Using Neuroimaging to Characterize Brain Alterations Associated With Psychopathology
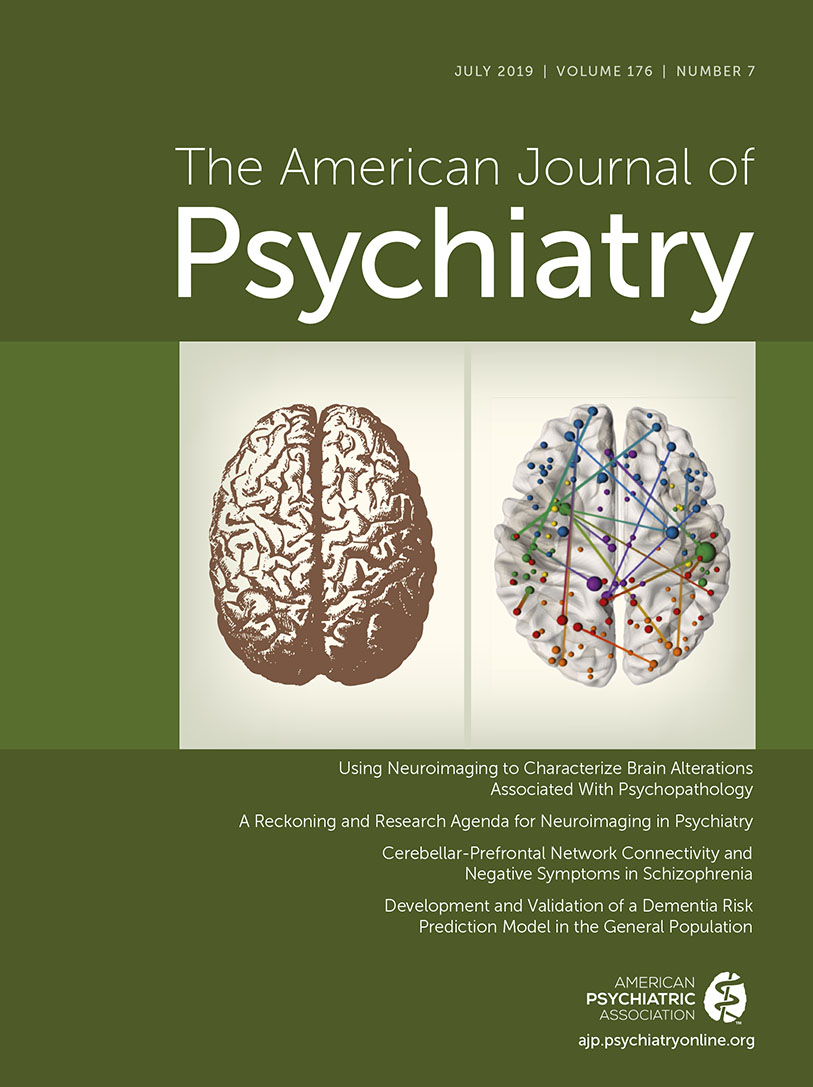
Please join me in celebrating the 175th anniversary of both APA and its official journal, the American Journal of Psychiatry. I am very grateful to have the privilege to continue to advance the outstanding tradition of the Journal and to have the opportunity to provide an overview for the Journal’s July 2019 issue—175 years after the first issue was published in July 1844. The founders of APA could never have envisioned the incredible progress we have made in understanding the brain and, in particular, its structural and functional alterations as they relate to psychiatric illness. Thus, I think it is very appropriate that 175 years later, this issue is dedicated to providing insights into psychopathology-linked brain alterations elucidated with modern neuroimaging methods. Needless to say, our capacity to monitor brain function and visualize brain structure has come a long way from methods of the past. The imaging field began with radiographs. Then, in attempting to visualize more detail within the skull, pneumoencephalography was developed, computerized tomography followed, and later came the advent of magnetic resonance imaging (MRI). Now, we use high-resolution structural and functional MRI (fMRI), as well as positron emission tomography and magnetoencephalography, combined with sophisticated data analytic and statistical approaches to investigate the neural substrates underlying the illnesses that we treat.
This issue of the Journal has, as its centerpiece, an insightful overview by Dr. Amit Etkin from Stanford University that provides a framework for thinking about the current state of MRI in relation to understanding psychiatric illnesses (1). Dr. Etkin’s research focuses on the neural underpinnings of psychopathology, and here he puts into perspective the progress the field has made in relation to neuroimaging. He discusses why earlier neuroimaging studies have not been as fruitful as was anticipated. Such issues include relatively small sample sizes and the use of a diagnostic system that likely clouds our ability to understand phenotypes that, at a neural level, may not be distinguishable with DSM-5 diagnoses. Importantly, he suggests directions for future neuroimaging work that have the potential to be more readily translatable to patient care. In this issue of the Journal, we present six original research articles that provide new and relevant insights into the neural alterations associated with schizophrenia, other psychotic disorders, attention deficit hyperactivity disorder (ADHD), and dementia. Many of the neuroimaging-related experimental design and methodological issues that Dr. Etkin raises in his overview can be found in these reports.
Using structural MRI, Lizano and coworkers (2) examine choroid plexus volume in patients with psychosis and their first-degree relatives with various diagnoses (i.e., bipolar disorder, schizophrenia, and schizoaffective disorder). The authors’ results demonstrate a transdiagnostic increase in choroid plexus volume across patients with psychosis and an association between increased choroid plexus volume and other brain structural alterations as well as measures of cognitive and immune function. The authors speculate on the meaning of these findings in relation to the role of the choroid plexus in regulating CSF production and in modulating the blood-brain barrier.
In another article using structural imaging in patients with schizophrenia with varying degrees of severity and chronicity, Wannan et al. (3) investigate alterations in cortical thickness. In addition to replicating earlier findings of schizophrenia-related cortical thinning across various regions, these authors demonstrate that the magnitude of cortical thickness reduction can be related across different areas of the cortex. This suggests that what appeared to be “irregular” alterations across the cortex are not simply sporadic but, rather, reflect how these regions may be connected to each other. Dr. Edward Bullmore, a neuropsychiatrist from the University of Cambridge and an expert in brain network organization, provides an editorial (4) on this article. Dr. Bullmore discusses these findings in the context of other work examining brain alterations in schizophrenia and explains the methods used in this article to explore structural connectivity. He raises questions about the meaning of these findings and into the mechanisms underlying the reported associations in cortical thickness reductions across different cortical regions.
Two other articles in this issue use structural imaging data: one addresses cortical alterations associated with ADHD, and another explores the utility of structural imaging metrics as a component of an algorithm to predict the development of dementia. In relation to ADHD, Hoogman and colleagues (5) use very large, multisite collaborative samples that incorporate children, adolescents, and adults with ADHD, as well as first-degree relatives and control subjects. With these large samples, the authors observe small but significant differences in cortical surface area in frontal, cingulate, and temporal cortical regions in children with ADHD. In contrast to children, these findings were not found in adolescents or adults with ADHD. This finding underscores the importance of considering developmental phase and age when conceptualizing illness-related alterations and the potential neural substrates underlying symptoms. Dr. Jay Giedd, a child and adolescent psychiatrist from the University of California, San Diego, and an expert in adolescent brain development, provides an editorial in which he puts these findings into perspective (6). He further emphasizes the importance of using these types of data to communicate, to doubters, that ADHD is a “true” illness.
The article by Licher et al. (7) is motivated by the need for improving the capacity of clinicians to predict an individual’s likelihood of developing dementia. Here, the authors ask the question as to whether structural imaging, cognitive testing, and other biological indices, such as assessment of the APOE-ε4 genotype, will improve the ability to predict the development of dementia beyond an algorithm based on standard clinical measures. By analyzing data from a large cohort, the authors conclude that the prediction of dementia over a 10-year period is significantly enhanced by the additional measures that include quantitative assessment of brain structure. In an accompanying editorial by Dr. Sterling Johnson and Dr. Sanjay Asthana (8), both dementia researchers from the University of Wisconsin, the importance of the finding is acknowledged, but the authors also emphasize the heterogeneous nature of dementia (e.g., Alzheimer’s, Pick’s, frontotemporal degeneration). Based on the different pathophysiologies of specific dementias, Johnson and Asthana underscore the need for developing selective algorithms based on state of the art, disease-specific biomarkers.
Two articles in this issue use fMRI methods in severely ill patients to better understand the neural underpinnings of social deficits, negative symptoms, and the role of cerebellar circuits. In patients with schizophrenia spectrum disorders, Hawco and coworkers (9) use hierarchical clustering methods to demonstrate various patterns of neural responsivity to tasks involving imitating and observing different facial expressions of emotion. By using this fMRI data–driven approach, the researchers find that, in the affected individuals studied, these different patterns of neural activity are predictive of social and neurocognitive scores. This article demonstrates the potential utility of an approach that uses fMRI to define neural heterogeneity in a meaningful way that is not revealed by our current diagnostic system.
Finally, in a very innovative study, Brady et al. (10) used fMRI to assess resting-state functional connectivity in a group of patients recently diagnosed with schizoaffective disorder and schizophrenia. After using a data-driven approach, this group found that decreased functional connectivity between the dorsolateral prefrontal cortex and the midline cerebellum was associated with individual differences in negative symptoms. Moving beyond the correlational analyses that are typical of most imaging studies, the authors tested whether modulation of this circuit predictably affected negative symptoms. Using transcranial magnetic stimulation applied to the midline cerebellar region, Brady and coworkers demonstrated the ability to increase functional connectivity between the cerebellum and prefrontal cortex. Remarkably, this increase in functional coupling was associated with an improvement in negative symptoms. Dr. Hengyi Cao and Dr. Tyrone Cannon, researchers from Yale University focused on understanding psychotic disorders, write an insightful commentary on these findings and provide a historical perspective in relation to altered cerebellar function in schizophrenia (11). They also suggest the possibility that these new findings with regard to negative symptoms could be mediated by neuronal projections from deep cerebellar nuclei to dopaminergic neurons involved in prediction error processing.
We are grateful for the contributions the authors and commentators made to this issue. These articles use state of the art neuroimaging and analytic strategies to uncover novel findings relevant to understanding brain alterations associated with psychopathology. We look forward to future studies from these research groups, and others, that will clarify how findings like these can be used to develop treatment-relevant diagnostic strategies that improve upon our current diagnostic schema and methods. Such brain-based, data-driven approaches also have the potential to direct the development of more specific and effective treatments focused on altering the structure and function of distinct neural targets. The advances in our science, and in our field in general, would have been unimaginable to our founders 175 years ago. And yet, with all of these advances, we still have a long way to go to meet our commitment to significantly improving the lives of many of our patients who continue to suffer from the complex and, at times, devastating illnesses that we treat.
1 : A reckoning and research agenda for neuroimaging in psychiatry. Am J Psychiatry 2019; 176:507–511Link, Google Scholar
2 : Association of choroid plexus enlargement with cognitive, inflammatory, and structural phenotypes across the psychosis spectrum. Am J Psychiatry 2019; 176:564–572Link, Google Scholar
3 : Evidence for network-based cortical thickness reductions in schizophrenia. Am J Psychiatry 2019; 176:552–563Link, Google Scholar
4 : Cortical thickness and connectivity in schizophrenia (editorial). Am J Psychiatry 2019; 176:505–506Link, Google Scholar
5 : Brain imaging of the cortex in ADHD: a coordinated analysis of large-scale clinical and population-based samples. Am J Psychiatry 2019; 176:531–542Link, Google Scholar
6 : The enigma of neuroimaging in ADHD (editorial). Am J Psychiatry 2019; 176:503–504Link, Google Scholar
7 : Development and validation of a dementia risk prediction model in the general population: an analysis of three longitudinal studies. Am J Psychiatry 2019; 176:543–551Link, Google Scholar
8 : Predicting risk for dementia: is it ready for the clinic? (editorial). Am J Psychiatry 2019; 176:501–502Link, Google Scholar
9 : Separable and replicable neural strategies during social brain function in people with and without severe mental illness. Am J Psychiatry 2019; 176:521–530Link, Google Scholar
10 : Cerebellar-prefrontal network connectivity and negative symptoms in schizophrenia. Am J Psychiatry 2019; 176:512–520Link, Google Scholar
11 : Cerebellar dysfunction and schizophrenia: from “cognitive dysmetria” to a potential therapeutic target (editorial). Am J Psychiatry 2019; 176:498–500Link, Google Scholar