Panic and Phobic Anxiety: Defining Phenotypes for Genetic Studies
Abstract
Objective: With recent advances in molecular genetics, the rate-limiting step in identifying susceptibility genes for psychiatric disorders has become phenotype definition. The success of psychiatric genetics may require the development of a “genetic nosology” that can classify individuals in terms of the heritable aspects of psychopathology. The authors" aim is to begin to apply this analysis to the anxiety disorders, focusing on panic and phobic disorders. Method: Two parallel traditions of defining anxiety phenotypes are reviewed: the first, more closely identified with clinical psychiatry, has identified categorical diagnoses (e.g., panic disorder and social phobia). The other, more closely identified with psychological studies of personality development, has examined dimensional traits (e.g., neuroticism) and anxious temperament (e.g., behavioral inhibition). Results: The authors suggest that a genetic nosology of panic and phobic disorders may incorporate features of both traditions and discuss strategies for optimizing genetic approaches to anxiety including 1) studying phenotypic extremes, 2) identifying biological trait markers, and 3) using animal models to identify candidate loci. Conclusions: An important dividend from the effort to define the boundaries of heritable phenotypes for genetic studies of anxiety may be a refinement of the nosology of anxiety disorders. Am J Psychiatry 1998; 155: 1152-1162
The part played by heredity in the development of the psychoneuroses is one of the fundamental unsolved problems in psychiatry . . . . But the chief difficulty is to define the condition the heredity of which one is attempting to trace.
Psychiatric genetics has emerged as an exciting frontier that holds the promise of revealing the molecular basis of neuropsychiatry. An early success story has been the identification of at least four specific genes involved in Alzheimer’s disease (2). Gene mapping studies have identified chromosomal regions linked to several other disorders, particularly bipolar disorder and schizophrenia, although some of these findings have eluded replication. Molecular genetic studies of anxiety disorders, however, have not yet had similar success. In part, this may be attributed to obstacles that complicate efforts to identify genes for any complex disorder: non-Mendelian inheritance patterns and the possibility of phenocopies, genetic heterogeneity, incomplete penetrance, and variable expressivity (3). However, an even more formidable obstacle to identifying genes influencing anxiety is the problem of defining the heritable phenotype (4). For the most part, gene mapping proceeds by demonstrating that a genetic marker (whose chromosomal location is known) is co-inherited with the phenotype of interest. Without an accurate specification of the phenotype, this procedure becomes difficult, if not impossible, to perform. In this sense, the success of psychiatric genetics has everything to do with nosology.
Tsuang and colleagues (4) have pointed out that ambiguities in identifying the phenotype may be the “rate-limiting step” in psychiatric genetic studies. The technology of DNA analysis has progressed to the point that whole-genome scans are feasible. The task of collecting clinical samples has been simplified by the trend toward genetic analyses that require only small nuclear families or even samples of unrelated individuals. But these advances cannot be usefully exploited in the absence of a system for identifying the heritable phenotypes of interest. One of the major tasks of psychiatric genetics, then, will be to construct a “psychiatric genetic nosology” capable of classifying individuals in ways that correspond to distinct genetic entities (4).
Family and twin studies, summarized elsewhere (5)(6), have demonstrated that anxiety disorders can be influenced by genetic factors. Because these investigations have relied on the DSM system to define anxiety disorder phenotypes, they suggest that the standard clinical nosology has been useful for genetic studies: it has described anxiety syndromes that demonstrate familiality and heritability. Nevertheless, preliminary efforts have not yet been able to identify the genetic loci that influence these syndromes.
To be useful, a genetic nosology must address obstacles to accurate classification such as phenocopies, variable expressivity, and incomplete penetrance. Several strategies have been proposed to accomplish this (4). For example, established diagnostic categories can be reorganized to accommodate the variable expression of a disease genotype. Alternatively, new phenotypes can be defined for the explicit purpose of capturing genetically determined components of psychopathology. In constructing a genetic nosology for panic and phobic anxiety, we need to describe anxiety phenotypes so as to maximize the likelihood of identifying genetic factors that influence anxiety disorders.
CATEGORICAL PHENOTYPES: ANXIETY DISORDERS
Historical Context
Although the categorical diagnosis of panic disorder did not appear in the standard nosology until the publication of DSM-III in 1980, similar syndromes had been described much earlier (7)(8). DSM-II, published in 1968, included the categories anxiety neurosis and phobic neurosis, both of which could be accompanied by panic-anxiety. Anxiety neurosis was succinctly defined as “anxious over-concern extending to panic and frequently associated with somatic symptoms”(p. 39). Influenced in large part by the pioneering work of Klein (9) on the “pharmacologic dissection” of anxiety, DSM-III differentiated symptoms of anxiety neurosis into two diagnostic categories: panic disorder and generalized anxiety disorder. A parallel influence was that of Marks and his colleagues (10), who provided evidence for the subdivision of phobic disorders into agoraphobia, social phobia, and simple phobias (called specific phobias in DSM-IV). In DSM-III-R, agoraphobia came to be characterized as a secondary complication of panic and distinct from other phobias. In DSM-IV, agoraphobia, by definition, involves fear of panic attacks or limited symptom panic attacks, so the agoraphobic phenotype can no longer be separated from panic. This view is supported by a substantial body of evidence, but it remains controversial (11). Because panic attacks can occur as part of both panic disorder and phobic disorders, they do not define the boundary between these disorders. The defining features of panic disorder may instead be the recurrence of unexpected panic attacks and the development of anticipatory anxiety about additional attacks (12). As our understanding of anxiety disorders evolves, the boundaries we draw between them are likely to shift again.
Familial Aspects of Panic and Phobic Disorders
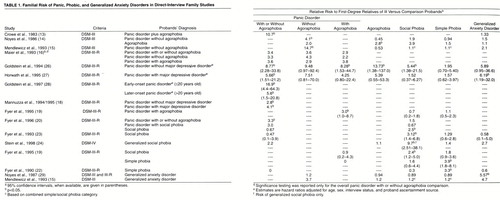
Despite these ambiguities, eight direct-interview family studies of the diagnosis of panic disorder (with or without agoraphobia) have reached the same conclusion: panic disorder is a familial phenotype (13)-(20). First-degree relatives of probands with panic disorder have a three- to 21-fold higher lifetime risk of panic disorder than relatives of unaffected probands. Analyses of pedigrees in several of these family studies have been consistent with the possibility that a single major locus contributes to the inheritance of panic disorder, but polygenic inheritance has not been excluded (13), (21). Fewer family studies of phobic disorders have been reported, but the available evidence suggests that they, too, are familial. Fyer and colleagues (19), (22) found that relatives of probands with simple phobia have a three- to fourfold greater risk of simple phobia than control subjects. Similarly, they found an approximately threefold greater risk of social phobia among relatives of probands with social phobia and no other anxiety disorder (19), (23). A recent family study by Stein and colleagues (24) further demonstrated that relatives of probands with generalized social phobia had a nearly 10-fold greater risk of the generalized type of social phobia but no greater risk of nongeneralized or discrete social phobias.
Besides evaluating whether a disorder aggregates in families, family studies can examine the genetic relationships among comorbid disorders (25). The results summarized in table 1 suggest that panic and phobic disorders tend to “breed true”: relatives are at highest risk for the proband’s disorder. Moreover, the available family studies do not support a familial relationship between simple (specific) phobia and panic disorder or other phobic disorders. Similarly, the DSM-III and DSM-III-R diagnosis of generalized anxiety disorder does not appear to share familial determinants with panic or phobic disorder.
In one of the only direct-interview family studies to examine the comorbidity of panic disorder and agoraphobia, Noyes and colleagues (14) found that relatives of probands with agoraphobia were at increased risk of both agoraphobia and panic disorder, while relatives of panic disorder probands had an increased risk of panic disorder but not agoraphobia. They interpreted the findings as consistent with the hypothesis that agoraphobia represents a more severe variant of panic disorder, but subsequent studies have produced conflicting results (15), (26). The familial relationship between panic disorder and social phobia also remains uncertain. Relatives of probands with social phobia have been reported to have an increased risk of social phobia but not panic disorder (19), (20), (23). However, in one large family study, social phobia did aggregate in the relatives of probands with panic disorder (without comorbid social phobia) (27). Because this association was seen in relatives of probands with and without panic disorder, the authors concluded that the comorbidity of panic and social phobia reflected their common co-occurrence rather than familial transmission of the social phobia.
The relationship between anxiety disorders, particularly panic disorder, and major depression has been another area of controversy. In one study comparing “pure” and comorbid panic disorder and major depression (30), relatives of probands with panic disorder alone were at an elevated risk of major depression without panic disorder. However, several family and twin studies have suggested that major depression is genetically distinguishable from panic and phobic disorders (17), (18), (26), (31)-(33) but may share genetic determinants with generalized anxiety (34).
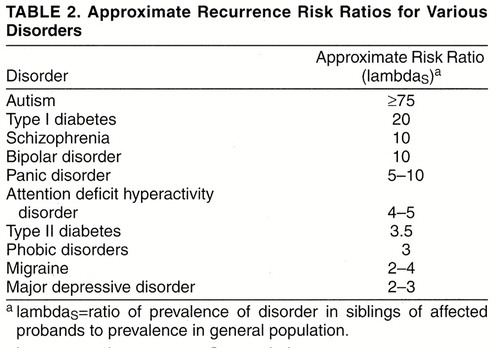
In addition to evaluating the transmission of individual and comorbid anxiety diagnoses, family studies can provide another piece of information that may be crucial for gene-mapping studies. Risch (35) has demonstrated that the power of a commonly used method of linkage analysis—affected-relative-pair analysis—depends on the relative risk (denoted lambdaR) of the disorder among relatives of affected probands compared to that of the general population. This recurrence risk ratio is often computed for siblings (lambdaS), and disorders with a lambdaS greater than 5–10 are much more amenable to gene-mapping studies than are disorders with a lower lambdaS(3). As table 2 shows, lambdaS for panic disorder makes it a suitable target for linkage studies.
Heritability of Panic and Phobic Disorders
Twin and adoption studies help address the question of whether the familial nature of panic and phobic disorders is due to genetic influences. By comparing concordance rates of monozygotic and dizygotic twins, one can estimate the heritability (proportion of phenotypic variance due to genetic factors) of these disorders, although this estimate will vary depending on the population studied. Unfortunately, there have been few studies of categorical anxiety diagnoses, and several of these have had relatively small samples of twins (36)-(39).
The largest and most informative twin study of anxiety disorders to date has been Kendler and colleagues’ study of a population-based sample of 1,033 female twin pairs from the Virginia Twin Registry (33), (40)-(43). This study has provided estimates of the heritability of DSM-III-R panic disorder (44%), agoraphobia (39%), generalized anxiety disorder (32%), animal phobias (32%), and social phobia (30%) that suggest a genetic influence on the expression of these phenotypes, although environmental factors play a large role. In contrast, situational phobias seemed to have little or no genetic component. In a subset of this sample (44), blood-injury phobias resembled situational phobias in having greater evidence for environmental than genetic etiology, although familial aggregation of blood-injury fears appeared to be due mainly to additive genetic factors.
The Virginia twin studies have also allowed Kendler and colleagues to investigate the genetic relationships among anxiety disorders. For example, they found support for the division of anxiety neurosis into panic disorder and generalized anxiety disorder in that genetic influences on the two disorders appeared to differ (43). In fact, generalized anxiety disorder and major depression appeared to reflect one common genetic factor, while panic disorder and phobias appeared to be influenced by another distinct factor. Among the phobias, agoraphobia appeared to have the highest heritability, although Kendler et al. found evidence for an inherited “phobia proneness” underlying agoraphobia, social phobia, and animal phobias (40). Agoraphobia had the lowest loading on this common genetic factor, suggesting that it may be genetically distinguishable from other phobic subtypes.
Implications for a Genetic Nosology
Family and twin studies suggest that panic disorder, as defined in DSM-III and its successors, is a familial phenotype and that genetic factors may explain more than 40% of the phenotypic variance. Phobic disorders exhibit similar, although less robust, familial aggregation and heritability. The Virginia Twin Registry studies raise the possibility that panic disorder and phobias reflect a shared genetic diathesis. However, the weight of the evidence indicates that genes influencing specific phobias, generalized anxiety disorder, and major depression are largely distinct from those influencing panic disorder and agoraphobia.
For the purposes of gene mapping studies, relying solely on categorical phenotypes may have important limitations. The formation of diagnostic categories requires that boundaries be drawn, and because the DSM categories are based on consensus definitions, there is a degree of arbitrariness built into them. This complicates efforts to classify individuals as “affected” or “unaffected” for the purpose of genetic studies. For example, how should we classify the individual who meets all criteria for panic disorder except that none of her recurrent panic attacks has more than three symptoms? Strictly speaking, this individual would not qualify for a DSM diagnosis of panic disorder—but can we confidently call her unaffected?
Psychiatric nosology has evolved from a complex mixture of clinical observation, empirical research, historical tradition, and even political considerations. Because DSM-III and its successors have aimed to be atheoretical and descriptive, their categories are not based on pathogenetic mechanisms. It would be surprising if they described just those aspects of psychopathology which are under genetic influence. The argument can be made that for the purposes of identifying susceptibility genes, the practice of condensing phenotypic data into dichotomous or categorical diagnoses results in a loss of information (45). In recognition of this, several investigators have found that familial/genetic aspects of anxiety disorders are more apparent when the definition of the affected state is expanded beyond the strict diagnostic criteria to include subsyndromal variants; most family, twin, and linkage studies of panic disorder have included subsyndromal definitions of caseness (13), (14), (17), (42).
One way to assess the value of broadening the “affected” category is to examine the heritability of subsyndromal anxiety symptoms. Here, again, results have been mixed. In several studies using questionnaire measures of phobic fears, heritability estimates have been in the range of 0.45 to 0.55 (46)-(49), somewhat higher than the heritability of clinically diagnosed phobic disorders estimated by Kendler and colleagues. On the other hand, some family and twin studies have not found that subsyndromal panic and phobic symptoms are highly transmissible (22), (23), (50). In their studies of phobic disorders, Fyer and colleagues (22), (23) found no evidence of familial transmission of irrational simple or social fears, and in a large twin-family study of volunteer and population-based twin samples, Kendler and colleagues (51) found only modest heritability of panic-phobic symptoms on the basis of responses to an anxiety questionnaire.
Broadening the definition of affected status may reduce the risk of false negative misclassification, but it could correspondingly increase the risk of false positive misclassification, which is the greater threat to linkage studies. A different approach to minimizing the arbitrariness of categorical diagnoses is to view anxiety phenotypes as traits or dimensions.
DIMENSIONAL PHENOTYPES: TRAIT ANXIETY AND ANXIOUS TEMPERAMENT
Studies of the psychology of personality and individual differences have suggested that there may be a small number of underlying dimensions along which individuals vary in ways that predict both normal behavior and pathologic states. According to this view, psychopathology represents extremes of dimensions that underlie normal personality (52) Several dimensional or temperamental constructs have been proposed to account for individual differences in personality and emotional experience, many of them directly related to anxiety, including neuroticism, introversion, behavioral inhibition, and harm avoidance (53)-(55). To illustrate the relevance of such dimensions to a genetic nosology of anxiety, we will discuss two examples.
Neuroticism
According to Eysenck (55) and others, pathological extremes of neuroticism are the basis of the neuroses, including anxiety neuroses. Neuroticism was said to be related to the “inherent lability of the autonomic nervous system” (55), p.4). Individuals high in neuroticism were described as anxious, worried, and frequently depressed. The frequent comorbidity of anxious and depressive symptoms in clinical settings has led some to propose that there is more evidence for a “general neurotic syndrome” than for the distinct anxiety and depressive disorders described in the DSM system (56).
A large body of studies have indicated that neuroticism is under substantial genetic control with a heritability of about 50% (57)-(59). Studies of a large sample of Australian twin pairs have supported the notion that anxiety disorders and depression are variable expressions of a heritable tendency toward neuroticism (37), (60)-(63). In a study of 2903 Australian twin pairs, Martin and colleagues (62) found evidence that genetic determinants of neuroticism overlapped with those of panic-anxiety among male but not female subjects. A subsequent study extended these findings by obtaining structured clinical interviews and DSM-III diagnoses for 462 twin pairs (37). There was substantial genetic influence on the trait of neuroticism and, to a lesser degree, on symptoms of anxiety and depression but no evidence for the heritability of categorical anxiety disorders. An implication of this study may be that searching for genes for categorical diagnoses such as panic disorder may be less fruitful than trying to identify genes influencing an underlying, latent anxiety-proneness such as neuroticism, which may be more directly heritable. In this context, it is noteworthy that the first reported human anxiety phenotype associated with a specific genetic locus was neuroticism. In one study, Lesch and colleagues (64) found that a polymorphism in the promoter region of the serotonin transporter gene was associated with higher scores on measures of neuroticism and trait anxiety.
Behavioral Inhibition
Another group of anxiety traits that appear to have a genetic basis are those related to behavioral inhibition and shyness. Although this is a somewhat heterogeneous group of phenotypes, the key feature appears to be autonomic/limbic arousal and decreased activity when an individual is confronted with an unfamiliar situation or social environment. Features of behavioral inhibition have been observed in many species, including rodents, dogs, and primates (65), suggesting that it is a robust and evolutionarily conserved temperamental phenotype. Gray (66) has proposed that the neuroanatomical substrate of anxiety is a “behavioral inhibition system,” subserved by limbic structures and triggered by threatening or novel stimuli. Cloninger (54) has described a similar temperamental construct as “harm avoidance” and suggests that it is mediated by polygenic influences on serotonergic function.
Kagan and colleagues have defined the temperamental construct of “behavioral inhibition to the unfamiliar” in children (53), (67). They have found that approximately 10%–15% of Caucasian children exhibit fearfulness, shyness, and quiet withdrawal in response to unfamiliar people, objects or situations; another 15% exhibit an “uninhibited” temperament characterized by an outgoing sociability and affective spontaneity. Physiologic correlates of behavioral inhibition include evidence of tonic sympathetic arousal and limbic hyperreactivity (67). Twin and adoption studies have demonstrated that the related constructs of shyness, introversion and behavioral inhibition are among the most heritable personality traits and appear to be distinct from neuroticism (68). Genetic factors appear to account for about 50% of the variance in behavioral inhibition during childhood (69). Although it is related to quantitative traits such as shyness, Kagan views behavioral inhibition as a qualitative trait: individuals who exhibit extremes of inhibited or uninhibited behavior represent discrete “types” that differ qualitatively from children who demonstrate intermediate degrees of inhibition (67).
A link between behavioral inhibition and anxiety disorders has emerged in a series of family studies (70). In these studies, children of parents with panic disorder/agoraphobia had high rates of behavioral inhibition, and parents of children with behavioral inhibition were more likely to have chronic, early-onset anxiety and multiple anxiety disorders. Behavioral inhibition was also associated with childhood anxiety disorders in both the children and their parents. These studies raise the possibility that behavioral inhibition reflects a constitutional “anxiety diathesis” or anxiety-proneness that is familial and predictive of liability to anxiety disorders, particularly panic disorder and social phobia (71). The existence of a heritable anxiety diathesis that may be variably expressed would be consistent with studies that have found elevated rates of several anxiety disorders in parents of anxious children (72)-(74) and in children of parents with anxiety disorders (75), (76).
FUTURE DIRECTIONS
Optimizing the Definition of “Genetic Caseness”
For the purposes of genetic linkage and association studies of categorical diagnoses, identifying a core phenotype that most closely reflects genetic “caseness” is essential. Defining a phenotype that is highly prevalent among relatives of affected probands and rare in the general population (i.e., maximizing lambdaR) increases the power of linkage studies(4)(35). Among the strategies available to accomplish this, three are discussed here.
Ascertaining phenotypic extremes. In designing gene mapping studies, selecting probands with early-onset anxiety disorders may enrich the sample for genetic cases. This approach has been used to minimize genetic heterogeneity and phenocopies within a sample (3). A recent study from Goldstein and colleagues (28) provided strong evidence that early-onset panic disorder is indeed associated with greater familial loading for the disorder. In a large, direct-interview family study, they found that relatives of probands who developed panic disorder before age 20 had a 17-fold higher risk of panic disorder than relatives of comparison subjects, while relatives of probands with later-onset panic disorder had a sixfold higher risk than relatives of comparison subjects. Relatives of the early-onset panic probands had higher rates of agoraphobia but did not differ from the relatives of later-onset panic probands in age at onset of panic or in symptom profiles.
Childhood anxiety disorders have been associated with an earlier age at onset of panic disorder/agoraphobia, more avoidance, more severe disorder, and more comorbidity (75), (77)-(80), possibly reflecting an underlying anxiety diathesis. The data on behavioral inhibition and familial risk for anxiety disorders are also consistent with the idea that early-onset anxiety may define a highly familial form of disorder. Ascertaining probands who have unusually severe disorder may also improve the genetic homogeneity of clinical samples (81).
A more general approach to optimizing the definition of genetic caseness involves analyzing family and twin data to determine which phenotypic features are associated with the greatest familiality and heritability. For example, on the basis of the data reviewed earlier, one might propose that expression of a heritable anxiety diathesis would include anxious temperament, comorbid panic and phobic disorders, continuing anxiety disorders from childhood to adulthood, and multiple affected family members. Although it would require an extensive database, such a hypothesis is testable. Familial recurrence risks or twin concordance rates could be calculated for this composite phenotype (or some subset of it) and compared to recurrence risks for panic or phobic disorders alone. An alternative, and perhaps more fruitful, strategy would be to analyze a range of phenotypic data without a priori hypotheses about which are the most salient. Such an approach, using logistic regression modeling, has been illustrated in studies of bipolar disorder and attention deficit hyperactivity disorder (82), (83). By including data on symptoms of panic and phobic disorders (e.g., panic attacks, phobias) as well as anxiety traits (e.g., neuroticism, behavioral inhibition) in such a model, one might empirically construct an improved definition of genetic caseness that incorporates both categorical and dimensional phenotypes. Of course, to do so would require a family or twin study database that comprises such a range of phenotypic data. In one small study (84), logistic regression modeling indicated that higher levels of the temperamental construct “emotionality” were predictive of caseness among siblings of probands with depression or anxiety disorders.
Identification of elemental phenotypes. A related approach would aim at identifying phenotypic elements of anxiety disorders that are more proximally related to genetic factors than are categorical anxiety diagnoses. The features that make up a clinical diagnosis of panic disorder may combine elements that are under the control of distinct genetic loci, as was recently suggested for obsessive-compulsive disorder (85). If so, the genetic architecture of the disorder could be much more complicated than that of the elements considered individually. Analysis of clinical data on panic disorder families may reveal distinct symptom clusters that may be under independent genetic influence. A suggestion of this was provided by Briggs and colleagues (86), who applied principal-components analysis to data from the Cross-National Panic Study and identified two symptom groups distinguished by the presence or absence of prominent respiratory symptoms. These subgroups appeared to be biologically meaningful because the group with prominent respiratory symptoms reported more spontaneous panic attacks and responded preferentially to imipramine, while the other group suffered more situational panic attacks and responded somewhat more to alprazolam.
Trait markers and spectrum phenotypes. The use of biological trait markers that may more closely reflect brain function than do clinical diagnoses has also been recommended as a strategy to simplify the genetic analysis of complex psychiatric disorders (4). This approach may also identify phenotypic spectra that are genetically related and associated with a higher lambdaS than the clinical diagnosis.
In the case of panic disorder, studies of the biological basis of panic attacks suggest several candidates for trait markers. In fact, panic disorder has emerged as one of the few psychiatric disorders whose symptoms can be provoked and studied under laboratory conditions. Overall, approximately 60%–75% of patients with panic disorder experience panic attacks in response to lactate infusion compared to 10%–15% of control subjects (87). Several other agents have been reported to provoke panic attacks more frequently in panic disorder patients including carbon dioxide (CO2), yohimbine, cholescystokinin, and caffeine (88). The mechanism by which these agents trigger panic attacks is unknown, but treatment with antipanic medications can block provoked panic attacks, suggesting that a neurobiologic abnormality may be involved.
Laboratory provocation tests may be useful in defining biologic subtypes of panic disorder or in identifying panic susceptibility among relatives of panic disorder probands. On the basis of family history data, a link between lactate-induced panic and familial risk of panic or other anxiety disorders has been reported (89), (90). However, a methodologically more rigorous direct-interview family study did not support this link (91).
Studies of CO2 inhalation have shown more promise (92)-(94). Perna and colleagues (92) found that panic disorder patients and subjects with a history of subsyndromal unexpected panic attacks had similarly elevated rates of panic in response to CO2 inhalation compared with normal control subjects. A family history of panic disorder was reported by 30% of the panic disorder patients, 31% of subjects with a history of unexpected panic attacks, and only 2% of normal control subjects. In another study (93), first-degree relatives of panic disorder patients had a rate of CO2-provoked panic that was significantly lower than that of the panic disorder patients but 12-fold higher than that of normal control subjects. These studies raise the possibility that CO2-hypersensitivity represents a trait marker for the genetic liability for panic attacks. Whether the CO2 inhalation test has sufficient specificity to make it a useful tool in genetic studies of panic disorder remains to be established. However, the identification of biological markers of anxiety disorders may provide a crucial handle for gene mapping studies and should continue to be a major focus of research. Because false-positive misclassification can dramatically reduce the power to detect linkage, the emphasis in identifying phenotypic indicators should be on maximizing their specificity (95).
Incorporating Quantitative Traits and Temperaments
Because quantitative assessments can incorporate more information than categorical assessments, such measures may facilitate gene-mapping efforts. In a recent illustration of this phenomenon, Brzustowicz and colleagues (96) found that a locus on chromosome 6p was linked to a quantitative measure of positive symptoms but not to the categorical diagnosis of schizophrenia. By examining temperaments and traits that may underlie anxiety disorders, we may circumvent the problem of the ambiguous boundaries of diagnostic categories. Self-report measures with good psychometric properties are available to measure neuroticism, harm avoidance, and other forms of trait anxiety. In the case of behavioral inhibition, the use of behavioral ratings offers a degree of standardization that should enhance the reliability of phenotypic assessments. Gene mapping studies of these phenotypes may be an important complement to studies of anxiety disorders. As discussed earlier, genetic influences on these traits may be greater than on the categorically defined anxiety disorders. In designing linkage studies, investigators could select probands who meet criteria for categorical diagnoses and also score highly on quantitative trait measures related to panic and phobic anxiety. Such a strategy would allow analyses of both the categorical and quantitative phenotypes. Risch and Zhang (97) have shown that the power of sib-pair linkage studies of quantitative traits is dramatically increased by selecting either extremely concordant or extremely discordant pairs.
Further investigations of genetic aspects of anxious traits would be useful. For example, “anxiety sensitivity” is a trait-like fearfulness of somatic symptoms of anxiety that has been shown to predict susceptibility to panic attacks (98); however, little is known about whether individual differences in this trait have a genetic basis. Additional studies are also needed to test the notion that clinical diagnoses can represent the extremes of quantitative traits.
Animal Models
Animal models offer a powerful tool for the genetic dissection of complex human disorders (99). The availability of highly inbred mouse strains eliminates the problem of genetic heterogeneity, and the ability to control environmental conditions minimizes the problem of phenocopies. Given their short breeding times and the ability to use large numbers of animals, limitations of statistical power in the mapping of quantitative traits can also be overcome. Individual genes can be inserted into (transgenic mice) or deleted from (knockout mice) the genome of a strain in order to evaluate the effect of specific genes. The importance of these models lies in the fact that the human genome has extensive homology with the genomes of mice and rats. A gene identified in a rodent model is likely to have a human homologue, and maps of conserved regions of DNA sequence (synteny homology) in mice and humans are readily available (100).
Several well-characterized animal models of anxiety already exist. One of the best characterized anxiety phenotypes in mice is that of “emotionality,” which appears to be analogous to anxious temperament in humans. Like behaviorally inhibited children, these mice exhibit arousal and reduced activity in novel environments. Among inbred strains of mice, this phenotype appears to be under strong genetic control (101) and several quantitative trait loci influencing emotionality have already been mapped (102), (103). In parallel with human studies, these animal models represent an important growing library of candidate loci for human anxiety.
CONCLUSIONS
We have reviewed the parallel efforts to characterize the genetics of anxiety in terms of either categorical or dimensional phenotypes. Converging lines of evidence from family/genetic studies indicate that panic and phobic anxiety are influenced by genetic factors. Of the anxiety disorders, panic disorder has the strongest evidence of a genetic component, but identification of the specific genes involved may require further refinement of the phenotype definition. Anxious temperaments have also been shown to be heritable and animal models of these phenotypes may facilitate gene mapping efforts. The reported association of the serotonin transporter gene with anxious traits is an encouraging example of the value of dimensional phenotype definitions.
One conceptualization that incorporates evidence from both of these approaches is the notion of an “anxiety diathesis”— a quantitative dimension of anxiety-proneness, which, in the extreme, may appear as qualitatively distinctive anxiety disorders such as panic disorder, agoraphobia, and social phobia (71). Although this construct is intuitively appealing, it still requires an operational definition. An important prerequisite to the mapping of panic/phobic disorder genes, then, may be to define the “diathesis” phenotype so as to optimize its heritability.
To accomplish this, the agenda for future studies should include efforts to define the relationship between clinical diagnoses and quantitative traits. Do individuals with clinically diagnosed anxiety disorders reliably and specifically exhibit elevated scores on measures of traits such as harm avoidance? Another priority will be to continue the search for psychobiological trait markers of anxiety disorder susceptibility, which could be used to refine the phenotype definition.
At the level of linkage and association studies, temperamental phenotypes such as behavioral inhibition may prove more amenable to gene mapping than are categorical diagnoses alone. The ascertainment of probands with early-onset anxiety disorders, which appear to be more familial, may also improve the power of genetic studies. Finally, animal models may be a key component in the genetic dissection of anxiety, as they proved to be for obesity (104), another complex phenotype.
The search for anxiety genes is in its early stages, but the importance of the endeavor may be substantial. The identification of specific susceptibility genes would signal a major advance in our understanding of the pathophysiology of anxiety at a molecular level. Practical consequences of cloning such genes would include the ability to develop methods of early detection of individuals at risk, targeted prevention strategies, and more specific and effective pharmacotherapeutics. A potentially more important consequence may be from the process rather than the outcome of gene mapping studies. The search for susceptibility genes in psychiatry will create the need for a careful reexamination of the boundaries of our diagnostic categories. Whether anxiety phenotypes can be collapsed with depression into a “general neurotic syndrome” (56), whether anxiety and depression are overlapping but distinguishable entities (105), and whether there are multiple discrete anxiety disorders that are also distinct from depression (9) are critical questions that the genetic epidemiology of anxiety disorders may help to answer. The project of constructing a genetic nosology for the purpose of linkage and association studies may well have implications for the further maturation of psychiatric nosology as a whole.
Received Oct. 20, 1997; revision received Feb. 19, 1998; accepted March 27, 1998. From the Department of Psychiatry, Massachusetts General Hospital; the Massachusetts Mental Health Center and Harvard Institute of Psychiatric Epidemiology and Genetics, Boston; and the Department of Epidemiology, Harvard School of Public Health, Boston.. Address reprint requests to Dr. Smoller, Department of Psychiatry, Massachusetts General Hospital, 15 Parkman St., WACC-815, Boston, MA 02114; [email protected] (e-mail). Supported in part by NIMH grant MH-17119 (Dr. Smoller).
 |
 |
1. Brown F: Heredity in the psychoneuroses. Proc R Soc Med 1942; 35:785–790Medline, Google Scholar
2. Lendon C, Ashall F, Goate A: Exploring the etiology of Alzheimer disease using molecular genetics. JAMA 1997; 277:825–831Crossref, Medline, Google Scholar
3. Lander ES, Schork NJ: Genetic dissection of complex traits. Science 1994; 265:2037–2048Crossref, Medline, Google Scholar
4. Tsuang M, Faraone S, Lyons M: Identification of the phenotype in psychiatric genetics. Eur Arch Psychiatry Clin Neurosci 1993; 243:131–142Crossref, Medline, Google Scholar
5. Knowles JA, Weissman MM: Panic disorder and agoraphobia, in American Psychiatric Press Review of Psychiatry, vol 14. Edited by Oldham JM, Riba MB. Washington, DC, American Psychiatric Press, 1995, pp 383-404Google Scholar
6. Knowles J, Mannuzza S, Fyer A: Heritability of social anxiety, in Social Phobia: Clinical and Research Perspectives. Edited by Stein M. Washington, DC, American Psychiatric Press, 1995, pp 147-161Google Scholar
7. Da Costa J: On irritable heart: a clinical study of a form of functional cardiac disorder and its consequences. Am J Med Sci 1871; 61:17–52Google Scholar
8. Freud S: Obsessions and phobias: their psychical mechanisms and their aetiology, in Early Psychoanalytic Writings. Edited by Rieff P. New York, Macmillan, 1963, pp 83-91Google Scholar
9. Klein D: Anxiety reconceptualized, in Anxiety: New Research and Changing Concepts. Edited by Klein D, Rabkin J. New York, Raven Press, 1981, pp 235-263Google Scholar
10. Marks I: The classification of phobic disorders. Br J Psychiatry 1970; 116:377–386Crossref, Medline, Google Scholar
11. Widiger T, Frances A, Pincus H, Ross R, First M, Davis W (eds): DSM-IV Sourcebook. Washington, DC, American Psychiatric Press, 1996Google Scholar
12. Barlow D, Brown T, Craske M: Definitions of panic attacks and panic disorder in the DSM-IV: implications for research. J Abnorm Psychol 1994; 103:553–564Crossref, Medline, Google Scholar
13. Crowe RR, Noyes R, Pauls DL, Slymen D: A family study of panic disorder. Arch Gen Psychiatry 1983; 40:1065–1069Crossref, Medline, Google Scholar
14. Noyes R Jr, Crowe RR, Harris EL, Hampa BJ, McChesney CM, Chaudry DR: Relationship between panic disorder and agoraphobia: a family study. Arch Gen Psychiatry 1986; 43:227–232Crossref, Medline, Google Scholar
15. Mendlewicz J, Papdimitriou G, Wilmotte J: Family study of panic disorder: comparison with generalized anxiety disorder, major depression and normal subjects. Psychiatr Genet 1993; 3:73–78Crossref, Google Scholar
16. Maier W, Lichtermann D, Minges J, Oehrlein A, Franke P: A controlled family study in panic disorder. J Psychiatr Res 1993; 27(suppl 1):79–87Google Scholar
17. Weissman MM, Wickramaratne P, Adams PB, Lish JD, Horwath E, Charney D, Woods SW, Leeman E, Frosch E: The relationship between panic disorder and major depression: a new family study. Arch Gen Psychiatry 1993; 50:767–780Crossref, Medline, Google Scholar
18. Mannuzza S, Chapman TF, Klein DF, Fyer AJ: Familial transmission of panic disorder: effect of major depression comorbidity. Anxiety 1994/1995; 1:180–185Google Scholar
19. Fyer AJ, Mannuzza S, Chapman TF, Martin LY, Klein DF: Specificity in familial aggregation of phobic disorders. Arch Gen Psychiatry 1995; 52:564–573Crossref, Medline, Google Scholar
20. Fyer A, Mannuzza S, Chapman T, Lipsitz J, Martin L, Klein D: Panic disorder and social phobia: effects of comorbidity on familial transmission. Anxiety 1996; 2:173–178Crossref, Medline, Google Scholar
21. Vieland V, Goodman D, Chapman T, Fyer A: New segregation analysis of panic disorder. Am J Med Genet 1996; 67:147–153Crossref, Medline, Google Scholar
22. Fyer A, Mannuzza S, Gallops S, Martin L, Aaronson C, Gorman J, Liebowitz M, Klein D: Familial transmission of simple phobias and fears. Arch Gen Psychiatry 1990; 47:252–256Crossref, Medline, Google Scholar
23. Fyer A, Mannuzza S, Chapman T, Liebowitz M, Klein D: A direct interview family study of social phobia. Arch Gen Psychiatry 1993; 50:286–293Crossref, Medline, Google Scholar
24. Stein MB, Chartier MJ, Hazen AL, Kozak MV, Tancer ME, Lander S, Furer P, Chubaty D, Walker JR: A direct-interview family study of generalized social phobia. Am J Psychiatry 1998; 155:90–97Link, Google Scholar
25. Wickramaratne P, Weissman M: Using family studies to understand comorbidity. Eur Arch Psychiatry Clin Neurosci 1993; 243:150–157Crossref, Medline, Google Scholar
26. Goldstein RB, Weissman MM, Adams PB, Horwath E, Lish JD, Charney D, Woods SW, Sobin C, Wickramaratne PJ: Psychiatric disorders in relatives of probands with panic disorder and/or major depression. Arch Gen Psychiatry 1994; 51:383–394Crossref, Medline, Google Scholar
27. Horwath E, Wolk SI, Goldstein RB, Wickramaratne P, Sobin C, Adams P, Lish JD, Weissman MM: Is the comorbidity between social phobia and panic disorder due to familial cotransmission or other factors? Arch Gen Psychiatry 1995; 52:574–582Google Scholar
28. Goldstein R, Wickramaratne P, Horwath E, Weissman M: Familial aggregation and phenomenology of “early”-onset (at or before age 20 years) panic disorder. Arch Gen Psychiatry 1997; 54:271–278Crossref, Medline, Google Scholar
29. Noyes R Jr, Clarkson C, Crowe RR, Yates WR, McChesney CM: A family study of generalized anxiety disorder. Am J Psychiatry 1987; 144:1019-1024Link, Google Scholar
30. Maier W, Minges J, Lichtermann D: The familial relationship between panic disorder and unipolar depression. J Psychiatr Res 1995; 29:375–388Crossref, Medline, Google Scholar
31. Torgersen S: Comorbidity of major depression and anxiety disorders in twin pairs. Am J Psychiatry 1990; 147:1199–1202Link, Google Scholar
32. Biederman J, Rosenbaum J, Bolduc E, Faraone S, Hirshfeld D: A high risk study of young children of parents with panic disorder and agoraphobia with and without comorbid major depression. Psychiatry Res 1991; 37:333–348Crossref, Medline, Google Scholar
33. Kendler K, Neale M, Kessler R, Heath A, Eaves L: Major depression and phobias: the genetic and environmental sources of comorbidity. Psychol Med 1993; 23:361–371Crossref, Medline, Google Scholar
34. Kendler K, Heath A, Martin M, Eaves L: Symptoms of anxiety and symptoms of depression: same genes, different environments? Arch Gen Psychiatry 1987; 44:451–457Google Scholar
35. Risch N: Linkage strategies for genetically complex traits, II: the power of affected relative pairs. Am J Hum Genet 1990; 46:229–241Medline, Google Scholar
36. Torgersen S: Genetic factors in anxiety disorders. Arch Gen Psychiatry 1983; 40:1085–1089Crossref, Medline, Google Scholar
37. Andrews G, Stewart G, Allen R, Henderson A: The genetics of six neurotic disorders: a twin study. J Affect Disord 1990; 19:23–29Crossref, Medline, Google Scholar
38. Skre I, Onstad S, Torgersen S, Lygren S, Kringlen E: A twin study of DSM-III-R anxiety disorders. Acta Psychiatr Scand 1993; 88:85–92Crossref, Medline, Google Scholar
39. Perna G, Caldirola D, Arancio C, Bellodi L: Panic attacks: a twin study. Psychiatry Res 1997; 66:69–71Crossref, Medline, Google Scholar
40. Kendler KS, Neale MC, Kessler RC, Heath A, Eaves L: The genetic epidemiology of phobias in women. Arch Gen Psychiatry 1992; 49:273–281Crossref, Medline, Google Scholar
41. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Generalized anxiety disorder in women. Arch Gen Psychiatry 1992; 49:267–272Crossref, Medline, Google Scholar
42. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Panic disorder in women: a population-based twin study. Psychol Med 1993; 23:397–406Crossref, Medline, Google Scholar
43. Kendler KS, Walter EE, Neale MC, Kessler RC, Heath AC, Eaves LJ: The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Arch Gen Psychiatry 1995; 52:374–383Crossref, Medline, Google Scholar
44. Neale M, Walters E, Eaves L, Kessler R, Heath A, Kendler K: Genetics of blood-injury fears and phobias: a population-based twin study. Am J Med Genet 1994; 54:326–334Crossref, Medline, Google Scholar
45. Pauls D: Behavioural disorders: lessons in linkage. Nat Genet 1993; 3:4–5Crossref, Medline, Google Scholar
46. Torgersen S: The nature and origin of common phobic fears. Br J Psychiatry 1979; 134:343–351Crossref, Medline, Google Scholar
47. Rose R, Ditto W: A developmental-genetic analysis of common fears from early adolescence to early adulthood. Child Dev 1983; 54:361–368Crossref, Medline, Google Scholar
48. Stevenson J, Batten N, Cherner M: Fears and fearfulness in children and adolescents: a genetic analysis of twin data. J Child Psychol Psychiatry 1992; 33:977–985Crossref, Medline, Google Scholar
49. Thapar A, McGuffin P: Are anxiety symptoms in childhood heritable? J Child Psychol Psychiatry 1995; 36:439–447Google Scholar
50. Phillips K, Fulker D, Rose R: Path analysis of seven fear factors in adult twin and sibling pairs and their parents. Genet Epidemiol 1987; 4:345–355Crossref, Medline, Google Scholar
51. Kendler K, Walters E, Truett K, Heath A, Neale M, Martin N, Eaves L: A twin-family study of self-report symptoms of panic-phobia and somatization. Behav Genet 1995; 25:499–515Crossref, Medline, Google Scholar
52. Slater E, Slater P: A heuristic theory of neurosis. J Neurol Psychiatry 1944; 7:49–55Crossref, Medline, Google Scholar
53. Kagan J, Reznick J, Clarke C, Snidman N, Garcia-Coll C: Behavioral inhibition to the unfamiliar. Child Dev 1984; 55:2212–2225Crossref, Google Scholar
54. Cloninger C: A unified biosocial theory of personality and its role in the development of anxiety states. Psychiatr Dev 1986; 3:167–226Google Scholar
55. Eysenck H, Eysenck S: Eysenck Personality Questionnaire Manual. San Diego, Calif, EdITS, 1975Google Scholar
56. Tyrer P: Neurosis divisible? Lancet 1985; 1:685–688Google Scholar
57. Young J, Fenton G, Lader M: The inheritance of neurotic traits: a twin study of the Middlesex Hospital Questionnaire. Br J Psychiatry 1971; 119:393–398Crossref, Medline, Google Scholar
58. Floderus-Myrhed B, Pedersen N, Rasmuson I: Assessment of heritability for personality, based on a short-form of the Eysenck Personality Inventory: a study of 12,898 twin pairs. Behav Genet 1980; 10:153–162Crossref, Medline, Google Scholar
59. Rose R, Koskenvuo M, Kaprio J, Sarna S, Langinvainio H: Shared genes, shared experiences, and similarity of personality: data from 14,288 adult Finnish co-twins. J Pers Soc Psychol 1988; 54:161–171Crossref, Medline, Google Scholar
60. Andrews G, Stewart G, Morris-Yates A, Holt P, Henderson S: Evidence for a general neurotic syndrome. Br J Psychiatry 1990; 157:6–12Crossref, Medline, Google Scholar
61. Jardine R, Martin N, Henderson A: Genetic covariation between neuroticism and the symptoms of anxiety and depression. Genet Epidemiol 1984; 1:89–107Crossref, Medline, Google Scholar
62. Martin N, Jardine R, Andrews G, Heath A: Anxiety disorders and neuroticism: are there genetic factors specific to panic? Acta Psychiatr Scand 1988; 77:698–706Google Scholar
63. Mackinnon A, Henderson A, Andrews G: Genetic and environmental determinants of the lability of trait neuroticism and the symptoms of anxiety and depression. Psychol Med 1990; 20:581–590Crossref, Medline, Google Scholar
64. Lesch K-P, Bengel D, Heils A, Sabol S, Greenberg B, Petri S, Benjamin J, Muller C, Hamer D, Murphy D: Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 1996; 274:1527–1531Crossref, Medline, Google Scholar
65. Marks I: Fears, Phobias and Rituals. New York, Oxford University Press, 1987Google Scholar
66. Gray J: Issues in the neuropsychology of anxiety, in Anxiety and the Anxiety Disorders. Edited by Tuma A, Maser J. Hillsdale, NJ, Lawrence Erlbaum Associates, 1985, pp 5-26Google Scholar
67. Kagan J, Reznick S, Snidman N: Biological bases of childhood shyness. Science 1988; 240:167–171Crossref, Medline, Google Scholar
68. Plomin R, Daniels D: Genetics and shyness, in Shyness: Perspectives on Research and Treatment. Edited by Jones W, Cheek J, Briggs S. New York, Plenum, 1986, pp 63-90Google Scholar
69. Robinson J, Kagan J, Reznick J, Corley R: The heritability of inhibited and uninhibited behavior: a twin study. Dev Psychol 1992; 28:1030–1037Crossref, Google Scholar
70. Rosenbaum JF, Biederman J, Bolduc-Murphy EA, Faraone SV, Chaloff J, Hirshfeld D, Kagan J: Behavioral inhibition in childhood: a risk factor for anxiety disorders. Harvard Rev Psychiatry 1993; 1:2–16Crossref, Medline, Google Scholar
71. Rosenbaum J, Biederman J, Hirshfeld D, Bolduc E, Chaloff J: Behavioral inhibition in children: a possible precursor to panic disorder or social phobia. J Clin Psychiatry 1991; 52:11(suppl):5–9Google Scholar
72. Bernstein GA, Garfinkel BD: Pedigrees, functioning, and psychopathology in families of school phobic children. Am J Psychiatry 1988; 145:70–74Link, Google Scholar
73. Last CG, Hersen M, Kazdin AE, Francis G, Grubb HJ: Psychiatric illness in the mothers of anxious children. Am J Psychiatry 1987; 144:1580–1583Link, Google Scholar
74. Last C, Hersen M, Kazdin A, Orvaschel H, Perrin S: Anxiety disorders in children and their families. Arch Gen Psychiatry 1991; 48:928–934Crossref, Medline, Google Scholar
75. Berg I: School phobia in the children of agoraphobic women. Br J Psychiatry 1976; 128:86–89Crossref, Medline, Google Scholar
76. Turner S, Beidel D, Costello A: Psychopathology in the offspring of anxiety disorders patients. J Consult Clin Psychol 1987; 55:229–235Crossref, Medline, Google Scholar
77. Gittelman R, Klein D: Relationship between separation anxiety and panic and agoraphobic disorders. Psychopathology 1984; 17(suppl 1):56–65Google Scholar
78. Buller R, Maier W, Goldenberg I, Lavori P, Benkert O: Chronology of panic and avoidance, age of onset in panic disorder, and prediction of treatment response. Eur Arch Psychiatry Clin Neurosci 1991; 240:163–168Crossref, Medline, Google Scholar
79. Battaglia M, Bertella S, Politi E, Bernardeschi L, Perna G, Gabriele A, Bellodi L: Age at onset of panic disorder: influence of familial liability to the disease and of childhood separation anxiety disorder. Am J Psychiatry 1995; 152:1362–1364Link, Google Scholar
80. Pollack MH, Otto MW, Sabatino S, Majcher D, Worthingon JJ, McArdle ET, Rosenbaum JF: Relationship of childhood anxiety to adult panic disorder: correlates and influence on course. Am J Psychiatry 1996; 153:376–381Link, Google Scholar
81. Risch N, Merikangas K: Linkage studies of psychiatric disorders. Eur Arch Psychiatry Clin Neurosci 1993; 243:143–149Crossref, Medline, Google Scholar
82. Blacker D, Lavori P, Faraone S, Tsuang M: Unipolar relatives in bipolar pedigrees: a search for indicators of underlying bipolarity. Am J Med Genet 1993; 48:192–199Crossref, Medline, Google Scholar
83. Milberger S, Faraone S, Biederman J, Testa M, Tsuang M: New phenotype definition of attention deficit hyperactivity disorder in relatives for genetic analyses. Am J Med Genet 1996; 67:369–377Crossref, Medline, Google Scholar
84. Kelvin R, Goodyer I, Altham P: Temperament and psychopathology amongst siblings of probands with depressive and anxiety disorders. J Child Psychol Psychiatry 1996; 37:543–550Crossref, Medline, Google Scholar
85. Leckman JF, Grice DE, Boardman J, Zhang H, Vitale A, Bondi C, Alsobrook J, Peterson BS, Cohen DJ, Rasmussen SA, Goodman WK, McDougle CJ, Pauls DL: Symptoms of obsessive-compulsive disorder. Am J Psychiatry 1997; 154:911–917Link, Google Scholar
86. Briggs AC, Stretch DD, Brandon S: Subtyping of panic disorder by symptom profile. Br J Psychiatry 1993; 163:201–209Crossref, Medline, Google Scholar
87. Cowley DS, Arana GW: The diagnostic utility of lactate sensitivity in panic disorder. Arch Gen Psychiatry 1990; 47:227–284Crossref, Google Scholar
88. Krystal J, Deutsch D, Charney D: The biological basis of panic disorder. J Clin Psychiatry 1996; 57(suppl 10):23–31Google Scholar
89. Cowley D, Dunner D: Response to sodium lactate in panic disorder: relationship to presenting clinical variables. Psychiatry Res 1988; 25:253–259Crossref, Medline, Google Scholar
90. Balon R, Jordan M, Pohl R, Yeragani VK: Family history of anxiety disorders in control subjects with lactate-induced panic attacks. Am J Psychiatry 1989; 146:1304–1306Link, Google Scholar
91. Reschke AH, Mannuzza S, Chapman TF, Lipsitz JD, Liebowitz MR, Gorman JM, Klein DF, Fyer AJ: Sodium lactate response and familial risk for panic disorder. Am J Psychiatry 1995; 152:277–279Link, Google Scholar
92. Perna G, Gabriele A, Caldirola D, Bellodi L: Hypersensitivity to inhalation of carbon dioxide and panic attacks. Psychiatry Res 1995; 57:267–273Crossref, Medline, Google Scholar
93. Perna G, Cocchi S, Bertani A, Arancio C, Bellodi L: Sensitivity to 35% CO2 in healthy first-degree relatives of patients with panic disorder. Am J Psychiatry 1995; 152:623–625Link, Google Scholar
94. Coryell W: Hypersensitivity to carbon dioxide as a disease-specific trait marker. Biol Psychiatry 1997; 41:259–263Crossref, Medline, Google Scholar
95. Faraone SV, Kremen WS, Lyons MJ, Pepple JR, Seidman LJ, Tsuang MT: Diagnostic accuracy and linkage analysis: how useful are schizophrenia spectrum phenotypes? Am J Psychiatry 1995; 152:1286–1290Google Scholar
96. Brzustowicz L, Honer W, Chow E, Hogan J, Hodgkinson K, Bassett A: Use of a quantitative trait to map a locus associated with severity of positive symptoms in familial schizophrenia to chromosome 6p. Am J Hum Genet 1997; 61:1388–1396Crossref, Medline, Google Scholar
97. Risch N, Zhang H: Extreme discordant sib pairs for mapping quantitative trait loci in humans. Science 1995; 268:1584–1589Crossref, Medline, Google Scholar
98. Schmidt N, Lerew D, Jackson R: The role of anxiety sensitivity in the pathogenesis of panic: prospective evaluation of spontaneous panic attacks during stress. J Abnorm Psychol 1997; 106:355–364Crossref, Medline, Google Scholar
99. Lander E, Botstein D: Mapping Mendelian factors underlying quantitative traits using RFLP linkage maps. Genetics 1989; 121:185–199Medline, Google Scholar
100. Fisher E: The contribution of the mouse to advances in human genetics. Adv Genet 1997; 35:155–205Crossref, Medline, Google Scholar
101. Trullas R, Skolnick P: Differences in fear motivated behaviors among inbred mouse strains. Psychopharmacology (Berl) 1993; 111:323–331Crossref, Medline, Google Scholar
102. Flint J, Corley R, DeFries JC, Fulker DW, Gray JA, Miller S, Collins AC: A simple genetic basis for a complex psychological trait in laboratory mice. Science 1995; 269:1432–1435Crossref, Medline, Google Scholar
103. Gershenfeld H, Neumann P, Mathis C, Crawley J, Li X, Paul S: Mapping quantitative trait loci for open-field behavior in mice. Behav Genet 1997; 27:201–210Crossref, Medline, Google Scholar
104. Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman J: Positional cloning of the mouse obese gene and its human homologue. Nature 1994; 372:425–431Crossref, Medline, Google Scholar
105. Clark L, Watson D: Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol 1991; 100:316–336Crossref, Medline, Google Scholar



