df=1, p<0.03).
Self-Report Measures
Two measures of anxiety (state and trait scales from the Spielberger State-Trait Anxiety Inventory) were obtained from participants (Table 2). Both self-reported state and trait anxiety scores decreased substantially in the partially hospitalized group but remained unchanged in the control group. The time-by-group interaction was significant (F=9.2, df=1, 33, p<0.005, and Wilks’s lambda=0.62, F=3.6, df=5, 29, p<0.02, for state and trait scores, respectively). The polynomial decomposition of the interactions revealed significant differences in the linear component of both interactions (F=32.9, df=1, 33, p<0.001, and F=15.1, df=1, 33, p<0.001, for state and trait scores, respectively), confirming that the slopes were significantly different for the two groups. Post hoc analysis indicated that the two groups began to report significantly different levels of state and trait anxiety measures from 9 months (t=4.69, df=36, p<0.001, and t=3.64, df=36, p<0.001, respectively).
Beck Depression Inventory scores also significantly decreased in the partially hospitalized group (Table 2). The group-by-time interaction was significant (F=13.1, df=1, 33, p<0.001); the change was significant after 9 months (t=4.06, df=36, p<0.001) and continued throughout treatment. The linear trend was significantly greater for the partially hospitalized group than the control group (F=58.3, df=1, 33, p<0.001).
On the global severity index scale of the SCL-90-R, the group-by-time interaction was significant (Wilks’s lambda=0.81, F=3.5, df=2, 31, p<0.05). The differences in scores were marked at 1 year and significant at 18 months (t=3.40, df=36, p<0.005) (Table 3). By contrast, the interaction between group and time on the positive symptom total score was not significant (F=3.0, df=1, 32, n.s.). This indicates that it was the severity of symptom reports rather than the number of symptoms reported that decreased in the partially hospitalized group.
The total Social Adjustment Scale—self-report score was significantly lower for the partially hospitalized group (mean=2.8) than the control group (mean=3.3) at the end of the study when adjusted for initial values. The ANCOVA was highly significant (F=8.7, df=1, 33, p<0.006). The mean total scores on the Inventory of Interpersonal Problems—circumflex version were 2.38 (SD=0.33) and 2.31 (SD=0.32) for the partially hospitalized and control groups, respectively, on admission. Whereas the scores decreased for the experimental group during treatment to 1.86 (SD=0.36), they increased slightly for the control group to 2.60 (SD=0.29). This difference was again highly significant (F=63.7, df=1, 34, p<0.001).
To examine predictors of improvement in the partially hospitalized group, suicide attempts and self-mutilation were combined into a single variable—self-harm—scored as a simple binary variable (present/absent). Nonparametric correlation coefficients were computed between the presence of self-harm and demographic, clinical, and outcome variables for the partially hospitalized group. For the 19 subjects, no admission variable predicted outcome.
DISCUSSION
Nineteen patients with borderline personality disorder were treated with psychoanalytically oriented partial hospitalization and compared with 19 patients treated with standard psychiatric care. The overall aims of this program were achieved. Patients treated with partial hospitalization for 18 months showed significant improvement on both symptomatic and clinical measures. Treatment was effective for both men and women. No patients committed suicide. Improvement in psychiatric symptoms and suicidal acts occurred after 6 months, but a reduction in the frequency of hospital admissions and the length of inpatient stays was only clear in the last 6 months, indicating a need for longer-term treatment. Shorter hospital stays for the partially hospitalized group were not a result of there being a program to which patients could return. All inpatients within the psychiatric services were routinely discharged to psychiatric partial hospitalization for a variable length of time, as agreed on between patient and psychiatrist.
The patients in this study represented a group of individuals with severe borderline personality disorder who frequently harmed themselves and attempted suicide, while exhibiting severe levels of depression, suffering from high levels of symptomatic distress, and demonstrating comorbidity for affective disorders. In contrast to the study reported by Linehan and colleagues (3), which included only women, improvement was observed in depressive symptoms. In both studies, patients continued to suffer pathological levels of symptoms at the end of treatment. Improvement of depression in the partially hospitalized subjects may have been a result of antidepressant medication (23). However, this explanation seems unlikely, since control subjects received therapeutic doses of medication for longer times, and symptomatic change occurred later than would have been expected with antidepressants.
This study was not specifically looking at cost-effectiveness; we do not have data on exact cost differences between the two treatments. The results suggest that offering a less structured and less intensive program than partial hospitalization is inadequate treatment and fails to reduce the medical risk of suicide, diminish symptoms, or ultimately decrease the numbers and durations of hospital stays. This study provides support for initiating a full cost-benefit analysis of partial hospitalization and inpatient approaches to treating borderline personality disorder.
There are a number of limitations to the conclusions that may be drawn from the study. In particular, we did not use the minimization method of random assignment, although no significant differences on baseline variables were found between the two groups. Follow-up data are not yet available. The numbers are small, perhaps accounting for the absence of predictors of outcome, and the results need replication with larger groups to determine their generalizability. Although three dropout and three crossover patients were excluded from the present analysis, the effect size for the treatment group remained unchanged when they were included. Because no resources were available for the ongoing monitoring of treatment, it remains unclear what the therapeutic factors are beyond the use of a highly structured program for the treatment of personality disorder. The large amount of staff time received by the partially hospitalized patients may be responsible for their improvement, but the control group received large amounts of staff attention through hospital admission, nonpsychoanalytic partial hospitalization, and extensive outpatient support. However, this treatment of the control group lacked coherence, was inconsistently applied, particularly at times of crisis, and was delivered by a number of uncoordinated agencies.
Only three patients (12%) dropped out of the program and could not be reengaged. This is less than the dropout rate found in some inpatient and outpatient psychoanalytic treatments for borderline personality disorder (24, 25) but similar to the 16% dropout rate found in one study involving dialectical behavior therapy (3). There are a number of possible features of psychoanalytic partial hospitalization that account for patients staying in treatment and benefiting from it. First, those who miss therapy sessions are actively pursued by phone, letter, and home visit, if necessary. Second, factors leading to nonattendance are targeted within individual therapy, and the reasons in terms of the patient’s current emotional state are discussed. Third, the structured nature of the program ensures that patients are constantly made aware of when and where to bring problems. Contact outside of the program was limited to prompting attendance at the next group meeting. In contrast to practices in other psychoanalytic and behavioral programs, no formal contract was made, since, in our view, patients with borderline personality disorder frequently sabotage treatment. Discharge because of failure to meet attendance requirements is likely to traumatically recreate the abandonment the borderline patient both is desperate to avoid and simultaneously provokes. Finally, treatment with partial hospitalization simultaneously balances support and treatment with individual responsibility. The program is neither too much nor too little.
We believe that a multicomponent program is necessary for treatment and that its critical feature is the way in which its components are brought together. It is our view that the essential features of an effective program for treating borderline personality disorder are the following: 1) a theoretically coherent treatment approach, 2) a relationship focus, and 3) consistent application over a period of time. This permits exploration of inconsistencies in the relationship patterns of patients with borderline personality disorder and identification of unconscious factors that interfere with the possibility of change. Partial hospitalization seems a promising, possibly cheaper, alternative to both specialist inpatient and general psychiatric treatment. Whether it is better than intensive outpatient treatment by specialists for severe borderline personality disorder remains to be seen.
Received June 16, 1998; revisions received Nov. 12, 1998, and March 5, 1999; accepted March 17, 1999. From the Halliwick Day Unit, St. Ann’s Hospital. Address reprint requests to Dr. Bateman, Consultant Psychiatrist in Psychotherapy, Haringey Healthcare NHS Trust, Halliwick Day Unit, St. Ann’s Hospital, St. Ann’s Road, London N15 3TH; [email protected] (e-mail). The authors thank Dr. Ilan Diamant for conducting research interviews and the day hospital staff for patient care.
 |
 |
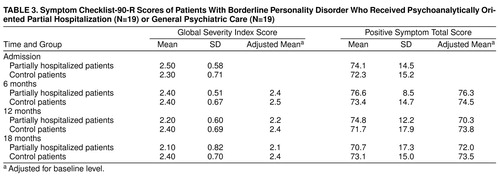 |
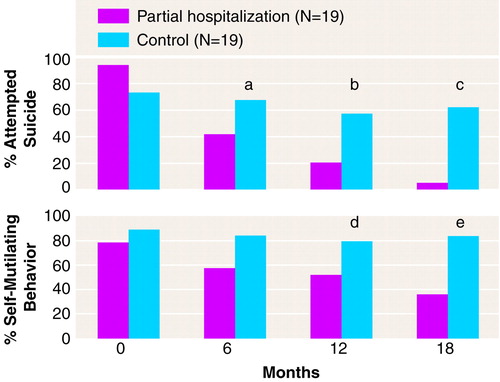
FIGURE 1. Percentage of Patients With Borderline Personality Disorder Who Received Psychoanalytically Oriented Partial Hospitalization or General Psychiatric Care Who Attempted Suicide or Exhibited Self-Mutilating Behavior During 6-Month Periodsa
aSignificant group differences (Mann-Whitney U=119, p<0.05).
bSignificant group differences (Mann-Whitney U=114, p<0.03)
cSignificant group differences (Mann-Whitney U=75, p<0.001).
dSignificant group differences (Mann-Whitney U=110, p<0.04).
eSignificant group differences (Mann-Whitney U=62, p<0.001).
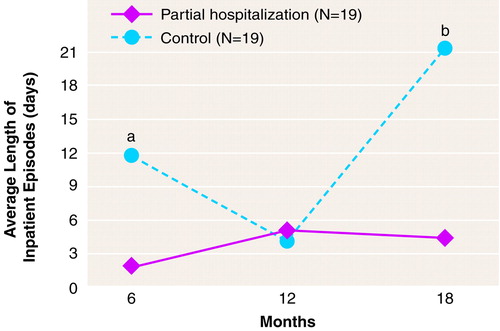
FIGURE 2. Mean Duration of Inpatient Episodes for Patients With Borderline Personality Disorder Who Received Psychoanalytically Oriented Partial Hospitalization or General Psychiatric Care During 6-Month Periods, Adjusted for Pretreatment Levels
aSignificant group differences (t=7.66, df=36, p<0.001, post hoc tests).
bSignificant group differences (t=13.23, df=36, p<0.001, post hoc tests).
1. Kernberg OF, Selzer MA, Koenigsberg HW, Carr AC, Appelbaum AH: Psychodynamic Psychotherapy of Borderline Patients. New York, Basic Books, 1989Google Scholar
2. Waldinger RJ: Intensive psychodynamic therapy with borderline patients: an overview. Am J Psychiatry 1987; 144:267–274Link, Google Scholar
3. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard H: Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry 1991; 48:1060–1064Google Scholar
4. Munroe-Blum H, Marziali E: Time-limited group psychotherapy for borderline patients. Can J Psychiatry 1988; 33:364–369Crossref, Medline, Google Scholar
5. Gunderson JG, Berkowitz C, Ruiz-Sancho A: Families of borderline patients: a psychoeducational approach. Bull Menninger Clin 1997; 61:446–457Medline, Google Scholar
6. Waldinger RJ, Gunderson JG: Effective Psychotherapy With Borderline Patients. Washington, DC, American Psychiatric Press, 1989Google Scholar
7. Sanislow CA, McGlashan TH: Treatment outcome of personality disorders. Can J Psychiatry 1998; 43:237–250Crossref, Medline, Google Scholar
8. Bateman AW, Fonagy P: Effectiveness of psychotherapeutic treatment of personality disorder. Br J Psychiatry (in press)Google Scholar
9. Linehan MM: Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, Guilford Press, 1993Google Scholar
10. Linehan MM, Heard HL, Armstrong HE: Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry 1993; 50:971–974Crossref, Medline, Google Scholar
11. Piper WE, Rosie JS, Azim HFA, Joyce AS: A randomized trial of psychiatric day treatment for patients with affective and personality disorders. Hosp Community Psychiatry 1993; 44:757–763Abstract, Google Scholar
12. Spitzer RL, Williams JBW, Gibbon M, First MB: User’s Guide for the Structured Clinical Interview for DSM-III-R (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
13. Gunderson JG, Kolb JE, Austin V: The Diagnostic Interview for Borderline Patients. Am J Psychiatry 1981; 138:896–903Link, Google Scholar
14. Fonagy P: An attachment theory approach to treatment of the difficult patient. Bull Menninger Clin 1998; 62:147–169Medline, Google Scholar
15. Bateman A: The treatment of borderline patients in a day hospital setting. Psychoanal Psychother 1995; 91:3–16Crossref, Google Scholar
16. Bateman A: Borderline personality disorder and psychotherapeutic psychiatry: an integrative approach. Br J Psychother 1997; 13:489–498Crossref, Google Scholar
17. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
18. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
19. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
20. Cooper P, Osborn M, Gath D, Feggetter G: Evaluation of a modified self-report measure of social adjustment. Br J Psychiatry 1982; 141:68–75Crossref, Medline, Google Scholar
21. Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS: Inventory of Interpersonal Problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892Crossref, Medline, Google Scholar
22. Alden LE, Wiggins JS, Pincus AL: Construction of circumflex scales for the Inventory of Interpersonal Problems. J Pers Assess 1990; 55:521–536Crossref, Medline, Google Scholar
23. Soloff PH: Algorithms for psychopharmacological treatment of personality dimensions: symptom-specific treatments for cognitive-perceptual, affective, and impulsive-behavioral dysregulation. Bull Menninger Clin 1998; 62:195–214Medline, Google Scholar
24. Waldinger RJ, Gunderson JG: Completed therapies with borderline patients. Am J Psychother 1984; 38:190–202Crossref, Medline, Google Scholar
25. Gunderson JG, Frank AF, Ronningstam EF, Wachter S, Lynch VJ, Wolf PJ: Early discontinuance of borderline patients from psychotherapy. J Nerv Ment Dis 1989; 177:38–42Crossref, Medline, Google Scholar



