Psychiatric Symptoms and Syndromes Among Adolescent Children of Parents With Lithium-Responsive or Lithium-Nonresponsive Bipolar Disorder
Abstract
OBJECTIVE: The purpose of this pilot study was to describe the initial course of psychiatric illness in the adolescent children of parents with bipolar disorder who were divided into two groups on the basis of their response to long-term lithium monotherapy. METHOD: Proband parents met Research Diagnostic Criteria for bipolar illness and predetermined criteria for a clear response or nonresponse to lithium prophylaxis. All adolescent offspring were interviewed by a blinded interviewer using the Schedule for Affective Disorders and Schizophrenia for School-Age Children, and final diagnosis was made by blinded consensus. RESULTS: Psychiatrically ill children of lithium-responsive parents tended to have affective disorders that remitted and followed a recurrent course. Psychiatrically ill children of lithium-nonresponsive parents, however, manifested a broad range of psychopathology, had high rates of comorbid illnesses, and experienced nonremitting affective illnesses. CONCLUSIONS: These results suggest that family history and course of illness are important factors to consider in the diagnosis and pharmacological treatment of affective disorders.
It is estimated that in up to 30% of cases the onset of bipolar illness occurs before age 20, most often following puberty (1). If subsyndromal symptoms were taken into account, the proportion of early-onset cases would likely be higher. Despite the substantial prevalence, morbidity, and greater mortality associated with early-onset bipolar disorder, there is insufficient reliable information about its initial course.
Bipolar illness runs in families, probably on a genetic basis, and early onset may be a clinical marker of a particularly strong genetic effect (2). The few available studies of children of parents with bipolar disorder describe affective psychopathology such as dysthymia, major depression, and cyclothymia (3, 4). However, there have also been reports of a wide range of psychopathology and high rates of comorbid illnesses in at-risk offspring. These include conduct disorders, substance abuse, anxiety disorders, and attention deficit hyperactivity disorder (5, 6). This range of disturbance either suggests a lack of phenotypic specificity for bipolar disorder or illustrates difficulties in diagnosing childhood psychiatric disorders.
Previously completed studies have been limited by methodological weaknesses such as nonblind assessments of offspring and the inclusion of a heterogeneous group of parent probands. Heterogeneity among the parents may have contributed to the breadth of psychopathology reported in their offspring. A more homogeneous, genetically based subgroup of patients with bipolar disorder can be studied by focusing on the patients' responses to long-term lithium monotherapy (7).
In this pilot study we describe the psychiatric symptoms and syndromes manifested by the adolescent children of two groups of parents with bipolar disorder. The parents were divided into groups on the basis of their response to long-term lithium prophylaxis. We hypothesized that the children of parents with lithium-responsive bipolar disorder would manifest psychopathology clustering in the affective spectrum and following an episodic course and that the children of parents with lithium-nonresponsive bipolar disorder would manifest a broad range of psychopathology following a chronic course.
METHOD
Parent probands. Twenty-one offspring of 13 probands with lithium-responsive bipolar disorder and 15 offspring of 10 probands with lithium-nonresponsive bipolar disorder were included in this study. The parent probands represented a consecutive series of patients followed in an affective disorders specialty clinic. All probands met Research Diagnostic Criteria (8) for bipolar I illness and met specific criteria described elsewhere (7) for a clear response or nonresponse to long-term lithium monotherapy. Briefly, all patients had to have a high recurrence risk before they started to take lithium. Lithium responders had to remain episode free while receiving adequate lithium treatment (plasma level greater than 0.7 mmol/liter for more than 3 years), and lithium nonresponders had to have had at least two recurrences despite adequate lithium treatment. In all cases, the other parent was psychiatrically well.
Offspring. All male and female offspring between 10 and 25 years of age of proband parents were asked to participate. After a complete description of the study was given to the parent or parents and children, written informed consent was obtained. All consenting offspring were interviewed by one of us (A.D.), who was blind to proband affiliation, following the semistructured interview format of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (KIDDIE-SADS) (9). In addition, at least one parent was interviewed about each adolescent. Final DSM-IV diagnoses were made by consensus among the three of us who were blind to proband affiliation (P.G., M.A., and S.K.), using all other pertinent clinical information (KIDDIE-SADS, charts, and family history).
Statistics. A two-tailed Fisher's exact test was used to compare the number of affectively ill subjects with a remitting or a nonremitting initial episode and the number of affectively ill subjects with a recurrent or chronic (more than 2 years) course of illness between the groups (children of lithium responders versus children of lithium nonresponders).
RESULTS
Demographics. The children of lithium responders and the children of lithium nonresponders did not differ in median age at assessment (18 versus 20 years, respectively). There were proportionately more girls among the children of lithium nonresponders than among the children of lithium responders (80% versus 57%, respectively). Nineteen eligible children refused to participate (12 children of lithium responders; seven children of lithium nonresponders). According to family history data, there was no difference in affective status, age, or gender between consenting and refusing adolescents.
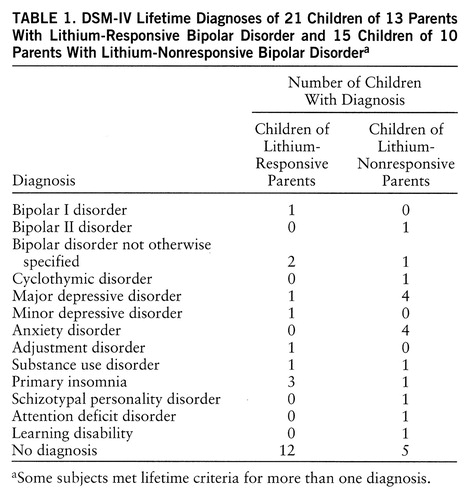
Diagnoses. Nine of the 21 children of lithium responders met DSM-IV criteria for at least one psychiatric disorder during their lifetime, compared with 10 of the 15 children of lithium nonresponders. Psychiatric diagnoses among the children of lithium responders tended to cluster within the affective domain, but the children of lithium nonresponders manifested a broad range of psychopathology (table 1).
Comorbidity. The affectively ill children of lithium nonresponders had a higher rate of comorbid illness than did affectively ill children of lithium responders. Specifically, only one of the children of lithium responders met criteria for primary insomnia as well as a later unrelated episode of major depression. By contrast, among the four children of lithium nonresponders with a history of major depression, two met criteria for a childhood anxiety disorder and one had an earlier unrelated history of substance abuse. Further, one of the children of lithium nonresponders met criteria for schizotypal personality disorder prior to bipolar illness and one cyclothymic child of a lithium nonresponder met criteria for primary insomnia.
Prodromal symptoms. Of the five children of lithium responders with an affective illness, only one manifested subsyndromal symptoms (episodic irritability). In the remaining four, the affective disturbance began as an episode of brief minor depression (recurrent in three cases). By comparison, six of the seven affectively ill children of lithium nonresponders showed chronic waxing and waning subsyndromal symptoms, including mood lability (N=4) and severe irritability (N=2).
Course of affective disorder. There was a clear difference between the groups in terms of the initial course of affective illness. All five affectively ill children of lithium responders had remitting affective episodes, compared with one of six affectively ill children of lithium nonresponders (p=0.01, Fisher's exact test). (One child of a lithium nonresponder was in the midst of an initial affective episode and was therefore excluded from these calculations.) Of those affectively ill children who had experienced at least two episodes or 2 years of illness, all three children of lithium responders had a recurrent course, while all five children of lithium nonresponders had a chronic course (p=0.02, Fisher's exact test).
DISCUSSION
The children of lithium responders tended to manifest psychiatric illnesses clustering in the affective domain, with few comorbid illnesses and an episodic course, compared with the children of lithium nonresponders, who had a broad range of psychopathology, more comorbid illnesses, and a chronic course. This result further supports the hypothesis that an excellent response to lithium prophylaxis is a clinical marker of a more homogeneous, genetically based subgroup of bipolar illness (7). Further, these findings suggest that family history, including course and treatment response in relatives with bipolar disorder, may be an important predictor of illness course and treatment response in adolescents manifesting primary affective disorders.
This pilot study is limited by small numbers. However, the validity of these findings is supported by the rigorous methodology and clear group differences. If these preliminary findings hold true in a larger study group, we will have a better understanding of the early course of primary affective illness in adolescents at risk and clues as to the rational use of pharmacotherapy in this patient population.
 |
Presented at the 16th Annual Meeting of the Canadian Academy of Child Psychiatry, Quebec, Sept. 28–Oct. 1, 1996. Received April 22, 1997; revision received Aug. 20, 1997; accepted Sept. 18, 1997. From the Affective Disorders Service, Royal Ottawa Hospital. Address reprint requests to Dr. Alda, Affective Disorders Service, Royal Ottawa Hospital, 1145 Carling Ave., Ottawa, Ont., Canada, K1Z 7K4; [email protected] (e-mail). Supported in part by a Research Fellowship from the Ontario Mental Health Foundation (Dr. Duffy) and by an Intermediate Research Fellowship from the Ontario Mental Health Foundation (Dr. Alda).
1. Goodwin FK, Jamison KR: Childhood and adolescence, in Manic Depressive Illness. New York, Oxford University Press, 1990, pp 186–209Google Scholar
2. Strober M: Family-genetic aspects of juvenile affective disorders, in The Depressed Child and Adolescent: Developmental and Clinical Perspectives. Edited by Goodyer IM. New York, Cambridge University Press, 1995, pp 149–170Google Scholar
3. Akiskal HS, Downs J, Jordan P, Watson S, Daugherty D, Pruitt DB: Affective disorders in referred children and younger siblings of manic-depressives: mode of onset and prospective course. Arch Gen Psychiatry 1985; 42:996–1003Google Scholar
4. Laroche C, Sheiner R, Lester E, Benierakis C, Marrache M, Engelsmann F, Cheifetz P: Children of parents with manic-depressive illness: a follow up study. Can J Psychiatry 1987; 32:563–569Crossref, Medline, Google Scholar
5. Gershon ES, McKnew D, Cytryn L, Hamovit J, Schreiber J, Hibbs E, Pellegrini D: Diagnoses in school-age children of bipolar affective disorder patients and normal controls. J Affect Disord 1985; 8:283–291Crossref, Medline, Google Scholar
6. Hammen C, Burge D, Burney E, Adrian C: Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Arch Gen Psychiatry 1990; 47:1112–1117Google Scholar
7. Grof P, Alda M, Grof E, Zvolsky P, Walsh M: Lithium response and genetics of affective disorders. J Affect Disord 1994; 32:85–95Crossref, Medline, Google Scholar
8. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978; 35:773–782Crossref, Medline, Google Scholar
9. Puig-Antich J, Chambers W: Schedule for Affective Disorders and Schizophrenia for School-Age Children (KIDDIE-SADS). New York, New York State Psychiatric Institute, Biometrics Research, 1978Google Scholar



