Transforming Discoveries About Cortical Microcircuits and Gamma Oscillations Into New Treatments for Cognitive Deficits in Schizophrenia
Abstract
The major cause of disability in schizophrenia is cognitive impairment, which remains largely refractory to existing treatments. This reflects the fact that antipsychotics and other therapies have not been designed to address specific brain abnormalities that cause cognitive impairment. This overview proposes that understanding how specific cellular and synaptic loci within cortical microcircuits contribute to cortical gamma oscillations may reveal treatments for cognitive impairment. Gamma oscillations are rhythmic patterns of high frequency (∼30–100 Hz) neuronal activity that are synchronized within and across brain regions, generated by a class of inhibitory interneurons that express parvalbumin, and recruited during a variety of cognitive tasks. In schizophrenia, both parvalbumin interneuron function and task-evoked gamma oscillations are deficient. While it has long been controversial whether gamma oscillations are merely a biomarker of circuit function or actually contribute to information processing by neuronal networks, recent neurobiological studies in mice have shown that disrupting or enhancing synchronized gamma oscillations can reproduce or ameliorate cognitive deficits resembling those seen in schizophrenia. In fact, transiently enhancing the synchrony of parvalbumin interneuron–generated gamma oscillations can lead to long-lasting improvements in cognition in mice that model aspects of schizophrenia. Gamma oscillations emerge from specific patterns of connections between a variety of cell types within cortical microcircuits. Thus, a critical next step is to understand how specific cell types and synapses generate gamma oscillations, mediate the effects of gamma oscillations on information processing, and/or undergo plasticity following the induction of gamma oscillations. Modulating these circuit loci, potentially in combination with other approaches such as cognitive training and brain stimulation, may yield potent and selective interventions for enhancing cognition in schizophrenia.
Despite the introduction of many second-generation antipsychotics over the past three decades, schizophrenia remains stubbornly disabling for most patients. It is now well understood that the major reason for this is cognitive impairment (1), which often predates frank psychosis, persists throughout the illness, and remains largely refractory to existing treatments such as antipsychotic medications (2, 3). The first antipsychotic medication, chlorpromazine, was discovered serendipitously, based on its calming effects. Additional antipsychotics were then chemically derived from chlorpromazine and similar compounds. Eventually, once dopamine and serotonin receptors were implicated in the pharmacology of many antipsychotics, new antipsychotics were developed based on their ability to block these receptors. Thus, antipsychotic medications have, from their inception, been directed at psychotic symptoms, rather than cognitive impairment.
Many other treatments have been tried for cognitive impairment in schizophrenia, but their current efficacy remains modest at best. This is perhaps not surprising, given that none of these have been developed on the basis of an understanding of what actually causes the cognitive deficits. Over the past 15 years, neuroscientists have been able to use new tools to conduct previously impossible experiments, in order to show how specific classes of neurons generate patterns of activity and how those patterns of activity contribute to aspects of cognition that are classically associated with schizophrenia. This overview focuses on specific patterns of activity known as gamma oscillations. Here, I present evidence that the deficits in gamma oscillations observed in schizophrenia are not merely symptoms of a malfunctioning cortex. Rather, gamma oscillations play an essential role in the proper functioning of cortical microcircuits; in particular, they enable the frontal cortex to perform essential aspects of executive function. This includes updating items stored in working memory and reappraising the salience of external cues. Gamma oscillations emerge from, and act upon, highly specific patterns of connections between a variety of cell types within cortical microcircuits. Thus, as we identify the cellular and synaptic loci that generate gamma oscillations, mediate their actions on cortical microcircuits, and undergo plasticity that is induced by gamma oscillations, targeting these loci may yield effective treatments for the cognitive deficits at the heart of schizophrenia.
What Are Gamma Oscillations and Where Do They Come From?
We often speak of brain activity as if it were a singular entity—for example, “activity in the prefrontal cortex increases during working memory tasks.” Of course, activity within any brain region has a more complex organization. In the temporal domain, neuronal activity tends to be organized into rhythms. These rhythms are synchronized across neurons within a brain region, and sometimes across brain regions as well. Thus, when electrical fields originating from many neurons are summed up, their peaks and troughs tend to align, giving rise to the characteristic “brain waves” that have been observed in EEG for almost a century. Gamma oscillations comprise the high end of frequencies typically resolvable via scalp EEG, that is, between 30 Hz and an upper limit that varies but is typically between 80 and 100 Hz. Because gamma oscillations reflect rhythmic activity that is synchronized across neurons, they can be observed across many scales, including scalp EEG, intracranial recordings of summed electrical activity (local field potentials), spiking activity from groups of neurons or individual neurons, and even in the subthreshold synaptic input to individual neurons.
The precise upper and lower bounds of frequencies that define gamma oscillations are somewhat arbitrary. That being said, there is something “special” about the range of frequencies associated with gamma oscillations, which is closely related to their underlying mechanism (and likely their function as well). One cycle of a gamma oscillation corresponds to ∼10–30 ms. This is very similar to the membrane time constant for most cortical neurons, that is, the effective window of time over which they integrate their inputs, and the time it takes for a neuron’s membrane potential to decay back toward its resting level. This is also very similar to the time constant associated with inhibitory (GABAergic) synapses, that is, the time it takes for a neuron to recover after it receives inhibitory synaptic input. For these reasons, one gamma cycle corresponds roughly to the time it takes a neuron to recover from inhibitory synaptic input and become responsive to excitatory input again. Gamma oscillations occur when the GABAergic neurons within a local cortical circuit become synchronized—in this scenario, GABAergic neurons will deliver synchronized synaptic inhibition to other neurons in the network (including themselves). This leads to a period of relative quiescence during which inhibition is high. Eventually, this inhibition decays, and neurons in the network (including GABAergic neurons) become active again, starting the next cycle. Thus, gamma oscillations are generated by the synaptic interactions within local cortical circuits, rather than being imposed by an external pacemaker.
At this point, it is important to note that measuring gamma oscillations is not the same as simply taking a neural signal (EEG, local field potential, spike rate, etc.), computing a power spectrum, and adding up the amount of power in the 30- to 90-Hz range. Even completely disorganized or random activity will have power in the gamma-frequency range. A “gamma oscillation” specifically occurs when levels of synaptic inhibition ebb and flow on timescales of 10–30 ms, producing the emergent dynamics described above.
What Is the Evidence Tying Gamma Oscillations to Schizophrenia?
Two major lines of evidence tie gamma oscillations to schizophrenia. First, in most cases (but not all [4]), gamma oscillations are generated by a specific class of cortical GABAergic interneurons that can be identified by their expression of the calcium-binding protein parvalbumin (PV) (5, 6). PV interneurons represent one of three major classes of cortical GABAergic interneurons, accounting for approximately 40% of all interneurons (7). Abnormalities in cortical PV interneurons are among the most well-established neuropathological findings in schizophrenia (3). In particular, schizophrenia is associated with lower levels of glutamic acid decarboxylase 67, the principal enzyme responsible for GABA synthesis, in the cell bodies and axon terminals of prefrontal PV interneurons (8–10), suggesting that the output from PV interneurons is reduced. The intrinsic properties of PV interneurons are also abnormal in schizophrenia (3); for example, levels of PV interneuron–specific potassium channels are reduced (11).
Second, in light of this link between PV interneurons and gamma oscillations, many groups have measured gamma oscillations in individuals with schizophrenia using EEG or magnetoencephalography (MEG) and found deficits. These consist of three different kinds of studies. Initially, many studies focused on the response to rhythmic trains of sensory stimulation, for example, the auditory steady-state response or responses to visual stimuli. These studies compared the steady-state amplitudes of evoked potentials during trains of stimuli at different frequencies. In schizophrenia, these studies found decreased amplitudes of rhythmic responses to gamma-frequency (e.g., 40 Hz) trains of sensory stimuli, whereas these amplitudes were normal during lower-frequency trains. This has been interpreted to indicate a deficit in the ability of cortical circuits to generate gamma-frequency activity (12–14). These deficits in the amplitudes of rhythmic responses to gamma-frequency auditory stimuli reflect decreases in both power (i.e., the amplitude of rhythmic activity) and phase locking (i.e., the consistency in the timing of the peak of a gamma oscillation that occurs following a stimulus). Furthermore, these deficits are present in first-episode patients (15) and actually predict the transition from a clinical high-risk state to psychosis (16). It is important to note, however, that in these studies, rhythmic activity was being driven (or at least entrained) by rhythmic external stimuli, as opposed to being intrinsically generated by cortical circuits.
A second class of studies examined gamma oscillations evoked by visual stimuli, including Gestalt stimuli (17), Mooney faces (18), visual oddball stimuli (15), and illusory contours (19). These studies generally found decreases in the power and/or phase locking of these visual stimulus-evoked gamma oscillations in schizophrenia that also occur in first-episode medication-naive patients (20). One potential caveat is that visual stimuli can elicit eye movements (microsaccades), which may produce artifactual increases in gamma power and cross-site synchronization (21). However, it is unclear to what extent these artifacts actually contaminate EEG and MEG recordings when appropriate references are used (22). Furthermore, many studies include data processing steps that may reject these kinds of artifacts, and these artifacts do not necessarily explain the occurrence of frequency-specific and/or phase-locked gamma oscillations following visual stimuli. A similar finding (less subject to potential eye movement–related confounding) is that gamma-frequency activity is also reduced in schizophrenia during auditory oddball tasks (23).
A third class of studies examined gamma oscillations, typically in frontal regions, evoked by cognitive tasks, which typically assay the cognitive domains that are impaired in schizophrenia (24). These include cognitive control tasks in both chronic and first-episode/medication-naive subjects (25, 26) and working memory tasks (27, 28). These studies have also found deficits in the amplitudes of task-evoked gamma oscillations.
Some EEG studies have measured power in the gamma-frequency band at rest or under baseline conditions. In contrast to the finding of decreased gamma-frequency activity evoked by sensory stimuli or tasks, these studies have sometimes found increases in total power in the gamma-frequency band under spontaneous or baseline conditions (29). As noted above, simply measuring the total power in a frequency band may be reflective of total neural activity, rather than the capacity of a circuit to generate rhythmic activity around specific frequencies when it is engaged by sensory stimuli or cognitive tasks. Therefore, we will draw a distinction between studies of baseline or spontaneous gamma power and those that specifically measure synchronized rhythmic activity induced by tasks or sensory stimuli.
What Is the Evidence That Deficient Gamma Oscillations Cause Cognitive Deficits (And Can Be Targeted to Improve Cognition)?
To summarize the preceding, gamma oscillations are patterns of synchronized rhythmic activity that emerge from interactions between excitatory and inhibitory neurons (primarily PV interneurons) in local cortical circuits. In schizophrenia, PV interneurons are abnormal and the gamma oscillations evoked by sensory stimuli or cognitive tasks have reduced power and/or synchrony. Of course this begs the question, what is the significance of these findings? Do deficits in the power and synchrony of gamma oscillations simply indicate that the underlying cortex is abnormal? Or do these oscillatory deficits themselves cause cognitive deficits? This is the corollary of a long-standing controversy in neuroscience: Do gamma oscillations simply indicate that brain circuits are active (akin to the roar of a V8 engine) or do these oscillations actually perform functions that enhance the performance of brain circuits (30, 31)?
Our laboratory has carried out studies in mice that provide direct evidence that gamma oscillations actually contribute to cognition, such that rescuing them may be critical for remediating cognitive deficits associated with schizophrenia. First, we studied mutant mice in which the development of PV interneurons is abnormal (32). After puberty, these mice develop deficits in a task that measures cognitive flexibility. In this task, mice dig in bowls and learn rules to find hidden food rewards. Different bowls contain different textured digging media (e.g., sand or wood chip) and are scented with different odors (e.g., garlic or coriander). Once mice learn that a single cue (e.g., the smell of garlic) reliably indicates the location of food, the rule undergoes an extradimensional shift, that is, a texture cue will become associated with reward. Whereas normal mice readily learn both an initial rule and the rule shift, mutant mice learn the initial rule normally, but become perseverative during the rule shift, continuing to make choices based on the original rule. This is reminiscent of the perseveration classically associated with schizophrenia in paradigms such as the Wisconsin Card Sorting Task (WCST). While no rodent task is a perfect analogue of the WCST, the rule shifting task, like the WCST, requires subjects to recognize that a rule has changed, suppress perseverative responses, and begin making choices based on cues that were previously irrelevant to trial outcomes. Like many cognitive control tasks, this rule shift task elicits increases in gamma oscillations in the prefrontal cortex, and these task-evoked gamma oscillations are deficient in the mutant mice that are perseverative on this task. Thus, while these mutant mice should not be considered a “mouse model of schizophrenia,” they do specifically model an association between PV interneuron dysfunction and the postpubertal onset of deficits in prefrontal-dependent cognitive flexibility and task-evoked gamma oscillations that occurs in schizophrenia.
In light of the previous discussion, we wondered whether restoring prefrontal gamma oscillations would rescue cognitive flexibility in these mice. We tested this using optogenetics, an approach that has revolutionized studies of neural circuits, in which light-sensitive proteins are expressed in a targeted group of cells so that light can be delivered to activate those cells at precise moments. In this case, we expressed the light-sensitive ion channel channelrhodopsin-2 (ChR2) in prefrontal interneurons, then flashed light at 40 Hz during rule shifts, to enhance interneuron-driven gamma oscillations during rule shifts. This intervention was sufficient to completely normalize performance on the rule shifting task in mutant mice. Two things about this effect were particularly notable. First, it was frequency specific: gamma-frequency stimulation (at 40 or 60 Hz) was effective, whereas delivering an equivalent amount of stimulation using a combination of frequencies above and below the gamma band was ineffective. Second, this effect was long-lasting. After a single session of stimulation, performance remained normal even when we retested mutant mice again weeks later (in the absence of any additional optogenetic stimulation).
These results showed that in mutant mice, enhancing gamma oscillations can have powerful therapeutic effects on the sorts of cognitive deficits seen in schizophrenia. However, they left open two outstanding questions. First, are gamma oscillations actually necessary for cognition in normal mice, or are they simply useful for enhancing cognition in mutant mice? Second, was the stimulation effective because it enhanced synchronized rhythmic brain activity, or did it act through some other mechanism? For example, perhaps gamma-frequency stimulation was effective simply because this frequency is particularly good for driving PV interneurons and eliciting GABAergic synaptic output, and maybe it is the total level of GABAergic synaptic output (not the organization of that output into a synchronized rhythm) that is important for circuit function.
To address this question, we conducted a follow-up study that focused on normal mice (33). First, we used a novel approach, in which we measured fluorescent signals from proteins that change their fluorescence based on the membrane voltage of PV interneurons. In this way, we were able to directly measure voltage signals from PV interneurons in the left and right prefrontal cortex of mice, and we found that when these mice learn a rule shift, rhythmic gamma-frequency activity in these PV interneurons become synchronized across the hemispheres. Next, we used optogenetics to enhance or disrupt this synchrony by stimulating prefrontal PV interneurons in the two hemispheres in a coordinated or uncoordinated manner. In both cases, we stimulated prefrontal PV interneurons in each hemisphere at 40 Hz. However, in one case, this stimulation was aligned perfectly in sync, whereas in the other it was misaligned so as to disrupt the synchronization of gamma oscillations between the hemispheres. Whereas mice that received in-sync 40 Hz stimulation learned rule shifts normally, previously normal mice that received misaligned stimulation became perseverative, like the mutant mice described earlier. Furthermore, when we performed additional experiments using the mutant mice described earlier, only perfectly in-sync 40 Hz stimulation improved their rule shift learning; misaligned stimulation failed to do so.
By showing that the same rhythmic stimulation can elicit opposing effects (inducing versus rescuing perseveration) depending on whether it is precisely synchronized or misaligned, these two studies definitively established a key role for synchronization of gamma-frequency activity in cognition (at least in mice). Several other studies in rodents that have used rhythmic optogenetic stimulation support this idea. For example, boosting prefrontal gamma-frequency activity can improve the performance of normal mice on an attention task (34) and rescue abnormal social behavior in a mouse model of autism (35). Modulating the amplitude of gamma oscillations in the amygdala using precisely timed optogenetic stimulation can bidirectionally affect the consolidation of appetitive spatial memories (36). And optogenetically perturbing gamma oscillations that normally spread from the entorhinal cortex to the hippocampus impair the ability of rats to find rewards using object- or location-based cues (37).
Three other studies have used various interventions to rescue behavior in mice that model the 22q11 microdeletion. This microdeletion is among the most highly penetrant risk factors for neurodevelopmental disorders, including schizophrenia and autism. In two of these studies, manipulations that rescued performance in cognitive tasks also normalized deficits in gamma oscillations (38, 39). In the other study, gamma synchrony between the hippocampus and prefrontal cortex increased, although this increase did not quite reach statistical significance (40). Thus, while these studies did not focus on the role of gamma oscillations, they are consistent with the implications of our studies: that restoring gamma oscillations may be sufficient to rescue cognitive deficits relevant to those present in schizophrenia.
More recently, human studies have begun to explore the relationship between gamma oscillations and interventions that improve cognition in schizophrenia. One study found that transcranial direct current stimulation (tDCS) that improves cognitive control also increases prefrontal task-evoked gamma power (41). Another found that changes in gamma power during auditory steady-state responses predicted improvements in positive and negative symptoms elicited by targeted cognitive training (42).
While a large body of evidence now indicates that gamma oscillations can causally influence cognition and behavior, it is not yet clear exactly how gamma oscillations influence neuronal information processing in ways that contribute to brain function. There are many hypotheses about these potential functions (30). Gamma oscillations were originally hypothesized to contribute to consciousness by binding together information in disparate parts of the brain to form a coherent percept (43), but this idea has since fallen out of favor both because of a lack of experimental support and because of concerns about its biological plausibility (44). One popular hypothesis, dubbed “communication through coherence,” posits that by synchronizing activity across upstream and downstream regions, gamma oscillations cause output from the upstream region to arrive in downstream regions when circuit inhibition is near its trough, maximizing the responsiveness of the downstream region (45). By synchronizing neural activity, gamma oscillations may concentrate synaptic output into narrow windows of time, allowing that output to summate more effectively (46), increasing the gain and reducing the variability of responses in downstream neurons (5). Synchronized gamma oscillations may also create conditions that enable neural circuits to update the information stored in working memory (47).
Cortical Microcircuit Organization
If enhancing gamma oscillations, particularly in the frontal cortex, can lead to powerful, and possibly enduring, improvements in cognitive deficits associated with schizophrenia, then it is logical to develop therapeutics that can harness these therapeutic effects. At this point, it is important to appreciate the details of the cortical microcircuits from which gamma oscillations emerge, and upon which they act. The term “microcircuit” is generally used to refer to a canonical pattern of organization, whereby different types of neurons are interconnected in a characteristic manner.
As mentioned earlier, there are many subtypes of inhibitory neurons that express the neurotransmitter GABA in the cortex. The three major subdivisions of these cortical interneurons are based on the expression of specific proteins such as PV, but these various classes also have other differences that likely contribute to their ability to perform distinct circuit functions. For example, PV interneurons classically comprise two major subtypes: the majority are “basket cells,” whereas a smaller fraction are “chandelier cells.” Both subtypes have characteristic “fast-spiking” electrophysiological properties, that is, they have ion channels that rapidly repolarize their membrane potential following action potentials. This limits the inactivation of voltage-gated sodium channels, enabling these neurons to fire at very high rates without slowing down (giving rise to their fast-spiking moniker). Basket cells are so called because they target the perisomatic region of excitatory neurons; thus, their axonal processes appear to form “baskets” around these excitatory cell bodies. Basket cells are also connected to each other with both chemical and electrical synapses (i.e., gap junctions), but tend not to inhibit other classes of inhibitory neurons (48–50). The combination of interconnections, perisomatic inhibition, and fast-spiking properties is thought to make basket cells particularly well suited for generating gamma oscillations (51–53). Whereas basket cells target the perisomatic region of excitatory neurons, chandelier cells target the axon initial segments of excitatory neurons, thus giving their axonal processes a chandelier-like appearance.
Another major class of cortical inhibitory neurons is defined by expression of the neuropeptide somatostatin (SST). Within this class, a major subtype are Martinotti cells, which, in contrast to both basket and chandelier cells, target the distal apical dendrites of cortical pyramidal neurons. Because PV and SST interneurons tend to target, respectively, the cell body and the distal dendrites, they produce fundamentally different types of inhibition. PV interneurons tend to hyperpolarize the soma, moving it further away from the spike threshold, whereas SST interneurons tend to increase the leakiness of regions of the dendrites that directly receive excitatory inputs, “shunting” these inputs and making them decay more rapidly. These subtly different effects can lead to profound differences in how these two classes of interneurons affect information processing by excitatory neurons. For example, PV interneurons tend to produce “subtractive” inhibition, which suppresses strong and weak responses equally, whereas SST interneurons tend to produce “divisive” inhibition, which disproportionately suppresses stronger responses (54, 55). SST interneurons also tend to inhibit PV interneurons (even though the converse is not true) (48–50). A third subtype of cortical interneurons, identified by expression of vasoactive intestinal polypeptide (VIP), tend not to inhibit excitatory neurons, but rather tend to inhibit SST interneurons (which also inhibit them back) (50, 56). As a result, activating VIP interneurons reduces circuit inhibition and can enhance responses to incoming input (57).
In the preceding discussion, “cortical GABAergic neurons” and “interneurons” are often referred to interchangeably. This terminology is based on a now outdated assumption that cortical GABAergic neurons give rise to projections that are confined to the local circuit. However, it is now known that some GABAergic neurons, including those in the prefrontal cortex, can project over long distances, sending output to other brain structures, even beyond the cortex (58, 59). Thus, gamma oscillations may be transmitted and synchronized across regions by long-range inhibitory connections originating from PV “interneurons.”
The preceding discussion also refers to cortical excitatory neurons as if these were a homogeneous group. In fact, it is now known that the excitatory pyramidal neurons within a cortical region differ, largely based on 1) the layer in which they are located and 2) the downstream targets of their axons (60). These various classes of pyramidal neurons also differ in their morphology (e.g., having thin or thick apical dendritic tufts), their electrophysiological properties (e.g., the presence of ionic currents that promote resonance at particular frequencies), and the expression of neuromodulatory receptors (e.g., dopamine D1 versus D2 receptors) (61, 62). Most strikingly, they differ in their connectivity. Different classes of pyramidal neurons have different patterns of intracortical connectivity (63) and receive different forms of input (64), enabling them to play distinct roles in local circuit computations. In particular, PV interneurons more strongly inhibit some classes of pyramidal neurons than others (64). This suggests that when PV interneurons generate gamma oscillations, these oscillations may be transmitted more strongly to certain classes of pyramidal neurons. For example, in the prefrontal cortex, layer 5 pyramidal neurons that project to subcortical targets such as the mediodorsal thalamus tend to have thick apical tufts and prominent hyperpolarization-activated currents, express dopamine D2 receptors, receive nondepressing callosal inputs, and are strongly inhibited by nearby PV interneurons. By contrast, a distinct subpopulation of layer 5 pyramidal neurons that projects across the corpus callosum tends to have thin apical tufts and minimal hyperpolarization-activated currents, express dopamine D1 receptors, receive rapidly depressing callosal inputs, and are more weakly inhibited by nearby PV interneurons.
How Can We Leverage Knowledge of Cortical Microcircuits to Advance New Therapies?
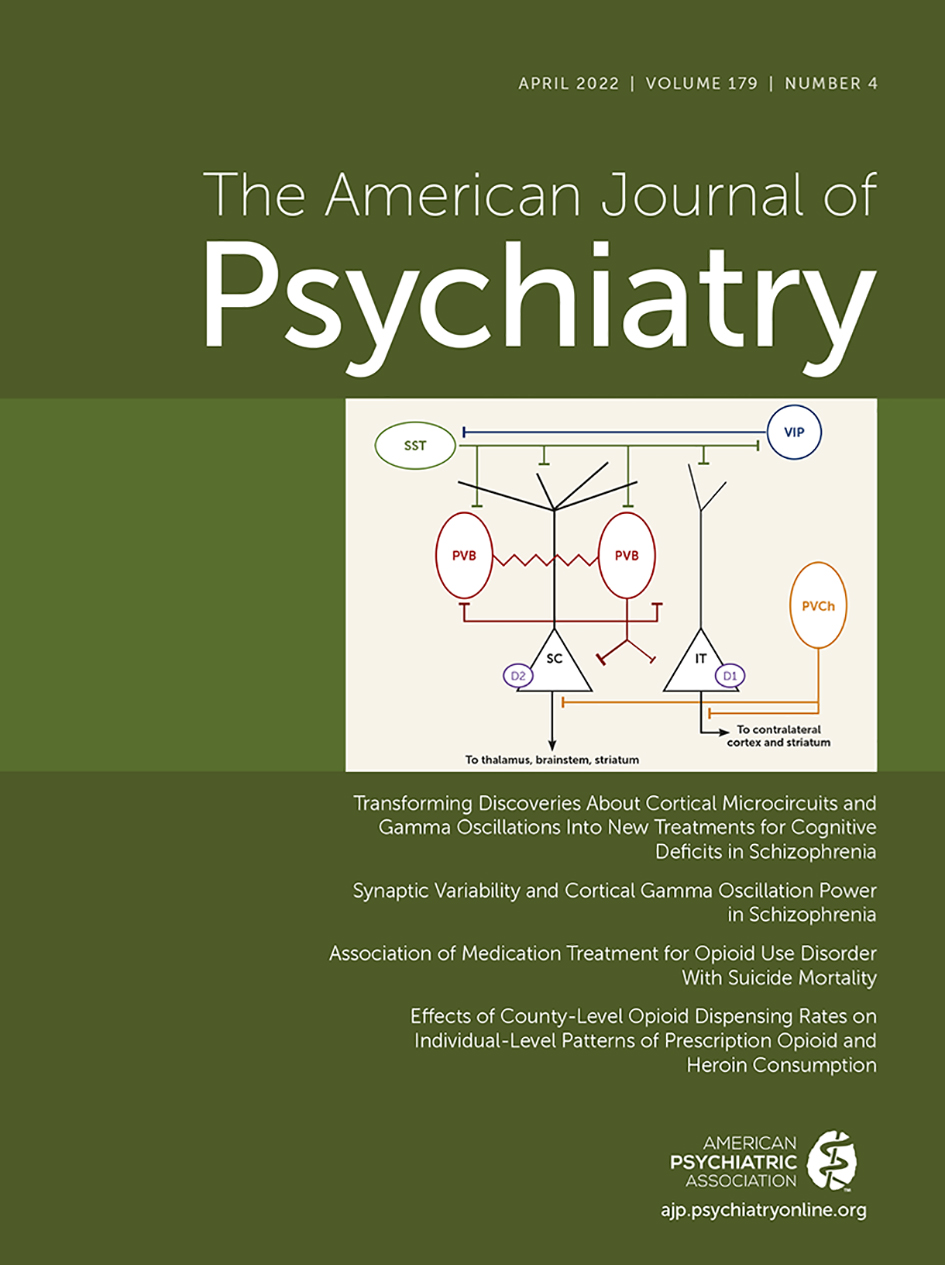
Papers discussing possible mechanisms underlying neuropsychiatric disorders, especially schizophrenia and autism, often invoke the “excitation-inhibition (E/I) ratio” or “excitation-inhibition (E-I) balance.” But as the preceding discussion hopefully makes clear, neither excitation nor inhibition is a unitary quantity. Rather, there are many types of excitatory and inhibitory neurons, each of which has a distinctive pattern of synaptic connectivity and intrinsic electrophysiological properties that enable it to play a unique role in information processing and circuit function. Furthermore, each of these possesses a characteristic complement of neuromodulatory receptors, endowing it with an idiosyncratic sensitivity to pharmacological manipulation. In this context, the cortical microcircuit represents a schematic wiring diagram, summarizing the different cell types and their characteristic patterns of connectivity within local cortical circuits (Figure 1). For example, in prefrontal cortex, PV interneurons more strongly inhibit subcortically projecting than do callosally projecting pyramidal neurons in layer 5. These PV interneurons also inhibit each other and are interconnected by gap junctions. PV interneurons receive inhibition from SST interneurons, which also inhibit and are inhibited by VIP interneurons. Taking this microcircuit into consideration, there may be many ways to achieve the end goal of enhancing gamma-frequency synchronization in a specific population of pyramidal neurons. These might include potentiating excitatory synapses onto PV interneurons, making PV interneurons more excitable, enhancing GABAergic synapses from PV interneurons onto pyramidal neurons, and targeting any neuromodulatory receptors on this specific population of pyramidal neurons that might enhance their tendency to synchronize with gamma-frequency inhibitory input. For example, we previously found that activating specific serotonin receptors on PV interneurons increases their responsiveness to gamma-frequency input (65).

FIGURE 1. Schematic of key cell types and inhibitory connections within cortical microcircuitsa
a In panel A, for simplicity, excitatory connections within cortical microcircuits are not shown, and the focus is on relationships between key cell types instead of the laminar organization of the cortex. SST=somatostatin-expressing interneuron; VIP=vasoactive intestinal polypeptide-expressing interneuron; PVB=parvalbumin-expressing basket cell; PVCh=parvalbumin-expressing chandelier cell; SC=subcortically projecting pyramidal neuron; IT=intratelencephalically projecting pyramidal neuron; D2=dopamine D2 receptor; D1=dopamine D1 receptor. PVBs inhibit the cell bodies of pyramidal neurons and other PVBs, and more strongly inhibit deep-layer pyramidal neurons that project subcortically than those that project callosally. PVBs also inhibit themselves via autaptic connections, and are coupled to other PVBs via electrical synapses (gap junctions). SST interneurons provide inhibition to the apical dendrites of pyramidal neurons, and also inhibit PVBs and VIP interneurons. VIP interneurons primarily inhibit SST interneurons. PVChs mainly inhibit the axon initial segments of pyramidal neurons. Subcortically projecting (SC) pyramidal neurons have thick apical dendritic tufts and express dopamine D2 receptors, whereas intratelencephalically projecting (IT) pyramidal neurons have thin dendritic tufts and express dopamine D1 receptors. As shown in panel B, within the cortical microcircuit, interactions between PVBs and pyramidal neurons are believed to generate gamma oscillations. Excitation from 1) local pyramidal neurons and 2) external sources excite PVBs, causing them to inhibit 3) pyramidal neurons, 4) other PVBs, and 5) (via autaptic connections) themselves. Gap junctions form electrical synapses between 6) PVBs, helping to synchronize their activity. When synaptic inhibition from PVBs wears off, pyramidal neurons are able to re-excite PVBs, and PVBs are once again receptive to excitation from both local and external sources, allowing a new cycle of the oscillation to begin. Many of these elements, including excitatory inputs onto PVBs, the intrinsic properties of PVBs, and inhibitory synaptic output from PVBs onto pyramidal neurons, are believed to be abnormal in schizophrenia, potentially contributing to deficits in gamma oscillations.
To evaluate these various possibilities, we must first understand the cortical microcircuitry from which gamma synchrony emerges. As described earlier, gamma oscillations are known to be paced and synchronized by synaptic inhibitory currents. However, PV interneurons elicit inhibitory currents both in downstream pyramidal neurons and in other PV interneurons (and potentially in long-range targets). Furthermore, as noted above, even among pyramidal neurons, the strength of inhibitory currents elicited by PV interneurons differs for different subtypes (corresponding to pyramidal neurons that project to different targets). And individual PV interneurons not only inhibit neighboring PV interneurons, they actually also make very strong synaptic connections onto themselves (“autapses”), and these could also potentially synchronize gamma oscillations (66). Thus, as a starting point, we should endeavor to discover which of these synaptic loci is most important for promoting gamma oscillations. Similarly, we might find that the critical information processing functions of gamma oscillations derive from their ability to synchronize firing in a specific class of pyramidal neurons, suggesting that GABAergic synapses from PV-expressing basket cells onto this class of pyramidal neurons are a critical target.
One way to target GABAergic synapses onto a particular class of neurons is to exploit the fact that GABAA receptors on different cell types are composed of distinct combinations of subunits. For example, GABAA receptors often differ in their alpha subunit composition, and these alpha subunits vary in their sensitivity to benzodiazepine-like compounds. This explains why, for example, newer hypnotics such as zolpidem and eszopiclone have different effects than classical benzodiazepines (67). Zolpidem and eszopiclone have relatively greater affinity for alpha1-containing GABAA receptors that promote sedating and amnestic effects, and relatively decreased affinity for the alpha2-, alpha3-, and alpha5-containing receptors that produce anxiolysis and myorelaxation.
Another promising avenue comes from the observation from our laboratory and others that in mutant mice that model aspects of schizophrenia, transient interventions can lead to long-lasting improvements in gamma synchrony and cognition (32, 33, 39). It may be possible to identify the specific cellular and synaptic loci that undergo enduring plasticity as a result of these interventions. Then it may be possible to identify treatments that trigger, enhance, or mimic this plasticity.
A proof of concept for this sort of translational approach comes from the novel therapeutic brexanolone, which was recently approved for the treatment of postpartum depression. Studies in a mouse model of postpartum depression found disruptions in specific GABAA receptors, which contain the delta subunit and are responsible for tonic inhibitory currents (68). These disruptions were secondary to changes in neurosteroid levels during and following pregnancy, and countering them using a delta subunit–specific GABAergic agonist could ameliorate abnormal postpartum phenotypes in these mice. Brexanolone targets specific GABAA receptors, enhancing these same tonic inhibitory currents (69). Thus, identifying the critical synaptic loci within the cortical microcircuit that were compromised in an animal model of a postpartum depression–like state helped lead to a clinically effective drug that acts on these loci with at least some degree of specificity.
Thus, suppose we find that gamma-frequency synchronization of a specific population of prefrontal pyramidal neurons plays a key role in enhancing information processing and circuit computations that are important for aspects of cognition that are disrupted in schizophrenia. We could use the sort of computational model presented by Chung and colleagues in this issue (70) to incorporate the microcircuit abnormalities that are known to occur in schizophrenia, and predict how well various types of interventions would restore gamma synchrony in this targeted class of pyramidal neurons. This type of approach might help us determine whether it would be most effective to target neuromodulatory receptors coupled to specific ion channels in these pyramidal neurons, AMPA versus NMDA receptors on PV interneurons, or GABAA receptor alpha subunits found in synapses between PV interneurons versus those found in synapses from PV interneurons onto a specific class of pyramidal neurons.
Assume we are able to use knowledge of cortical microcircuits to identify promising candidate interventions in this way. Then we might measure how these interventions affect gamma oscillations in individuals performing cognitive tasks, to validate that they do indeed elicit the intended effect. In fact, it may one day be possible to link specific changes in gamma oscillations, for example, reduced amplitude versus altered frequency versus attenuated long-range synchronization, with specific microcircuit alterations in order to predict what types of interventions would be most likely to rescue gamma synchrony and improve cognition in a particular individual. Furthermore, there is no reason to assume that these interventions should be limited to pharmacology. It might be possible to administer a drug that enhances the capacity for a circuit to generate gamma synchrony with a behavioral intervention such as cognitive training, meditation, or biofeedback, or noninvasive brain stimulation (e.g., tDCS) to enhance gamma oscillations. Similar to what we observed in mutant mice, enhancing gamma synchrony during the performance of cognitive tasks might engender long-lasting improvements in circuit function and cognition.
Outlook and Next Steps
It is now clear that gamma synchronization contributes to the function of brain circuits in ways that could be highly relevant for treating cognitive deficits in conditions such as schizophrenia. Furthermore, the complexity of cortical microcircuits may turn out to be a major asset (not a barrier) to developing these treatments, by enabling us to target particular aspects of gamma synchrony in a relatively specific manner. Achieving these translational goals will require us to address the following outstanding questions.
We have summarized schizophrenia-associated abnormalities in the gamma oscillations evoked by sensory stimulation and in the gamma oscillations elicited by cognitive tasks. Are both sets of abnormalities indicative of common changes at the level of microcircuits—for example, PV interneuron dysfunction—or do they reflect distinct mechanisms? Are both of these phenomena equally relevant for schizophrenia, that is, should we be trying to boost gamma oscillations throughout the brain (e.g., using pharmacology), or should we focus specifically on enhancing frontal gamma oscillations during cognitive tasks (e.g., using targeted brain stimulation or neurofeedback)?
Will strategies that rescue gamma synchrony and cognition in mice translate to individuals with schizophrenia? For example, we found that a subsedative and subanxiolytic dose of the benzodiazepine clonazepam rescues deficits in gamma synchrony and cognition in mutant mice that model aspects of schizophrenia, and that optogenetically enhancing gamma synchrony elicits persistent improvements in these mice (32, 33). Another study found that dopamine D2 receptor antagonists such as haloperidol, given in late adolescence, can persistently rescue deficits in PV interneuron function, gamma oscillations, and cognition in mice that model the 22q11 microdeletion (39). There are reasons to be optimistic and pessimistic about the prospect, suggested by mouse studies, that individual interventions might elicit such persistent improvements. On the one hand, the Prevention Through Risk Identification, Management, and Education study examined the effects of antipsychotic treatment in patients who have prodromal symptoms of psychosis and are believed to be at risk for developing schizophrenia. The trial found that treating this group of patients with olanzapine may transiently mask their psychotic symptoms but does not elicit persistent improvements in their clinical outcomes (71). By contrast, the study from O’Keeffe and colleagues in this issue (72) suggests that shortening the duration of untreated psychosis has beneficial effects on symptoms and functioning that endure for >20 years, supporting the idea that therapeutic interventions delivered early on may be able to elicit enduring benefits. As we seek to produce these kinds of long-lasting improvements in individuals with schizophrenia, we must keep in mind that aberrant circuitry in the human brain does not (in most cases) reflect a single highly penetrant genetic disruption, but is likely to be multifactorial, reflecting the interaction between multiple genetic, developmental, and environmental processes unfolding over decades. This suggests that successfully treating cognitive deficits in schizophrenia may require remediation across multiple levels, achieved by interventions that target multiple complementary mechanistic processes, possibly through different modalities of treatment.
PV interneuron dysfunction and deficits in gamma synchrony have been hypothesized to possibly result from other pathogenic processes, for example, excessive synaptic pruning (73) or hippocampal hyperactivity (74). If reductions in gamma synchrony are downstream consequences of the loss of synapses due to excessive pruning, or PV interneuron dysfunction following hippocampal hyperactivity, might the reverse also be true? That is, might (persistently) restoring inhibitory neuron-drive gamma oscillations create a network state that is favorable for synaptic plasticity, helping lead to a broader restoration of brain function? This represents one hypothesis for how transient interventions can elicit long-lasting therapeutic effects in the mouse studies described above.
Although we have established that gamma synchrony does contribute to brain function and behavior, the exact mechanisms through which it does so remain unknown. For example, are gamma oscillations acting to enhance communication between brain regions, or to facilitate certain types of computations within a brain region, or to create circuit dynamics that are favorable for the plasticity of specific synapses, etc.? Identifying the detailed mechanisms through which gamma oscillations contribute to brain function will help to elucidate exactly how we should aim to enhance gamma synchrony in order to improve cognition. For example, understanding whether gamma oscillations contribute to cognition by enhancing information processing within local cortical circuits versus promoting interregional communication might provide clues about whether we should optimize our therapies to enhance the amplitude of gamma oscillations at specific sites versus their synchronization across long distances.
In summary, there is now ample evidence that gamma synchrony plays an important role in the aspects of cognition that are impaired in schizophrenia. Nevertheless, the detailed relationships between specific cellular and synaptic loci within cortical microcircuits and pathological or therapeutic changes in gamma synchrony remains unclear. Elucidating these relationships may reveal potent and highly selective approaches for harnessing gamma synchrony to remediate the cognitive deficits that are the major cause of disability in schizophrenia and related conditions.
1. : Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 2006; 67(Suppl 9):3–8; discussion 36–42Medline, Google Scholar
2. : Developing treatments for impaired cognition in schizophrenia. Trends Cogn Sci 2012; 16:35–42Crossref, Medline, Google Scholar
3. : Mechanisms underlying dorsolateral prefrontal cortex contributions to cognitive dysfunction in schizophrenia. Neuropsychopharmacology 2022; 47:292–308Crossref, Medline, Google Scholar
4. : Cortical gamma band synchronization through somatostatin interneurons. Nat Neurosci 2017; 20:951–959Crossref, Medline, Google Scholar
5. : Parvalbumin neurons and gamma rhythms enhance cortical circuit performance. Nature 2009; 459:698–702Crossref, Medline, Google Scholar
6. : Driving fast-spiking cells induces gamma rhythm and controls sensory responses. Nature 2009; 459:663–667Crossref, Medline, Google Scholar
7. : Three groups of interneurons account for nearly 100% of neocortical GABAergic neurons. Dev Neurobiol 2011; 71:45–61Crossref, Medline, Google Scholar
8. : Gene expression deficits in a subclass of GABA neurons in the prefrontal cortex of subjects with schizophrenia. J Neurosci 2003; 23:6315–6326Crossref, Medline, Google Scholar
9. : Cortical deficits of glutamic acid decarboxylase 67 expression in schizophrenia: clinical, protein, and cell type-specific features. Am J Psychiatry 2011; 168:921–929Link, Google Scholar
10. : Altered parvalbumin basket cell terminals in the cortical visuospatial working memory network in schizophrenia. Biol Psychiatry 2021; 90:47–57Crossref, Medline, Google Scholar
11. : Lower gene expression for KCNS3 potassium channel subunit in parvalbumin-containing neurons in the prefrontal cortex in schizophrenia. Am J Psychiatry 2014; 171:62–71Link, Google Scholar
12. : Gamma frequency-range abnormalities to auditory stimulation in schizophrenia. Arch Gen Psychiatry 1999; 56:1001–1005Crossref, Medline, Google Scholar
13. : Steady state visual evoked potential abnormalities in schizophrenia. Clin Neurophysiol 2005; 116:614–624Crossref, Medline, Google Scholar
14. : Gamma band oscillations reveal neural network cortical coherence dysfunction in schizophrenia patients. Biol Psychiatry 2006; 60:1231–1240Crossref, Medline, Google Scholar
15. : Sensory-evoked gamma oscillations in chronic schizophrenia. Biol Psychiatry 2008; 63:744–747Crossref, Medline, Google Scholar
16. : 40-Hz auditory steady-state responses characterize circuit dysfunctions and predict clinical outcomes in clinical high-risk for psychosis participants: a magnetoencephalography study. Biol Psychiatry 2021; 90:419–429Crossref, Medline, Google Scholar
17. : Abnormal neural synchrony in schizophrenia. J Neurosci 2003; 23:7407–7411Crossref, Medline, Google Scholar
18. : Whole-brain source-reconstructed MEG-data reveal reduced long-range synchronization in chronic schizophrenia. eNeuro 2017; 4:1–14.
19. : EEG findings of reduced neural synchronization during visual integration in schizophrenia. PLoS One 2015; 10:e0119849Crossref, Medline, Google Scholar
20. : Evidence for dysregulated high-frequency oscillations during sensory processing in medication-naïve, first episode schizophrenia. Schizophr Res 2013; 150:519–525Crossref, Medline, Google Scholar
21. : Transient induced gamma-band response in EEG as a manifestation of miniature saccades. Neuron 2008; 58:429–441Crossref, Medline, Google Scholar
22. : Response to: Yuval-Greenberg et al, “Transient induced gamma-band response in EEG as a manifestation of miniature saccades.” Neuron 58, 429–441. Neuron 2009; 62:8–10Crossref, Medline, Google Scholar
23. : Reduced oscillatory gamma-band responses in unmedicated schizophrenic patients indicate impaired frontal network processing. Clin Neurophysiol 2004; 115:1863–1874Crossref, Medline, Google Scholar
24. : Dysfunctional prefrontal gamma-band oscillations reflect working memory and other cognitive deficits in schizophrenia. Biol Psychiatry 2015; 77:1010–1019Crossref, Medline, Google Scholar
25. : Impairments in frontal cortical gamma synchrony and cognitive control in schizophrenia. Proc Natl Acad Sci USA 2006; 103:19878–19883Crossref, Medline, Google Scholar
26. : Gamma oscillatory power is impaired during cognitive control independent of medication status in first-episode schizophrenia. Neuropsychopharmacology 2010; 35:2590–2599Crossref, Medline, Google Scholar
27. : Cortical oscillatory activity is critical for working memory as revealed by deficits in early-onset schizophrenia. J Neurosci 2009; 29:9481–9489Crossref, Medline, Google Scholar
28. : GABA level, gamma oscillation, and working memory performance in schizophrenia. Neuroimage Clin 2014; 4:531–539Crossref, Medline, Google Scholar
29. : Neural oscillations and synchrony in brain dysfunction and neuropsychiatric disorders: it’s about time. JAMA Psychiatry 2015; 72:840–844Crossref, Medline, Google Scholar
30. : How close are we to understanding what (if anything) γ oscillations do in cortical circuits? J Neurosci 2016; 36:10489–10495Crossref, Medline, Google Scholar
31. : Snapshots of the brain in action: local circuit operations through the lens of γ oscillations. J Neurosci 2016; 36:10496–10504Crossref, Medline, Google Scholar
32. : Gamma rhythms link prefrontal interneuron dysfunction with cognitive inflexibility in Dlx5/6(+/-) mice. Neuron 2015; 85:1332–1343Crossref, Medline, Google Scholar
33. : Cross-hemispheric gamma synchrony between prefrontal parvalbumin interneurons supports behavioral adaptation during rule shift learning. Nat Neurosci 2020; 23:892–902Crossref, Medline, Google Scholar
34. : Prefrontal parvalbumin neurons in control of attention. Cell 2016; 164:208–218Crossref, Medline, Google Scholar
35. : Gamma oscillation dysfunction in mPFC leads to social deficits in neuroligin 3 R451C knockin mice. Neuron 2018; 97:1253–1260.e7Crossref, Medline, Google Scholar
36. : Closed-loop control of gamma oscillations in the amygdala demonstrates their role in spatial memory consolidation. Nat Commun 2019; 10:3970Crossref, Medline, Google Scholar
37. : Gamma rhythm communication between entorhinal cortex and dentate gyrus neuronal assemblies. Science 2021; 372:eabf3119Crossref, Medline, Google Scholar
38. : Restoring wild-type-like CA1 network dynamics and behavior during adulthood in a mouse model of schizophrenia. Nat Neurosci 2018; 21:1412–1420Crossref, Medline, Google Scholar
39. : Long-lasting rescue of network and cognitive dysfunction in a genetic schizophrenia model. Cell 2019; 178:1387–1402.e14Crossref, Medline, Google Scholar
40. : Developmental inhibition of Gsk3 rescues behavioral and neurophysiological deficits in a mouse model of schizophrenia predisposition. Neuron 2016; 89:1100–1109Crossref, Medline, Google Scholar
41. : Using prefrontal transcranial direct current stimulation (tDCS) to enhance proactive cognitive control in schizophrenia. Neuropsychopharmacology 2020; 45:1877–1883Crossref, Medline, Google Scholar
42. : Gamma oscillations predict pro-cognitive and clinical response to auditory-based cognitive training in schizophrenia. Transl Psychiatry 2020; 10:405–410Crossref, Medline, Google Scholar
43. : Temporal binding and the neural correlates of sensory awareness. Trends Cogn Sci 2001; 5:16–25Crossref, Medline, Google Scholar
44. : Synchrony unbound: a critical evaluation of the temporal binding hypothesis. Neuron 1999; 24:67–77, 111–125Crossref, Medline, Google Scholar
45. : Rhythms for cognition: communication through coherence. Neuron 2015; 88:220–235Crossref, Medline, Google Scholar
46. : Correlated neuronal activity and the flow of neural information. Nat Rev Neurosci 2001; 2:539–550Crossref, Medline, Google Scholar
47. : Gamma and beta bursts underlie working memory. Neuron 2016; 90:152–164Crossref, Medline, Google Scholar
48. : Two networks of electrically coupled inhibitory neurons in neocortex. Nature 1999; 402:75–79Crossref, Medline, Google Scholar
49. : A network of fast-spiking cells in the neocortex connected by electrical synapses. Nature 1999; 402:72–75Crossref, Medline, Google Scholar
50. : Inhibition of inhibition in visual cortex: the logic of connections between molecularly distinct interneurons. Nat Neurosci 2013; 16:1068–1076Crossref, Medline, Google Scholar
51. : Synchronized oscillations in interneuron networks driven by metabotropic glutamate receptor activation. Nature 1995; 373:612–615Crossref, Medline, Google Scholar
52. : Proximally targeted GABAergic synapses and gap junctions synchronize cortical interneurons. Nat Neurosci 2000; 3:366–371Crossref, Medline, Google Scholar
53. : Inhibitory coupling specifically generates emergent gamma oscillations in diverse cell types. Proc Natl Acad Sci USA 2005; 102:18638–18643Crossref, Medline, Google Scholar
54. : Activation of specific interneurons improves V1 feature selectivity and visual perception. Nature 2012; 488:379–383Crossref, Medline, Google Scholar
55. : Asymmetric effects of activating and inactivating cortical interneurons. eLife 2016; 5:e18383Crossref, Medline, Google Scholar
56. : Cortical interneurons that specialize in disinhibitory control. Nature 2013; 503:521–524Crossref, Medline, Google Scholar
57. : VIP Interneurons contribute to avoidance behavior by regulating information flow across hippocampal-prefrontal networks. Neuron 2019; 102:1223–1234.e4Crossref, Medline, Google Scholar
58. : The long and short of GABAergic neurons. Curr Opin Neurobiol 2013; 23:179–186Crossref, Medline, Google Scholar
59. : A class of GABAergic neurons in the prefrontal cortex sends long-range projections to the nucleus accumbens and elicits acute avoidance behavior. J Neurosci 2014; 34:11519–11525Crossref, Medline, Google Scholar
60. : The neocortical circuit: themes and variations. Nat Neurosci 2015; 18:170–181Crossref, Medline, Google Scholar
61. : Projection-specific neuromodulation of medial prefrontal cortex neurons. J Neurosci 2010; 30:16922–16937Crossref, Medline, Google Scholar
62. : Synaptic activity unmasks dopamine D2 receptor modulation of a specific class of layer V pyramidal neurons in prefrontal cortex. J Neurosci 2012; 32:4959–4971Crossref, Medline, Google Scholar
63. : Intracortical circuits of pyramidal neurons reflect their long-range axonal targets. Nature 2009; 457:1133–1136Crossref, Medline, Google Scholar
64. : Pyramidal neurons in prefrontal cortex receive subtype-specific forms of excitation and inhibition. Neuron 2014; 81:61–68Crossref, Medline, Google Scholar
65. : Serotonin enhances excitability and gamma frequency temporal integration in mouse prefrontal fast-spiking interneurons. eLife 2017; 6:e31991Crossref, Medline, Google Scholar
66. : Strong preference for autaptic self-connectivity of neocortical PV interneurons facilitates their tuning to γ-oscillations. PLoS Biol 2019; 17:e3000419Crossref, Medline, Google Scholar
67. : An emerging circuit pharmacology of GABAA receptors. Trends Pharmacol Sci 2018; 39:710–732Crossref, Medline, Google Scholar
68. : GABA(A)R plasticity during pregnancy: relevance to postpartum depression. Neuron 2008; 59:207–213Crossref, Medline, Google Scholar
69. : Neurosteroids as novel antidepressants and anxiolytics: GABA-A receptors and beyond. Neurobiol Stress 2019; 11:100196Crossref, Medline, Google Scholar
70. : Synaptic variability and cortical gamma oscillation power in schizophrenia. Am J Psychiatry 2022; 179:277–287Link, Google Scholar
71. : Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry 2006; 163:790–799Link, Google Scholar
72. : 20-year prospective, sequential follow-up study of heterogeneity in associations of duration of untreated psychosis with symptoms, functioning, and quality of life following first-episode psychosis. Am J Psychiatry 2022; 179:288–297Link, Google Scholar
73. : Altered ErbB4 splicing and cortical parvalbumin interneuron dysfunction in schizophrenia and mood disorders. Neuropsychopharmacology 2018; 43:2478–2486Crossref, Medline, Google Scholar
74. : Hippocampal dysfunction in the pathophysiology of schizophrenia: a selective review and hypothesis for early detection and intervention. Mol Psychiatry 2018; 23:1764–1772Crossref, Medline, Google Scholar